- Submissions

Full Text
Integrative Journal of Conference Proceedings
Identification of Drug Therapy Problem in Adult Hypertensive Patients in A Nigerian Tertiary Hospital
Ukoha-kalu blessing O*, Adibe Maxwell O and Ukwe Chinwe V
Department of Clinical Pharmacy and Pharmacy Management, Faculty of Pharmaceutical Sciences, University of Nigeria, Nigeria
*Corresponding author: Ukoha-kalu blessing O, Department of Clinical Pharmacy and Pharmacy Management, Faculty of Pharmaceutical Sciences, University of Nigeria, Nigeria
Submission: September 12, 2020;Published: September 23, 2020

Volume2 Issue3September, 2020
Abstract
Background: An event involving drug therapy that actually or potentially interferes with the desired health outcomes is known as drug therapy problem.
Objective: The study aimed to identify drug related problems encountered by hypertensive patients receiving care in a Nigeria Tertiary Hospital.
Methods: This study was a retrospective analysis of the medical records of Adult hypertensive patients. A total of 171 patient folders were used for the study. The data were collected from the patients’ medical records using the Pharmaceutical Care Network Europe (PCNE) Classification tool Version 6.2 (PCNE, 2010). For each of the 171 medical records, the DTPs experienced within the study period were identified. The demographic information such as age and gender were recorded. Other items documented were the drugs implicated in the therapy problems, type of drug therapy problem, cause of drug therapy problem (DTP), type of intervention and the outcome of intervention. Data were analyzed using the IBM Statistical Product and Service Solutions (SPSS) for Windows, Version 21.0 (IBM Corp, Version 21.0, and Armonk, NY, USA).
Results: Majority of the patients were above 65years of age 64(37.4%), while about half of the patients were females. Also, most of the patients were traders 62(36.3%), 146(85.4%) were married, 146(79.1%) were Christians by religion and 164(95.9%) were currently non-smokers as at the time of the study. It was also found that approximately 53.2% of the patients suffered from two or more diseases. The most common hypertension co morbid disease was congestive heart failure 41(23.9%) followed by Diabetes mellitus (31.1%). In this study the average number of anti-hypertension medications prescribed per patient was 1.58 ± 0.69 with minimum of one and maximum of four. Most patients were on two combined therapy 66(38.6%), 75(43.9%) were on three combined therapy and only 10(5.8%) were on monotherapy. Amlodipine was most commonly prescribed 90(52.6%) followed by losartan 75(43.9%). The total number of drug related problem found was 193 which 60 (31.1%) were noncompliance. Unnecessary drug treatment was the least type of drug therapy problem encountered.
Conclusion: The prevalence of drug therapy problems among hypertensive patients was high. Presence of co-morbidity increase number of medication and age were associated with an increase in drug therapy problem. Increased drug therapy problem can lead to increase in complications, increased hospital stay, emergency hospitalization and increased medical cost.
Keyword: Hypertension; Drug therapy Problem; Antihypertensives
Introduction
An event involving drug therapy that actually or potentially interfers with the desired health outcomes is known as drug therapy problem [1]. Hypertension is the most common cardiovascular disease recorded in Africa. In a surveyed carried out in 2011, hypertension was in 42% of African adults [2]. This prevalence varies with age, race, education [2]. Also, about 70% of adults will develop hypertension by the age of 80 [3]. Analysis of the global burden of hypertension revealed that over 26% of the world’s adult population had hypertension in 2000, and there has also been a rapid increase in prevalence affecting significant numbers of individuals in Sub-Saharan Africa [4]. Studies worldwide indicate that despite the availability of effective medical therapy, more than half of hypertensive patients on treatment have blood pressures over 140/90mm Hg threshold [5]. This is mostly because of drug therapy problems which include but not limited to non-compliance, ADRs, improper drug selection and drug interactions. The occurrence of a DTP among hypertensive patients could prevent or delay patients from achieving desired therapeutic goals [6]. It has been attributed to unnecessary over-prescription of drugs, substantial worsening of diseases, avoidable increases in hospital admission rates, and longer hospital stays leading to a significant medical burden [7]. As a result, substantial numbers of patients do not get the maximum benefit of medical treatment, resulting in poor health outcomes, lower quality of life, increased health care costs and erodes public confidence in health systems [8].
Objective
The objective of this study was to identify drug related problems encountered among adult hypertensive patients receiving care in a Nigerian Tertiary Hospital
Methods
Study design: This was a retrospective analysis of the medical records of Adult hypertensive patients receiving care in a tertiary hospital in Enugu state, Nigeria, within a 3-year period (January 1, 2015- December 31, 2018).
Ethical committee approval: Ethical approval was obtained from the Health Research and Ethics Board of the University of Nigeria Teaching Hospital (UNTH), Ituku-Ozalla, Enugu State (NHREC/05/01/2008BFWA00002458- 1RB00002323) before commencement of the study Eligibility criteria: All folders of hypertensive outpatients who received prescription from the hospital within the study period.
Sample size calculation: All folders that fell within the eligibility criteria were utilized for the study. A total of 171 patient folders were used.
Data collection: The data were collected from the patients’ medical records using the Pharmaceutical Care Network Europe (PCNE) Classification tool Version 6.2 (PCNE, 2010). For each of the 171 medical records, the DTPs experienced within the study period were identified. The demographic information such as age and gender were recorded. Other items documented were the drugs implicated in the therapy problems, type of drug therapy problem, cause of drug therapy problem (DTP), type of intervention and the outcome of intervention. The PCNE V 6.2 has 4 primary domains for problems, 8 primary domains for causes and 5 primary domains for interventions. On a more detailed level, there are 9 grouped subdomains for problems, 37 grouped sub-domains for causes and 17 grouped sub-domains for interventions. The sub-domains are explanatory for the principal domains.
Data analysis: Data were analyzed using the IBM Statistical Product and Service Solutions (SPSS) for Windows, Version 21.0 (IBM Corp, Version 21.0, and Armonk, NY, USA).
Results
Majority of the patients were above 65years of age 64(37.4%), while about half of the patients were females. Also, most of the patients were traders 62(36.3%), 146(85.4%) were married, 146(79.1%) were Christians by religion and 164(95.9%) were currently non-smokers as at the time of the study [Table 1]. It was also found that approximately 53.2% of the patients suffered from two or more diseases. The most common hypertension co morbid disease was congestive heart failure 41(23.9%) followed by Diabetes mellitus (31.1%) [Table 2]. The total number of drug related problem found was 193 which 60 (31.1%) were noncompliance. Unnecessary drug treatment was the least type of drug therapy problem encountered [Table 3]. The major cause of drug related problem was patient related factors which account 64(37.4%) of drug related problem. These include patients refusing to take their drugs or patients abruptly stopping their medications [Table 4]. Marital status (p=0.000), number of drugs (P=0.00) and number of co-morbid (P=0.000) are associated with increased drug therapy problems. Drug therapy problems increase as age increase (P=0.00) and smoking status (P=0.000) significantly affect DTP. Religion (P=1.000), gender (P=0.963) and employment (P=0.321) were not associated with increased DTP [Table 5].
Table 1: Demographic characteristics.
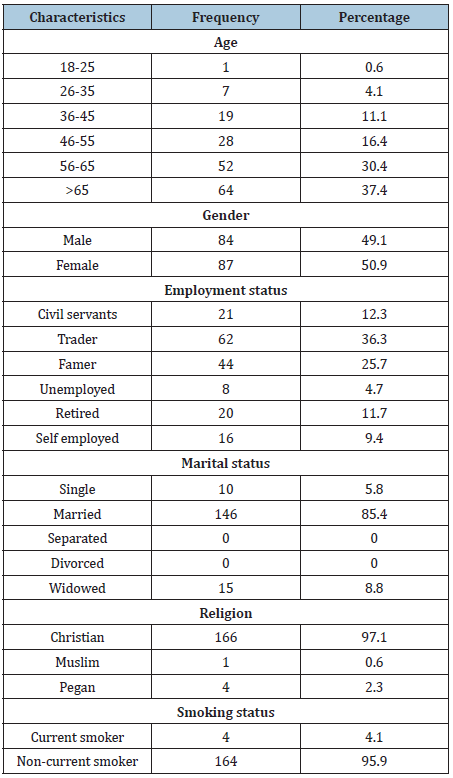
Table 2: Presence of co-morbidity.
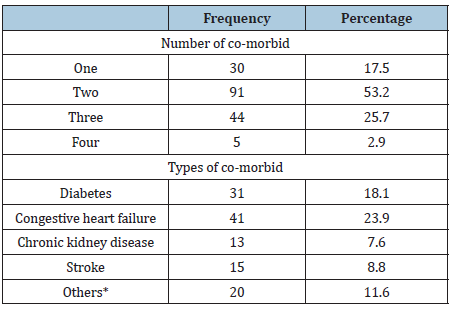
Others* acute kidney disease=5, cardiovascular disease=6, ulcer=9.
Table 3: Types of drug related problem.
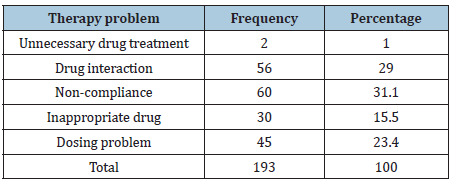
Table 4: Cause of drug related problem.
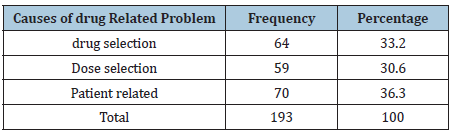
Table 5: Association between DRP and patients demographics & other factors.

*P < 0.05.
Discussion
In this study, a total of 193 drug therapy problems was identified in 171 folders. The most common DRP identified was noncompliance. According to this study the result shown that ARB (losartan), lisinopril and aspirin caused drug interaction the more. Other studies reported that beta blockers were the main cause of drug-drug interaction followed by ACE inhibitor and this difference may be due to the variation in commonly prescribed medications [9,10]. The data obtained from patient’s folder revealed the proportion of treatment non-compliance was high showing that a large proportion of patients found in the hospital do not adhere to their medications. Marital status, number of medications and number of co-morbidity significantly affect DRP. This could be because majority of the single patients were younger in age and so may have less or no co-morbid conditions. Increase in the number of co-morbid conditions a patient has will invariably lead to an increase in the number of medications the patient will be taken. Similar studies also recorded that increase in the number of drug leads to an increase in the drug therapy problem a patient might experience [11-13]. Majority of the drug therapy problems recorded were among the married population. This is in agreement with other studies which revealed that married people tend to have a lot of responsibilities and financial burden which makes them to stop taking their medications as a result of their inability to afford these drugs [14,15].
Conclusion
The prevalence of drug therapy problems among hypertensive patients was high. Presence of co- morbidity increase number of medication and age were associated with an increase in drug therapy problem. Increased drug therapy problem can lead to increase in complications, increased hospital stay, emergency hospitalization and increased medical cost.
References
- Aguwa CN, Nworu CS (2012) Hypertension. In: Aguwa CN (Ed.), (4th edn), Therapeutic basis of clinical pharmacy in the tropics. Snaap Press Nigeria limited, Nigeria, pp. 88-90.
- Andros V, Egger A, Dua U (2006) Blood pressure goal attainment according to JNC 7 guidelines and utilization of antihypertensive drug therapy in MCO patients with type 1 or type 2 diabetes. J Manag Care Pharm 12(4): 303-309.
- Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, et al. (2008) Treatment of hypertension in patients 80 years of age or older. N Engl J Med 358(18): 1887-1898.
- Gudina EK, Michael Y, Assegid S (2013) Prevalence of hypertension and its risk factors in southwest Ethiopia: a hospital-based cross-sectional survey. Integr Blood Press Control 6: 111-117.
- Gobezie T, Belay Y, Yesuf EA, Gelaw BK, Defesha AD (2014) Drug therapy problem among patients with cardiovascular disease in felege hiwot referral hospital, NE, Ethiopia. International Journal of Pharmacy Teaching and Practice 5(3): 989-996.
- Katzung BG, Trevor AJ (2015) Basic and clinical pharmacology. Antihypertensive agents, McGraw-Hill Education, USA, pp. 169-187.
- Husseia M, Likisa J, Woldu MA, Tegegne GT, Umeta GT (2014) Assessment of drug related problem among hypertensive patients on follow up in adama hospital medical college, east Ethiopia 3(2): 1-6.
- Mahmud MA (2013) Drug therapy problems and quality of life in patients with chronic kidney disease. Int J Res Med Sci 1: 74-85.
- Mandavi, D’Cruz S, Sachdev A, Tiwari P (2012) Adverse drug reactions & their risk factors among Indian ambulatory elderly patients. Indian J Med Res 136: 404-410.
- Perterson C, Gustafsson M (2017) Characterization of drug related problem and associated factors at clinical pharmacy-naïve hospital in northern part of sweeden. Drugs Real World Outcomes: 4(2): 97-107.
- Rosendorff C, Black HR, Cannon CP, Gersh BJ, Gore J (2007) Treatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the America heart association council for high blood pressure research and the councils on clinical cardiology and epidemiology and prevention. Circulation 113(9): e435-e470.
- Redzuan AM, Ramali AR, Pheng MT (2017) Drug related problem hypertensive patients with comorbidities 1(3): 1-8.
- Trevisol DJ, Moreira LB, Fuchus FD, Fuchs SC (2012) Health-related quality of life is worse in individuals with hypertension under drug treatment: Results of population based study. J Hum Hypertens 26(3): 374-380.
- Bemt PM, Egberts TC, Berg LT (2014) Drug-related problems in hospitalized patients. Drug Safety 22(4): 321-333.
- Yone De Almeida, Carvalho WS, de Assis FA (2009) Drug related problems observed in pharmaceutical care service in belo horizonte, Brazil. Brazilian Journal of Pharmaceutical Sciences 45(2): 321-330.
© 2020 Ukoha-kalu blessing O. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






