- Submissions

Full Text
Gastroenterology Medicine & Research
Rendez-vous Approach to Segmental Biliary Disconnection after Liver Transplantation
Bourguignon Arnaud¹, Nisolle Marie-Laure², Tannouri Fadi¹, Lemmers Arnaud³ and Devière Jacques³*
1Department of Radiology, Belgium
2Department of Anesthesiology, Belgium
3Department of Gastroenterology and Hepatopancreatology, Erasme Hospital, Free University of Brussels, Brussels, Belgium
*Corresponding author:Devière Jacques, Department of Gastroenterology and Hepatopancreatology, Erasme Hospital, Free University of Brussels, Brussels, Belgium
Submission:July 17, 2023;Published: August 01, 2023

ISSN 2637-7632Volume7 Issue4
Abstract
Introduction: Selected cases of complete common bile duct transection can be successfully treated using
a combined endoscopic/transhepatic approach. Intrahepatic segmental exclusions are more challenging
and such combined approach for repermeabilization has not been reported so far.
Case presentation: A 44-year-old woman with a past history of liver transplantation and ischemic
cholangitis presented a hilar stricture involving both sides with a passable stricture on the left side
(Amsterdam type C) and a complete blockage on the right side, excluding segments V and VIII (Amsterdam
type D). We present here the management of these lesions: first was managed endoscopically and the
second by percutaneous/endoscopic rendez-vous technique.
Conclusion: Intrahepatic biliary reconnection is feasible, but more difficult than common bile duct
reconnection and benefits from using multiple guidance modalities.
Keywords:Liver transplantation; Biliary stricture; Segmental biliary disconnection; Rendez-vous technique
Introduction
Biliary tract lesions are well-known complications after liver transplantation [1] and may result in bilomas, external leaks, stenoses, biliary peritonitis, and sepsis. The Bismuth- Strasberg classification and the Amsterdam classification are frequently used to classify biliary tract injuries [2-5]. Treatment of these lesions involves endoscopic procedures (sphincterotomy, dilatation, stenting, internal transmural drainage), surgical procedures (suture, reimplantation, external drainage), and interventional (transhepatic drainage) approaches. Complete blockage of segmental bile ducts represents a severe complication that often requires surgical revision. Complete biliary transection, usually considered a surgical indication, has been successfully treated using a combined endoscopic/transhepatic approach in selected cases [6,7], and may be facilitated by using endoscopic and percutaneous cholangioscopy [8]. Multi-technique, non-surgical approaches have been proposed for severe complications after liver surgery, but management of segmental occlusion associated with ischemic cholangitis after orthotopic liver transplantation (OLTx) has not, to our knowledge, been reported so far.
Case
A 44-year-old woman with a past history of liver transplantation 3 years before (fulminant auto-immune hepatitis) presented with multiple episodes of cholangitis and sepsis secondary to a hilar stricture involving both sides with a passable stricture on the left side (Amsterdam type C) and a complete blockage on the right side, excluding segments V and VIII (Amsterdam type D) (Figure1a). Initial management consisted of an endoscopic retrograde biliary drainage (ERBD) to dilate and stent the left side of the liver from which the right posterolateral segments arose. No opacification of the remaining right anteromedial segments was obtained, even after forceful injection with an occluding balloon, suggesting a complete occlusion (Figure 1b). Several recurrences of sepsis were treated with antibiotics, iterative dilatation, and replacement of the biliary prothesis. Over time, despite internal biliary drainage, an increased dilatation of the right biliary tree above the non-passable stricture was observed on follow-up Magnetic Resonance Imaging (MRI). Considering this, and the fact that the clinical situation of the patient was becoming worse despite adequate endoscopic drainage of the accessible segments (left and right (postero-lateral)), the decision was made to perform a percutaneous drainage of the isolated right antero-medial segments. Transhepatic passage of a guidewire to the Common Bile Duct (CBD) was not achievable and simultaneous endoscopic and transhepatic opacifications demonstrated a > 1cm gap between the two structures (Figure 1c), making a cholangioscopic approach (with transillumination) challenging. After two unsuccessful attempts of recanalization according to the rendez-vous technique, surgical alternatives, including a possible new hepatic transplantation, were considered. After Multidisciplinary Team (MDT) discussion and with the patient’s consent, the decision was made to proceed with a new attempt at recanalization using a rendez-vous technique and intrahepatic puncture, as has been previously described for common bile duct transection [8].
Figure 1:(a) Cholangiogram demonstrating biliary tree dilatation,
(b) Forceful injection during cholangioscopy.
(c) Transhepatic opacification demonstrating the stenosis of left hepatic duct and complete occlusion of the right
hepatic duct.
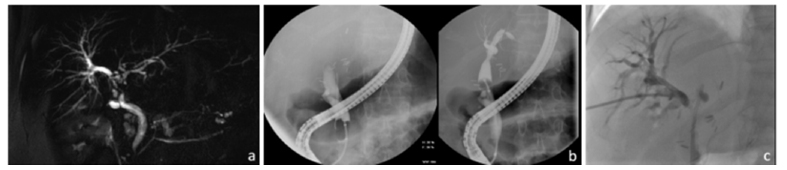
Figure 2:Fluoroscopic procedure including endoscopic retrograde cholangiopancreatography and transhepatic
approaches.
(a) Needle sheath bulging in the common bile duct wall.
(b) Internal-external drainage by ring catheter after rendez-vous technique.
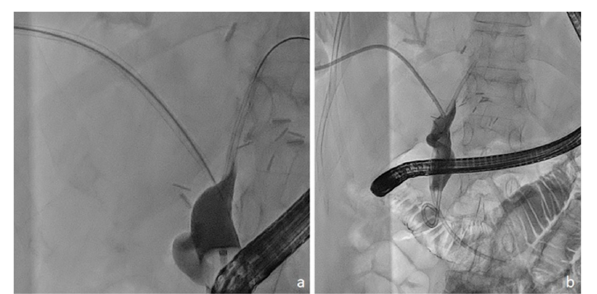
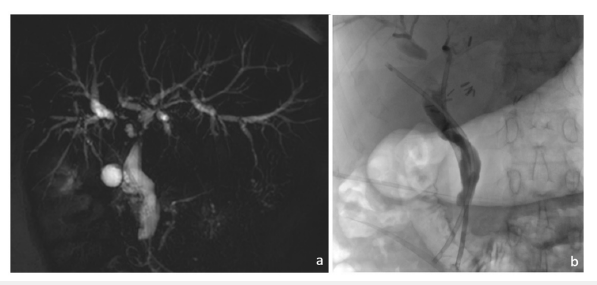
The procedure was performed under general anaesthesia by two experienced gastroenterologists, including one who performed an Endoscopic Retrograde Cholangiopancreatography (ERCP), and two interventional radiologists, including one who performed ultrasound guidance of the needle. An Amplatz guidewire (Boston Scientific – USA) was left in the antero-medial segment and, after dilation with an 11Fr bougie, a TIPSSI set (Cook – Belgium) was inserted, as previously described [6]. Multiple punctures were performed without being able to reach the CBD despite Ultrasound (US) guidance. Using an Azurion fluoroscopy table (Koninklijke Philips N.V. - Amsterdam) that allowed multiple incidences by the rotation of the C-arm and combined US guidance, it was possible to identify the axis of the track from the Intra-Hepatic Ducts (IHD) to the CBD and puncture was ultimately obtained using a 18G trocar stylet passed through the 5Fr catheter with visualization of its imprint (before deploying the inner stylet) on the endoscopically opacified CBD (Figure 2). The needle was then exchanged for a 0.035-inch, 4.5m long, angulated hydrophilic stiff wire (Jagwire Boston Scientific – USA) which was advanced into the duodenal lumen. It was then endoscopically captured with a 6Fr endoscopic snare (Creo Medical – Wales) and pulled back up through the endoscope while the 5Fr catheter was maintained in the biliary stump to protect it from frictional forces. An 8.5Fr multiperforated Ring catheter (Cook – Belgium) was pushed over the guidewire into the duodenal lumen and left there for biliary drainage, with side holes adjusted above and below the recanalized biliary tract portion. Repeated cholangitis episodes disappeared after the procedure. One-month follow-up MRI demonstrated a significant reduction in bi-segmental biliary dilatation. The Ring catheter was replaced 2 months later with a Münchener 10Fr percutaneous stent set (Pflugbeil – Germany) (Figure 3a) and was replaced at 6 months with two 8.5Fr 12cm Cotton plastic stents (Cook – Belgium) (Figure 3b) which will be further left in place for a 12-month calibration period (with systematic stent exchange at 6 months).
Figure 3:Follow-up.
(a) 1-month follow-up MRI demonstrating reduction of the intrahepatic biliary duct dilatation.
(b) 6-month follow-up endoscopic retrograde cholangiopancreatography with internalization of the drainage by the
withdrawal of the external drainage and the setting of plastic prothesis.
Discussion
The case presented here illustrates a difficult, multi-technique approach to a severe biliary complication occurring after OLTx, classically considered to be unamenable to non-surgical therapy, that allowed recovery without requiring possible retransplantation. Multiple cholangitis episodes, some with severe sepsis, suggested a nonpharmacological therapeutic intervention was appropriate for this patient. Exclusively endoscopic or percutaneous approaches were unlikely to allow reconnection of the two biliary segments. Although the rendez-vous technique using either puncture with a TIPssi set or under cholangioscopic guidance has been described, mainly for transections (Amsterdam grade D) affecting the CBD, the present case was clearly more complex. Indeed, the gap between the proximal and distal parts of the occlusion was long and identification of the puncture axis was difficult. Considering surgical alternatives (with associated higher morbidity), the decreasing condition of the patient, and the patient’s preference, the MDT decision was to proceed with a new attempt, despite previous technical difficulties, with the idea of improving the guidance procedure. The puncture was finally obtained after using both US guidance and multiple incidences under fluoroscopic control. Despite its complexity, the postoperative course of the procedure was uneventful and the patient was discharged after 6 days. This case illustrates the feasibility of non-surgical reconnection of isolated biliary segments secondary to ischemic cholangitis after OLTx. This type of non-surgical approach is, of course, only indicated in highly selected cases and when a surgical approach is considered hazardous and difficult or implies re-transplantation. Working in an experienced multidisciplinary environment is a prerequisite for such an approach. In this case, it was made easier by the availability of multiple guidance techniques (in this case the use of multiple fluoroscopic incidences and US). Future perspectives include image fusion (e.g., fluoroscopy and CT), allowing the addition of a 3-D volume to the fluoroscopy, and Cone-Beam Computed Tomography (CBCT) guidance which allows planification of the puncture route and its visualization in every incidence allowing a real-time adjustment. Post-contrast administration images or CBCT are also feasible and may provide a more precise identification of the biliary and vascular structures.
Conclusion
“When plumbing saves a liver” could have been the title of this case report which illustrates the benefit of a multi-technique and multidisciplinary approach to a difficult biliary occlusion in the setting of OLTx. Intrahepatic biliary reconnection is feasible, but more difficult than CBD reconnection due to the length of the gap and the different axes of biliary segments, and benefits from using multiple guidance modalities.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Brookmeyer CE, Bhatt S, Fishman EK, Sheth S (2022) Multimodality imaging after liver transplant: Top 10 important complications. Radiographics 42(3): 702‑7
- Nordin A, Grönroos JM, Mäkisalo H (2011) Treatment of biliary complications after laparoscopic cholecystectomy. Scand J Surg 100(1): 42‑4
- Strasberg SM, Hertl M, Soper NJ (1995) An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 180(1): 101‑1
- Bismuth H, Majno PE (2001) Biliary strictures: Classification based on the principles of surgical treatment. World J Surg 25(10): 1241‑124
- Martínez-Mier G, Medina G, los S, Luna O, Hernández N, et al. (2017) Factors associated with adverse outcomes after surgical repair of bile duct injury. J Gastroenterol Res 1(2).
- Dumonceau JM, Baize M, Devière J (2000) Endoscopic transhepatic repair of the common hepatic duct after excision during cholecystectomy. Gastrointest Endosc 52(4): 540‑54
- Bergman JJ, van den Brink GR, Rauws EA, de Wit L, Obertop H, et al. (1996) Treatment of bile duct lesions after laparoscopic cholecystectomy. Gut 38(1): 141‑14
- Ratone JP, Caillol F, Marx M, Hoibian S, Dahel Y, et al. (2022) A novel case of biliary common bile duct reconstruction by the rendezvous technique using endoscopic cholangioscopy and percutaneous cholangioscopy. Endoscopy 54(S 02): E950‑E95
© 2023 Devière Jacques. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






