- Submissions

Full Text
Gastroenterology Medicine & Research
Association Between Quality of Life and Dietary-Medical Factors in Individuals with Inflammatory Bowel Disease
Alejandra Parada Daza1,2*, Álvaro Reyes Ponce3 and Carolina Pávez Ovalle4
1Department of Nutrition, Diabetes and Metabolism, Faculty of Medicine, Pontificia Universidad Católica de Chile, Santiago, Chile
2UDA- Health Sciences, Nutrition and Dietetics Career, Faculty of Medicine, Pontificia Universidad Católica de Chile, Santiago, Chile
3Faculty of Rehabilitation Sciences, Andrés Bello University, Viña del Mar, Chile
4Department of Gastroenterology, School of Medicine, Pontificia Universidad Católica de Chile, Santiago, Chile
*Corresponding author: Alejandra Parada Daza, Department of Nutrition, Diabetes and Metabolism, Faculty of Medicine, UDA- Health Sciences, Nutrition and Dietetics Career, Faculty of Medicine, Pontificia Universidad Católica de Chile, Santiago, Chile
Submission:January 3, 2023;Published: January 12, 2023

ISSN 2637-7632Volume7 Issue3
Abstract
Background: The quality of life in individuals with inflammatory bowel disease is variable. This
study evaluated the association between quality of life and dietary-medical factors in individuals with
inflammatory bowel disease during confinement by COVID 19 in Chile.
Methods: online surveys of quality of life, diet and pharmacological aspects of the disease were applied
to adults with inflammatory bowel disease.
Results: 364 people were surveyed. The average quality of life score of the whole group was low (4.71
points), for Crohn’s disease was 4.64 points and for ulcerative colitis was 4.73 points. The quality of life
is low and worsens when there is a crisis of the disease. Dietary and pharmacological factors have a
negative impact on quality of life.
Conclusion: the quality of life in patients with inflammatory bowel disease is low and worsens when
there is a crisis of the disease.
Keywords:Ulcerative colitis; Crohn disease; Inflammatory bowel disease; Quality of life; Diet
Introduction
Inflammatory Bowel Disease (IBD) is a group of pathologies characterized by chronic and uncontrolled inflammation of the intestine, including Crohn’s Disease (CD) and Ulcerative Colitis (UC). People with IBD present a dysregulation of the innate and adaptive immune response that affects the gut with periods of crisis and remission [1]. Treatment has focused on nonspecific anti-inflammatory and immunosuppressive therapies with varied results [2]. For IBD patients point of view, diet is considered as important as pharmacological treatment, because many foods increase gastrointestinal symptoms, decrease Quality of Life (QoL) and alter nutritional status [3]. The objective of this study is to evaluate the association between QoL and dietary-medical factors in individuals with IBD during periods of crisis and remission of the quarantine disease decreed for COVID 19 in Chile.
Methods
Participants
In this cross-sectional study, individuals with IBD were convocated to participate in a survey posted online in the Carlos Quintana Crohn Colitis Ulcerosa Foundation website, this is a Chilean organization for IBD. The survey was available online during May 2020, which corresponded to the first lockdown period in Chile. The inclusion criteria were: 1) diagnosis of IBD (Crohn’s disease and ulcerative colitis), 2) older than 15 years. Before starting the survey, all participants read and signed the informed consent online. This survey was approved by the Ethic Committee of the Pontificia Universidad Católica de Chile. The study protocol complies with the ethical guidelines of the Declaration of Helsinki.
Questionnaires
The questionnaires were a) sociodemographic and general health history, b) problems associated with the diet and medical treatment, and c) quality of life. The QoL survey of IBD (IBDQ-32) translated and validated into Spanish by Maschas et al. [4] was applied. This survey includes 32 questions, responses to every question were scored on a 7-point scale where 7 is the best and 1 the poorest perceived QoL.
Statistical analysis
The results are presented as percentage, mean and standard deviation. The Shapiro-Wilk test was used to test the normality assumption. The Chi-square test was used to determine the association between categorical variables. A significant result was set at p<0.05. Statistical analyses were performed with STATA15.1
Results
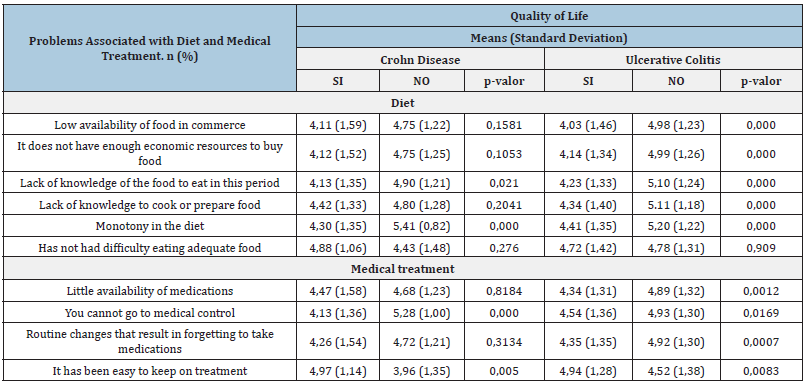
Four hundred and sixty-two individuals with IBD answered the survey and 369 of them met the inclusion criteria. 75% were women and 25% men and the age of diagnosis was 29.26 years (SD: 10.5). 70.2% and 25.5% were in remission and crisis, respectively. The most frequently reported pharmacological treatments for CD were biological (14%), immunomodulator (21%), and 5ASA (20%). The quality of life was significantly lower during the crisis period than during the remission period (Table 1). Regarding problems related to feeding, the question that obtained the highest percentage of response was “monotony in feeding”, with 66% for CD and 57% for UC, and to the problems related to medical treatment, was “not being able to attend medical check-ups”, with 58% for CD and 55% for UC. UC patients report greater problems than CD patients in relation to diet and medical treatment. These problems have an impact on the quality of life (Table 2).
Table 1:General characteristics of people with inflammatory bowel disease.
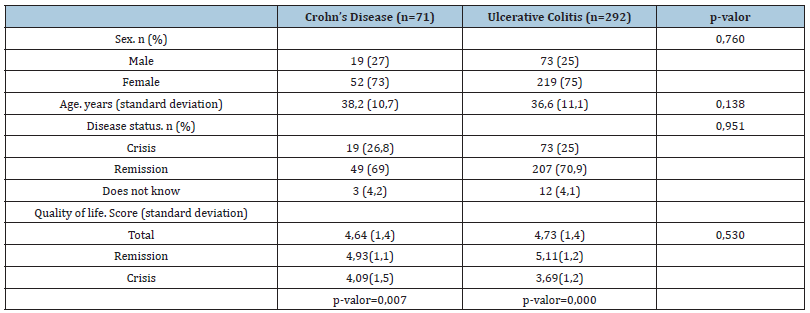
Table 2:Association between Quality of life and problems with diet and medical treatment for Crohn’s disease and ulcerative colitis, in the COVID-19 period.
Discussion
This study shows that the QoL in Chilean patients with IBD is lower than that reported in other groups that have used this survey [4]. Moreover, QoL is lower when there is a crisis than the remission period, for CD and UC. In a pandemic, the QoL in IBD can be altered by periods of confinement or by the difficulty in attending medical appointments. However, Azzam et al. showed that in people with IBD from Saudi Arabia, there were no significant differences in QoL in the pre-and post-COVID-19 pandemic period [5]. Problems associated with feeding are present in CD and UC. However, when analyzing these problems according to the state of the disease, a higher frequency of feeding problems is observed in UC in crisis. Knowledge of diet can improve QoL [6,7]. Moreover, there is evidence that inadequate food intake can alter the nutritional status and the immune system, and this is associated with an increased risk of infections in patients with IBD [8]. All patients with IBD report problems related to medical treatment. Factors such as not attending medical appointments and suspension of face-to-face consultations are described as difficult for these patients. Fortunately, the evidence shows an increase in telephone and telemedicine care in the world [9] would improve the QoL of patients.
The results of this study highlight that problems related to diet and drug treatment worsen the quality of life in UC. One of the reasons is the suboptimal drug treatment these patients receive. When analyzing the drugs, it is observed that UC patients that use corticosteroids have a lower QoL score than the rest of the patients (3.93 points vs 4.81 points, with a p-value < 0.000 (Data not shown)) One explanation for these results is because patients who use corticosteroids have active disease or suboptimal management of their disease [10]. This study has limitations including a small sample size and lack of a control group, as well as potential confounders not related to diet and drugs about quality of life. However, it is the first study in Chilean IBD.
Conclusion
In conclusion, the QoL in Chilean patients with IBD is low and worsens when there is a crisis of the disease, especially in individuals with UC. In addition, dietary and pharmacological factors have a negative impact on QoL.
Conflict of Interest
The authors declare that they have no conflict of interest.
Acknowledgment
The participation of the Carlos Quintana Crohn Colitis Ulcerosa Foundation, the Chilean organization for Inflammatory Bowel Disease.
Funding
This work had no funding.
References
- Baumgart D, Carding S (2007) Inflammatory bowel disease: Cause and immunobiology. Lancet 369(9573): 1627-1640.
- Pithadia AB, Jain S (2011) Treatment of Inflammatory Bowel Disease (IBD). Pharmacol Rep 63(3): 629-642.
- Kane S (2012) What physicians don’t know about patient dietary beliefs and behavior can make a difference. Expert Rev Gastroenterol Hepatol 6(5): 545-547.
- Masachs M, Casellas F, Malagelada JR (2007) Spanish translation, adaptation, and validation of the 32-item quality of life questionnaire (IBDQ-32) for inflammatory bowel disease. Rev Esp Enferm Dig 99(9): 511-519.
- Azzam NA, Aljebreen A, Almuhareb A, Almadi M (2020) Disability and quality of life before and during the COVID-19 outbreak: A cross-sectional study in inflammatory bowel disease patients. Saudi J Gastroenterol 26(5): 256-262.
- Fritsch J, Garces L, Quintero M, Pignac-Kobinger J, Santander A, et al. (2021) Low-fat, high-fiber diet reduces markers of inflammation and dysbiosis and improves quality of life in patients with ulcerative colitis. Clin Gastroenterol Hepatol 19(6): 1189-1199.
- Chandrasekaran A, Groven S, Lewis J, Levy S, Diamant C, et al. (2019) An autoimmune protocol diet improves patient-reported quality of life in inflammatory bowel disease. Crohns Colitis 360 1(3): otz019.
- Al-Ani AH, Prentice RE, Rentsch CA, Johnson D, Ardalan Z, et al. (2020) Review article: Prevention, diagnosis and management of COVID-19 in the IBD patient. Aliment Pharmacol Ther 52(1): 54-72.
- Lees CW, Regueiro M, Mahadevan U (2020) International organization for the study of inflammatory bowel disease. Innovation in inflammatory bowel disease care during the COVID-19 pandemic: Results of a global telemedicine survey by the international organization for the study of inflammatory bowel. Gastroenterology 159(3): 805-808.
- Lamb CA, Kennedy NA, Raine T, Hendy PA, Smith PJ, et al. (2019) British society of gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut 68(suppl 3): s1-s106.
© 2023 Alejandra Parada Daza. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






