- Submissions

Full Text
Gastroenterology Medicine & Research
Plummer Vinson Syndrome in a Severe Anemic Patient
Gabriel Constantinescu1, Alexandra Jichitu2*, Oana-Mihaela Plotogea1, Ecaterina Rinja2, Vasile Sandru2, Andreea Cristina Butuc2, Adriana Carasel2 and Madalina Stan-Ilie1
1Department of Gastroenterology, Clinical Emergency Hospital of Bucharest, Carol Davila University of Medicine and Pharmacy, 014461 Bucharest, Romania
2Department of Gastroenterology, Clinical Emergency Hospital of Bucharest, Romania
*Corresponding author:Alexandra Jichitu, Department of Gastroenterology,Clinical Emergency Hospital of Bucharest, Romania
Submission:September 23, 2022;Published: November 01, 2022

ISSN 2637-7632Volume7 Issue2
Abstract
Background:Plummer Vinson syndrome is a rare nowadays affliction that is characterized by the classical triad of dysphagia, hyposideremic anemia and esophageal webs. It is more common among middle aged women and with time it increases the risk of proximal esophagus and pharyngeal cancer. Regarding its etiology, this is still unknown and possible iron or vitamin B deficiency were incriminated. Plummer Vinson’s main characteristic is the presence of esophageal webs consisting of fibrosis, epithelial cells and chronic inflammatory elements.
Case report:A 44 years old women known with hyperthyroidism presented to the emergency room complaining of chronic progressive dysphagia. Complete blood count revealed severe hypochromic microcytic anemia and further tests showed iron deficiency. Upper digestive endoscopy was performed and esophageal webs were incriminated as the cause of dysphagia. Dilatation with Savary-Gilliard dilators was performed and iron supplementation was administered. Although additional examinations were performed in order to display the possible cause of iron deficiency, no underlying pathology was found. One-month follow up evaluation revealed no more dysphagia, no esophageal stenosis and improvement of hemoglobin levels.
Conclusion:Plummer Vinson Syndrome is a rare disease, which is caused by possible iron deficiency. Endoscopic dilatation and iron supplementation bring total symptomatology disappearance.
Keywords:Plummer vinson syndrome; Dysphagia; Esophageal webs; Anemia; Iron deficiency
Introduction
Plummer-Vinson syndrome is a rare disease that presents as the classical triad of dysphagia, esophageal webs and iron-deficiency anemia [1]. Data about its prevalence are not widely available due to the rarity of this syndrome nowadays, but most cases have been reported among middle-aged women between 40-70 years old [1]. Regarding the clinical manifestations, Plummer Vinson syndrome patients may be complaining about fatigue, tachycardia (due to the anemic syndrome) and painless, progressive and sometimes intermittent dysphagia. Clinical examination may reveal glossitis, angular cheilitis and koilonychias. Moreover, it could associate with splenomegaly or enlargement of the thyroid. We present the case of a 44 years old woman that was admitted to our clinic for total dysphagia and weight loss.
Case Report
Chief complaints
Physical examination shows a mild underweight patient with a BMI of 17.58kg/m2, koilonychias, angular cheilitis and pale teguments. Blood pressure was 128/79mmHg and heart rate was 88 beats per minute.
History of present illnes
The patient reports that symptoms were progressive and dysphagia started about 3 months ago. Firstly, dysphagia affected only solid aliments, but lately it also intermittently affects the fluids.
No menorrhagia or gastrointestinal bleeding were depicted by the patient.
History of past illness
No history of past illness
Personal and family history
She was diagnosed with Basedow disease 3 years ago and is taking 5mg of thyrozol per day since then, but she had no recent evaluation of the thyroid function.
No dietary restriction was depicted by the patient.
The patient had no family medical history or relevant genetic information.
Physical examination upon admission
On admission the patient was pale, underweight, had koilonychias and angular cheilitis. No signs of upper or lower digestive system hemorrhage were found.
Laboratory examination
Routine blood tests showed severe hypochromic microcytic anemia (hemoglobin 5g/dL, mean corpuscular volume 60μm3, mean corpuscular hemoglobin 20pg.), hyposidermia, hypoglycemia and normal values of TSH (thyroid stimulating hormone) and fT4.
Imaging examination
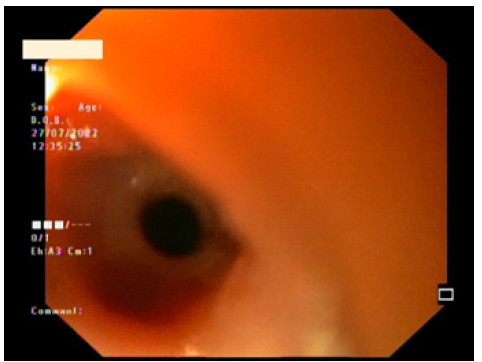
Abdomino-pelvic ultrasound showed small uterine fibroids. Ultrasound examination of the thyroid reveled normal size and structure. Upper gastrointestinal endoscopy was performed and high esophageal stenosis determined by esophageal webs was revealed. Mentzer index was calculated with a value of 16.33, which suggested deficiency anemia, so more investigations were performed in order to exclude any gastrointestinal bleeding. Colonoscopy was negative for any possible source of hemorrhage and stool was also negative for occult blood. Celiac disease, which might also be a cause of iron deficiency anemia was also excluded (Figure 1).
Figure 1: Endoscopic upper esophagus view-circumferential web.
Multidisciplinary Expert Consultation
Other causes of anemia were also ruled out after hematologic and gynecologic evaluation.
Final Diagnosis
Taking into consideration the clinical manifestation dominated by dysphagia, the endoscopic finding of esophageal webs and the biological pattern that revealed iron-deficiency anemia, the patient was diagnosed with a rare nowadays syndrome called Plummer Vinson.
Treatment
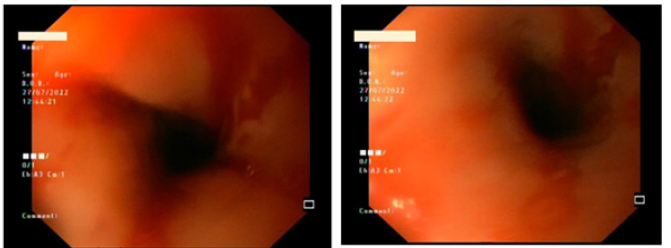
The treatment consisted of endoscopic dilatation with Savary- Gilliard dilators, transfusions of packed red blood cells and iron supplementation (Figure 2,3).
Figure 2:Endoscopic upper esophagus view-Savary-Gilliard dilatation.
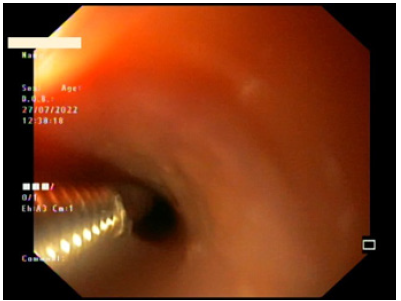
Figure 3: Endoscopic upper esophagus view-after dilatation appearance.
Outcome and Follow-Up
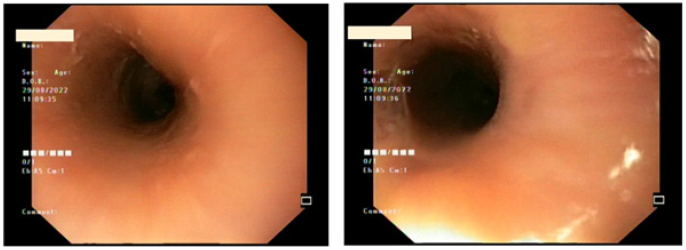
One month after the patient was discharged from our clinic, imagistic and biologic evaluation was carried out. Endoscopy showed no more esophageal webs and hemoglobin levels improved by 10g/dL. The patient was completely asymptomatic concerning the previous dysphagia (Figure 4).
Figure 4: Endoscopic upper esophagus view: one-month evaluation.
Discussion
Epidemiological data about the incidence and prevalence of Plummer Vinson Syndrome are not widely available due to its rarity. Most cases in the literature focuses on case reports. The particularity of our case was represented by the lack of symptoms regarding the anemic syndrome, the lack of any cause of iron deficiency, despite a thorough search, and the association with Basedow disease. Although the patient reported no dietary restriction, anemia was interpreted in the context of malnutrition. Data reveals that 89% of the patients with Plummer Vinson syndrome are females with mean age at presentation being 47 and our case was represented by a 44 years old female [2]. Regarding the most frequently associated pathology, celiac disease occupies the first place, closely followed by menorrhagia, hiatus hernia and chronic gastrointestinal bleeding [3-7]. Other potential associated afflictions are Crohn’s disease, rheumatoid arthritis and thyroid disorders. From this vague list of potential associated diseases, our patient had Basedow’s disease under treatment, but she had no recent endocrinological assessment. Overall prognosis of the patients that are diagnosed with Plummer Vinson syndrome is usually good with no relevant dysphagia during the follow-up period, as it was outpatient’s case too, who reported completely disappearance of the symptoms at one-month evaluation [8]. Concerning potential complications, although they are rarely reported, they must be taken into account. Esophageal webs can progressively lead to absolute dysphagia, which might be responsible for secondary aspiration pneumonia. Another possible complication is related to the symptoms of anemia, such as dyspnea, fatigue, tachycardia or even angina pectoris, therefore iron supplementation is mandatory in these patients [9]. Talking about the endoscopic treatment of the esophageal webs, it should also be taken into consideration the risk of potential esophageal perforation. Lastly, it must not be forgotten that close periodic follow-up of the patients should be done because there is a small risk of potential squamous cell cancer of the esophagus or pharynx. Follow-up studies revealed that post-cricoid carcinoma rages from 4 to 16% [10]. Moreover, there are some case reports showing there is a small association between Plummer Vinson Syndrome and gastric cancer [11].
Conclusion
To conclude, Plummer Vinson syndrome is a rare, but still existing nowadays syndrome. The main complain of the patients consists of chronic, progressive dysphagia. Although rarely described, the risk of potential esophagus and sometimes even gastric cancer, exists, so close monitoring of the patients should be taken into consideration.
References
- Wynder EL, Hultberg S, Jacobsson F, Bross IJ (1957) Environmental factors in cancer of the upper alimentary tract; a Swedish study with special reference to Plummer Vinson (Paterson-Kelly) syndrome. Cancer 10(3): 470-487.
- Kitahara S, Ohmae Y, Ogura M, Matumury Y (1999) The operation of upper esophageal web in Plummer Vinson syndrome: A case report. Auris Nasus Larynx 26(4): 495-500.
- Jani PG (2001) Plummer Vinson syndrome: Case report. East Afr Med J 78(6): 332-333.
- Makharia GK, Nandi B, Garg PK, Tandon RK (2002) Plummer Vinson syndrome: Unusual features. Indian J Gastroenterol 21(2): 74-75.
- Maleki D, Cameron AJ (2002) Plummer Vinson syndrome associated with chronic blood loss anemia and large diaphragmatic hernia. Am J Gastroenterol 97(1): 190-193.
- Rashid Z, Kumar A, Komar M (1999) Plummer Vinson syndrome and postcricoid carcinoma: Late complications of unrecognized celiac disease. Am J Gastroenterol 94(7): 1991-1910.
- Jessner W, Vogelsang H, Puspok A, Ferenci P, Gangl A, et al (2003) Plummer Vinson syndrome associated with celiac disease and complicated by postcricoid carcinoma and carcinoma of the tongue. Am J Gastroenterol 98(5): 1208-1209.
- Gottfried N (2006) Plummer Vinson syndrome. Orphanet J Rare Dis 1: 36.
- Verma S, Sandeep M (2022) Plummer Vinson Syndrome. StatPearls.
- Chisholm M (1974) The association between webs, iron and post cricoid carcinoma. Postgrad Me J 50(582): 215-219.
- Kim KH, Kim MC, Jung GJ (2005) Gastric cancer occurring in a patient with Plummer Vinson syndrome: A case report. World J Gastroenterol 11(44): 7048-7050.
© 2022 Alexandra Jichitu. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






