- Submissions

Full Text
Gastroenterology Medicine & Research
Evaluation of Knee Sport Injuries with Magnetic Resonance Images
Ana Lazarova1,2* and Antonio Gligorievski1,3
1University Clinic for Surgery St. Naum Ohridski-Skopje, R. Macedonia
2International Balkan University-Skopje, R. Macedonia
3University Goce Delcev-Stip, R. Macedonia
*Corresponding author: Ana Lazarova, University Clinic for Surgery St. Naum Ohridski-Skopje, International Balkan University-Skopje, R. Macedonia
Submission:February 17, 2022;Published: February 25, 2022

ISSN 2637-7632Volume6 Issue4
Abstract
Introduction: The knee is one of the major weights bearing joint that provides not only mobility and stability during physical activity, but also balance while standing. Sport injuries are injuries caused by sports activities and may lead to severe pain and disability. Magnetic Resonance Imaging (MRI) is established as the leading modality for noninvasive evaluation of the sports knee injuries with its multiplanar capabilities and excellent soft-tissue contrast.
The aim of the study: To investigate the accuracy of MRI in assessment of sport related knee injuries. Materials and methods: This is a prospective study which includes 50 patients with knee injuries during sport activities from period of May 2020 to September 2021. All patients came to department of traumatology at University clinic for Surgery “St. Naum Ohridski “-Skopje, and after physical examination were sent for MRI examination at the department of radiology at the same clinic. In all patients Magnetic Resonance Images (MRI) was performed at 1.5 T MR in SAG T2 weighted images, SAG Proton Density (PD) weighted images, COR STIR weighted images, COR T1 weighted images, AX PD weighted images and additional weighted images if it is needed for evaluating the anterior cruciate ligament. The results from MRI were evaluated and also compared with the results from arthroscopy or surgery.
Results: 50 patients with knee sport injuries were included in study, from them 35 male and 15 female from age of 16 to 35. Depending on the sport which cases the injury 20 patients get knee injury while preforming handball, 10 football, 7 patients during ski activities, 3 patients during running and jumping, and the rest 10 patients from bicycling and other different sport activities. Depending on the MRI results: in 33 patient lesion of Anterior Cruciate Ligament (ACL) was detected on MRI, from which 7 patients were with complete lesion and 26 were with partial lesion. 3 patients have founding of bone edema and cartilage injuries. 2 patients have retinaculum lesions, 7 patients have meniscal lesion and 5 patients were with combined injuries of meniscal lesion and lesion of ACL. With comparison of the results from MRI finding with arthroscopy or surgery findings which were taken as a gold standard we get the accuracy of MRI in 66.7% of finding the meniscal complete lesion and 85.7% of meniscal incomplete lesion. The accuracy of MRI in detection the ACL lesion was 85.7% in complete ACL lesion and 80.8% for detection the ACL partial lesion. 100% for bone edema and cartilage lesion and also 100% for retinaculum lesion.
Conclusion: MRI is noninvasive diagnostic tool with high accuracy and it is the primary approach in sport knee injuries. Thus MRI is superior to the diagnostic arthroscopy and we recommend MRI as the primary diagnostic tool for the evaluation of sports knee injuries. This study has shown total accuracy of MRI in finding the sport knee injuries at 87%, which makes it valuable noninvasive diagnostic tool for primary sport injuries.
Introduction
The knee is one of the major weights bearing joint that provides not only mobility and stability during physical activity, but also balance while standing. Sport injuries are injuries caused by sports activities and may lead to severe pain and disability [1]. Although plain radiographic films have traditionally been the first diagnostic imaging study performed in the evaluation of the painful knee, today they are useful only for evaluating joint space narrowing, alignment, and major trauma which results with bone fractures [2]. Magnetic Resonance Imaging (MRI) is established as the leading modality for noninvasive evaluation of the sports knee injuries with its multi-planar capabilities and excellent soft-tissue contrast [3]. Magnetic resonance imaging is a high accepted imaging modality in the initial diagnostic approach of patients with knee complaints. Also MRI has largely replaced diagnostic arthroscopy at this point. It is because is the top imaging and diagnostic tool for the knee joint as a result of its ability to evaluate a wide range of anatomy and pathology varying from ligamentous injuries to articular cartilage lesions [4,5]. Imaging of the knee especially for evaluation of sport injuries requires excellent contrast, high resolution, ability to visualize very small structures, multiplanar projection all of which can be provided by MR imaging. The development of advanced diagnostic MR imaging tools for the joints is of increased clinical importance has been recently shown that musculoskeletal imaging is a rapidly growing field in MR imaging applications [6]. Although arthroscopy is established as ‘‘the gold standard’’ for the diagnosis of traumatic intra-articular knee injuries, by its nature is an invasive procedure that requires hospitalization and anesthesia, thus presenting all the potential complications of a surgical procedure [7]. Over the past 20 years, since its beginning in radiology in the 80s years of the last century magnetic resonance imaging have become first-line imaging study that should be performed in the evaluation of the painful knee [8]. MRI has gained in popularity as a diagnostic tool for knee injuries. It is general opinion between surgeons that MRI is an accurate, non-invasive method to diagnose knee injuries, and gives adequate information to support decisions for conservative treatment and save the patient from unnecessary arthroscopy [9].
Materials and Methods
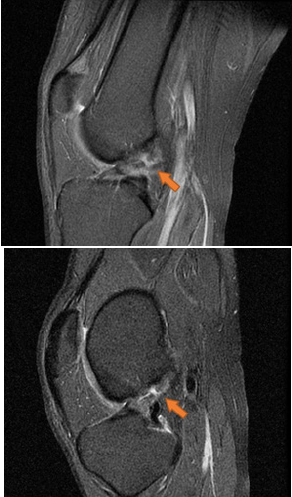
This is a prospective study which includes 50 patients with knee injuries during sport activities from period of May 2020 to September 2021.All patients came to department of traumatology at University clinic for Surgery “St. Naum Ohridski “-Skopje, and after physical examination were sent for MRI examination at the department of radiology at the same clinic. In all patients Magnetic Resonance Images (MRI) was performed at 1.5 T MR in SAG T2 weighted images, SAG Proton Density (PD) weighted images, COR STIR weighted images, COR T1 weighed images, AX PD weighed images and additional weighted images if it is needed for evaluating the anterior cruciate ligament. The results from MRI were evaluated and also compared with the results from arthroscopy or surgery (Figure 1-6).
Figure 1: MRI of knee, SAG and COR Proton Density (PD) weighted images. Incomplete lesion of posterior horn of medial meniscus.
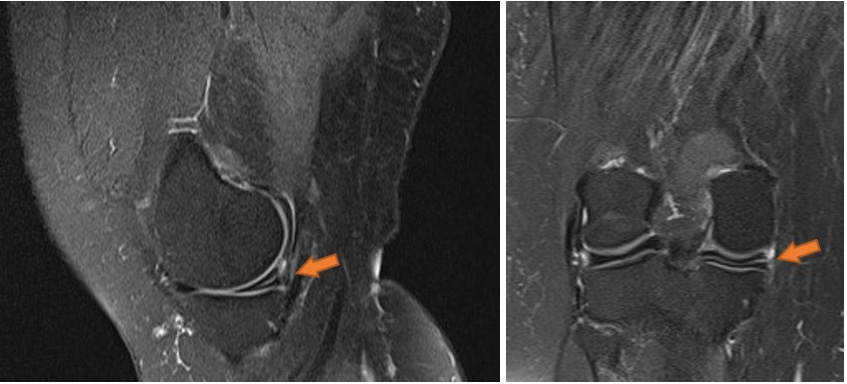
Figure 2: MRI of knee, SAG Proton Density (PD) weighted images. Complete lesion of posterior horn of medial meniscus.
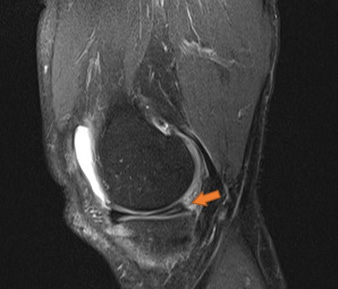
Figure 3: MRI of knee, SAG Proton Density (PD) weighted images. Bone edema on medial condyle of tibia and femur.
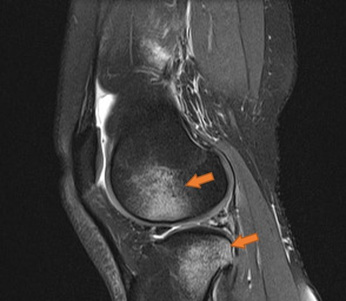
Figure 4: MRI of knee, SAG proton density (PD) weighted images. Partial lesion of ACL Gr. I.

Figure 5: MRI of knee, SAG proton density (PD) weighted images. Partial lesion of ACL Gr. II.
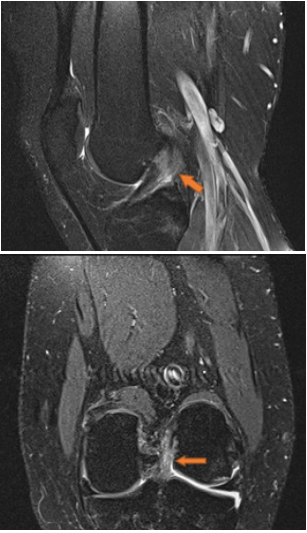
Figure 6: MRI of knee, in sagittal plane proton density sequence. Complete lesion of ACL Gr. III.
Results
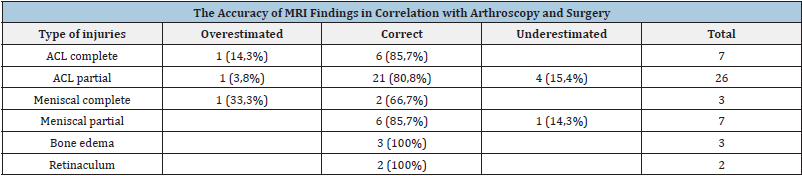
50 patients with knee sport injuries were included in this study, from them 35 male (70%) and 15 female (30%) (Table 1). The age of the patients range from 16 years to 35years, 5 patients were at the range to 20ty, 28 patients were at the age between 20ty and 30ty, and 17 patients were at the age between 30ty and 40ty (Table 2). Depending on the sport which cases the injury 20 patients get knee injury while preforming handball, 10 football, 7 patients during ski activities, 3 patients during running and jumping, and the rest 10 patients from bicycling together with other different sport activities (Table 3). Depending on the MRI results, MRI findings for distribution of the type of injuries of the knee: in 33 patient lesion of Anterior Cruciate Ligament (ACL) was detected on MRI, from which 7(21.2%) patients were with complete lesion and 26(78.8%) were with partial lesion. 3 patients have finding of bone edema and cartilage injuries. 2 patients have retinaculum lesions. 7 patients have meniscal lesion, from them 3 patients (42.85%) have complete lesion and 4 patients (57.15%) have incomplete lesion.5 patients were with combined injuries of meniscal lesion and lesion of ACL (Table 4 & 5). With comparison of the results from MRI finding with arthroscopy or surgery findings which were taken as a gold standard we get the accuracy of MRI in 66.7% of finding the meniscal complete lesion and 85.7% of meniscal incomplete lesion. The accuracy of MRI in detection the ACL lesion was 85.7% in complete ACL lesion and 80.8% for detection the ACL partial lesion. 100% for bone edema and cartilage lesion and also 100% for retinaculum lesion (Table 6). This study has shown total accuracy of MRI in finding the sport knee injuries at 87%.
Table 1: Distribution of patients by gender.
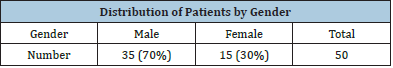
Table 2: Distribution of patients by gender and age in decades.

Table 3: Distribution of patients by gender and the sport that causes the trauma.
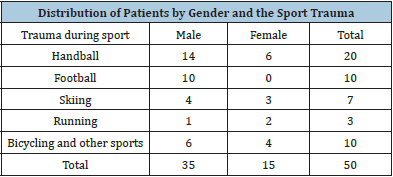
Table 4: Distribution by the type of injuries of the knee elements
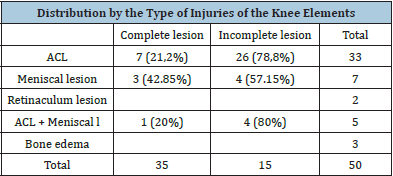
Table 5: Distribution by the degree of the lesion: Gr. 0 - intact, Gr. I - low-grade partial tear, Gr. II - high-grade partial tear, and Gr. III - complete tear.
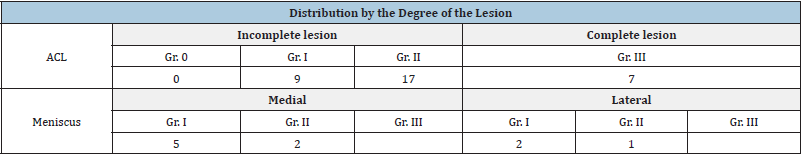
Table 6: The accuracy of MRI findings in correlation with arthroscopy and surgery.
Discussion
MRI of the knee is the basic tool in the detection of knee injuries especially in sport activity and younger patients. Injuries to menisci and cruciate ligaments can be diagnosed on MRI with a high degree of sensitivity and specificity, but it is shown that the accuracy of MRI decreases in patients with multiple injuries [10]. Although arthroscopy is established as the Gold Standard in diagnosis of meniscal and ligament injuries, MRI remains a high sensitive, noninvasive diagnostic method, which can reduce the use of diagnostic arthroscopy [11]. For the adequate evaluation of the internal knee elements, the knee must be scanned in the axial, coronal, and sagittal planes using thin sections (3-mm thick) with a combination of T1- and T2-weighted techniques as well as at least one 5-mm thick Short Tau Inversion Recovery (STIR) or T2-weighted image with fat suppression and proton density [12]. The anterior and posterior horns of the medial and lateral menisci appear as wedge-shaped, low-intensity structures pointing toward each other on sagittal and coronal views. High signal within the meniscus, extending to the superior or inferior articular surface, constitutes a meniscal tear [13]. Horizontal-oblique tears are considered the results of myxoid degeneration and are called “degenerative” tears. Those oriented in the vertical direction, which involve both the superior and inferior articular surfaces, are considered “traumatic” tears. Tears do not need to be seen in both the sagittal and coronal planes, as they are only visualized when they are perpendicular to the plane of the section. In fact, tears running oblique to both the coronal and sagittal planes may well be visualized only by a notch on the articular surface. This “notch sign” has served us very well over the last decade in diagnosing subtle meniscal tears [14]. Occasionally, a large piece of meniscal fibrocartilage will become detached from its capsular attachment and flip back-to-front or centrally into the intercondylar notch. Clinically, these patients present with a locked knee. These “bucket-handle” or “flap” tears are recognized on the basis of two findings: An absence of the normal meniscus in its expected position and abnormal meniscal-intensity material in an unexpected location [15].
Bucket-handle tears flipping from posterior to anterior appear as arrowheads pointing posteriorly in the position of the anterior horn of the meniscus, with nothing at all in the expected position of the posterior horn. This pattern is more common for bucket-handle tears of the lateral meniscus. Tears flipping from the periphery into the intracondylar region of the knee appear as an extra structure adjacent to the cruciate ligaments, with an absence of meniscal signal in the expected position of the posterior horn. Typically, this pattern is seen with bucket-handle tears of the medial meniscus. When the displaced meniscal fragment lies parallel to the Posterior Cruciate Ligament (PCL), it may produce the “double PCL sign” [16]. The Anterior Cruciate Ligament (ACL) may be seen on sagittal images; however, it is always seen as an upside-down “V” on coronal images. The ACL is lateral to the rounded dark Posterior Cruciate Ligament (PCL) [17]. The ACL is most commonly injured by valgus stress to the knee while the leg is in external rotation, e.x a “clipping” injury in football or getting hit laterally coming down from a layup in basketball [18]. In addition to the medial distraction resulting from valgus stress during an ACL injury, there is lateral impaction. This may lead to bone marrow contusions of both the femoral and tibial surfaces of the lateral compartment [19]. Bone marrow contusions (also called “bone bruises” and “trabecular fractures”) cannot be seen on plain films and can be a major source of pain. They should be suspected in the patient with an acutely injured knee without a meniscal or ligamentous injury in the absence of plain-film findings of fracture. Because their water content is higher than that of adjacent fatty bone marrow, these contusions are best detected on fat-suppressed T2-weighted images [20]. In evaluating bone marrow contusions, it is important to determine if they extend to the articular surface, as this is usually an indication that the patient must rest for 30 days. Continued activity in this setting could convert a bone bruise with intact cartilage (type I) to one in which the cartilage becomes disrupted (type II), leading to early osteoarthritis. Bone bruises can be seen whenever abnormal forces are applied to normal tissue or essentially normal forces are applied to weakened tissue, e.x, osteoporotic bones in middle-aged “weekend warriors” [21]. An interesting pattern of bone marrow contusion can be seen with traumatic dislocation of the patella. After the patella dislocates laterally when the knee is in hyperextension, the quadriceps contracts, jamming the medial patellar facet against the lateral femoral condyle, resulting in bone marrow edema on both surfaces. Usually, this is also associated with disruption of the black line of the medial retinaculum, which, acutely, may have associated bleeding or edema. Such injuries are seen in football and basketball players who come down on a hyperextended knee [19,20]. Lesions of the PCL and the lateral collateral ligament are much less common than their anterior counterparts. The PCL is recognized as a dark C-shaped structure on sagittal images and is visualized as a dark, rounded structure seen en face on coronal images. The coronal images are best for visualizing partial PCL tears (which show increased signal in a normally black structure), while the sagittal view may better illustrate complete disruption [20,21].
Conclusion
MRI is noninvasive diagnostic tool with high accuracy and it is the primary approach in sport knee injuries. Thus MRI is more adequate to the diagnostic arthroscopy and we recommend MRI as the primary diagnostic tool for the evaluation of sports knee injuries. Over the past 20 years, MRI has become the leading imaging method for the evaluation of the painful knee following a sports injury. It can detect soft tissue abnormalities (meniscal and cruciate/collateral ligament tears) and fractures that cannot be detected by plain film. These findings are critical for the therapeutic decisions to be made by the orthopedic surgeon and traumatologist. This study has shown total accuracy of MRI in finding the sport knee injuries at 87%, which makes it valuable noninvasive diagnostic tool for primary sport injuries.
References
- Brinckmann P, Frobin W, Leivseth G (2002) Musculoskeletal biomechanics. Thieme, New York, NY, USA.
- Yawn BP, Amadio P, Harmsen WS, Hill J, Ilstrup D, et al. (2000) Isolated acute knee injuries in the general population. J Trauma 48(4): 716-723.
- Standaert CJ, Herring SA (2009) Expert opinion and controversies in musculoskeletal and sports medicine: Stingers. Arch Phys Med Rehabil 90(3): 402-406.
- Vincken PW, Ter Braak AP, Van Erkel AR, Coerkamp EG, W de Rooy TP, et al. (2007) MR imaging: Effectiveness and costs at triage of patients with nonacute knee symptoms. Radiology 242(1): 85-93.
- Livstone BJ, Parker L, Levin DC (2002) Trends in the utilization of MR angiography and body MR imaging in the US Medicare population: 1993-1998. Radiology 222(3): 615-618.
- Nikolaou VS, Chronopoulos E, Savvidou C, Plessas S, Giannou-dis P, et al. (2008) MRI efficacy in diagnosing internal lesions of the knee: A retrospective analysis. J Trauma Manag Outcomes 2(1): 4.
- Rubin DA, Kettering JM, Towers JD (1998) MR imaging of knees having isolated and combined ligament injuries. AJR Am J Roentgenol 170(5): 1207-1213.
- Zairul-Nizam ZF, Hyzan MY, Gobinder S, Razak MA (2000) The role of preoperative magnetic resonance imaging in internal derange-ment of the knee. Med J Malaysia 55(4): 433-438.
- Madhusudhan T, Kumar T, Bastawrous S, Sinha A (2008) Clinical examination, MRI and arthroscopy in meniscus and ligamentous knee injuries-a prospective study. J Orthop Surg Res 3: 19.
- Mazlomy M, Makhmalbaf H, Kashani Omidi F, Mahvalati Sadri A (2007) Comparison of clinical findings with arthroscopic findings in knee intra-articular injuries. Med J Mashhad Univ Med Sci 49: 421-6.
- Thomas S, Pullagura M, Robinson E, Cohen A, Banaszkiewicz P (2007) The value of magnetic resonance imaging in our current management of ACL and meniscus injuries. Knee Surg Sports Traumatol Arthrosc 15(5): 533-536.
- Peleg B, Ely S, Hagai A, Nachman A, Dekel S, et al. (2006) Accuracy of magnetic resonance imaging of the knee and unjustified surgery. Clin Orthop Relat Res 447: 100-104.
- Kuikka PI, Sillanpää P, Mattila VM, Niva MH, Pihlajamäki HK (2009) Magnetic resonance imaging in acute traumatic and chronic meniscal tears of the knee: A diagnostic accuracy study in young adults. Am J Sports Med 37(5): 1003-80.
- Ramnath RR, Magee T, Wasudev N, Murrah R (2006) Accuracy of 3-T MRI using fast spin-echo technique to detect meniscal tears of the knee. AJR Am J Roentgenol 187(1): 221-225.
- Mackenzie R, Palmer CR, Lomas DJ, Dixon AK (1996) Magnetic resonance imaging of the knee: Diagnostic performance studies. Clin Radiol 51(4): 251-257.
- Jee WH, McCauley TR, Kim JM, Jun DJ, Lee YJ, et al. (2003) Meniscal tear configurations: Categorization with MR imaging. AJR Am J Roentgenol 180(1): 93-97.
- Khanda GE, Akhtar W, Ahsan H, Ahmad N (2008) Assessment of menisci and ligamentous injuries of the knee on magnetic resonance imaging: Correlation with arthroscopy. J Pak Med Assoc 58(10): 537-540.
- Rayan F, Bhonsle S, Shukla DD (2009) Clinical, MRI, and arthroscopic correlation in meniscal and anterior cruciate ligament injuries. Int Orthop 33(1): 129-32.
- Witonski D (2008) Acute traumatic hemarthrosis of the adult’s knee-A diagnostic options in arthroscopic era. Literature review. Chir Narzadow Ruchu Ortop Pol 73(5): 339-343.
- Vaz CE, Camargo OP, Santana PJ, Valezi AC (2005) Accuracy of magnetic resonance in identifying traumatic intraarticular knee lesions. Clinics (Sau Paulo) 60(6): 445-450.
- Helms CA (2002) The meniscus: Recent advances in MR imaging of the knee. AJR Am J Roentgenol 179(5): 1115-1122.
© 2022 Ana Lazarova. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






