- Submissions

Full Text
Gastroenterology Medicine & Research
Gastric Post-Transplant Lymphoproliferative Disorder after Allogenic Stem Cell Transplantation
Legarda M1, Garcia-Alberdi E2, Lopez-Almaraz R3, Berastegui M4, Irastorza I1,5, Vitoria JC1,5 and Astigarraga I3,5*
1Pediatric Gastroenterology Unit, Department of Pediatrics, Cruces University Hospital, Biocruces Bizkaia Health Research Institute, Spain
2Department of Histopathology, Cruces University Hospital, Spain
3Pediatric Haematology and Oncology Unit, Department of Pediatrics. Cruces University Hospital. Biocruces Bizkaia. Health Research Institute, Spain
4Department of Pediatric Radiology, Cruces University Hospital, Spain
5Department of Pediatrics, Basque Country University, Spain
*Corresponding author: Itziar Astigarraga, Head of the Department of Pediatrics, Cruces University Hospital, Barakaldo, Bizkaia, Spain
Submission:December 21, 2021;Published: January 10, 2022

ISSN 2637-7632Volume6 Issue4
Case Report
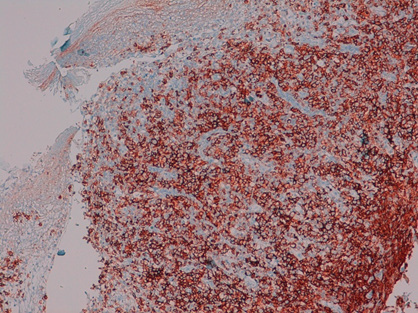
Post-Transplant Lymphoproliferative Disease (PTLD) is a well-known complication following transplantation. Its estimated incidence is 2.5% at 1 year after bone marrow transplantation [1,2]. PTLD consists of excessive (most frequently B) lymphocyte proliferation in immunosuppressed patients. Most cases are associated with primary EBV infection and occur within the first year after transplantation. Staging ranges from plasmocytic hyperplasia to lymphoma. PTLD can be potentially fatal and treatment is based on reduced immunosuppression, antiviral therapies, B cell proliferation blockers, chemotherapy and most recently T-cell therapies [1,3]. We present the case of an 18-year-old young man, who presented with a 48-hour history of low-grade fever, anorexia, abdominal discomfort and vomiting. In 20Post-Transplant Lymphoproliferative Disease (PTLD) is a well-known complication following transplantation. Its estimated incidence is 2.5% at 1 year after bone marrow transplantation [1,2] he had been diagnosed with acute T cell lymphoblastic leukaemia, which was treated with chemotherapy. Three years later he developed a second leukaemia (mixed phenotype acute leukaemia), for which he received a BMT from an unrelated donor 4 months prior to admission. Upon presentation, he was receiving immunosuppressive treatment with mycophenolate and anti-infectious prophylaxis with acyclovir, co-trimoxazole and posaconazole. A CT scan showed an area of inflammation in the gastric antrum (Figure 1). Subsequently, he underwent an upper GI endoscopy that showed nodularity and bleeding in the gastric body (Figure 2). Biopsies were obtained indicating a B cell lymphoma (Figure 3 & 4), following which a PET/CT scan was performed showing multisystemic lymphoproliferative infiltration. His EBV PCR in blood was 85,200 copies/ml. Unfortunately the PTLD was progressive, refractory to different therapies, and fatal in 5 months after PTLD diagnosis. Gastric PTLD is a very rare entity with only a few cases having been reported in the literature [1,4]. Diagnosis and management of EBV gastrointestinal PTLD is difficult in many patients, but a multidisciplinary approach and a prompt biopsy to identify the PTLD subtype are important for appropriate therapy. In this case, gastric biopsies showed an aggressive B-cell lymphoma. Because treatment modalities can vary significantly, it is essential to differentiate between PTLD and other conditions such as tumor relapse, GVHD or infection in transplanted patients with abdominal symptoms.
Figure 1: Abdominal CT scan showing a circumferential wall thickening in the gastric antrum and an incidental finding of an uncomplicated gallstone.

Figure 2: Upper GI Endoscopy findings.

Figure 3: Gastric body biopsies. HE stain.
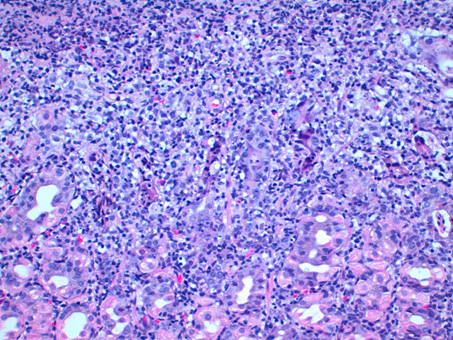
Figure 4: Gastric body biopsies. CD 20 stain.
References
- Marie E, Navallas M, Navarro OM, Punnett A, Shammas A, et al. (2020) Posttransplant lymphoproliferative disorder in children: A 360-degree perspective. Radiographics 40(1): 241-265.
- Lindsay J, Othman J, Heldman MR, Slavin MA (2021) Epstein-Barr virus posttransplant lymphoproliferative disorders: Update on management and outcomes. Curr Opin Infect Dis 34(6): 635-645.
- Wistinghausen B, Gross TG, Bollard C (2013) Post-transplant lymphoproliferative disease in pediatric solid organ transplant recipients. Pediatr Hematol Oncol 30(6): 520-531.
- Khedmat H, Ghamar-Chehreh ME, Amini M (2014) Localization of post-transplant lymphoproliferative disorders to the stomach might be associated with favorable outcome: A systematic review. Saudi J Kidney Dis Transpl 25(2): 353-361.
© 2022 Astigarraga I. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






