- Submissions

Full Text
Gastroenterology Medicine & Research
Hypoglycemia Refractory in Patient with Metastatic Gastrointestinal Stromal Tumor (GIST): Case Report and Literature Review
Facanha ALBP1, Junior JEBR1 and Marcos Pedro Guedes Camandaroba1*
1Department of Clinical Oncology, Ac Camargo Cancer Center, Brazil
*Corresponding author:Marcos Pedro Guedes Camandaroba, Medical Oncologist, Antonio Prudente Street, São Paulo, Brazil
Submission: February 09, 2021;Published: February 24, 2021

ISSN 2637-7632Volume5 Issue4
Abstract
A case of NICTH secondary to gastrointestinal stromal tumor (GIST) is described, male patient admitted to the emergency referring asthenia and drowsiness, and measured blood glucose of 20mg/dL. Patient continued to present episodes of recurrent hypoglycemia: 33/55/32mg/dL, even with continuous reposition of 10% glucose solution. Hypoglycemia can be related to several tumors, including islet cell and non-islet cell tumors. Non-islet cell tumor hypoglycemia (NICTH) is a rare and serious complication of malignancy, and its presence is usually associated with a poor prognosis. The most common cause of this type of hypoglycemia is tumor overproduction of insulin-like growth factor II (IGF-II), which stimulates the insulin receptor, leading to decreased insulin and glucagon levels. The diagnosis of NICTH is based on clinical and laboratory findings. Patients with NICTH have low serum concentrations of insulin and C-peptide during hypoglycemia. The treatment of this condition is related to the control of the underlying neoplasia. In patients who are unable to undergo invasive procedures, the use of corticosteroids is a good treatment option, leading to normalization of glycemia. Its management is of unquestionable importance to ensure the patient’s quality of life. A review of the literature on epidemiology, diagnosis and treatment of this complication follows.
Keywords: Hypoglicemia; Paraneoplastic endocrine syndromes; Gastrointestinal stromal tumors
Introduction
Several types of tumors are associated with Non-islet cell tumor hypoglycemia (NICTH), although gastrointestinal stromal tumor (GIST), is rarely involved [1,2]. These tumors are usually large and located in the chest or retroperitoneum [1]. NICTH is associated with the production of IGF-II, which stimulates the insulin receptor, leading to decreased insulin and glucagon levels, consumption of glucose by tumor cells, reduction ketogenesis, glycogenolysis and gluconeogenesis, reduction of lipolysis and glucose storage in skeletal muscles; it also binds to IGF-I receptor, leading to decreased growth factors and IGF-I levels [3,4]. The treatment of this condition is related to the control of the underlying neoplasia, being indicated cytoreductive surgery or tumor embolization, for patients that don’t have a controlled disease with the regular treatment used for GIST (bases on tyrosine kinase inhibitors) [5,6]. In patients who are unable to undergo invasive procedures, the use of corticosteroids is a good treatment option, leading to normalization of glycemia [6,7]. Although, hypoglycemia can reoccur once they are discontinued [7]. We report a rare case of a metastatic GIST and refractory hypoglycemia, followed by a review of the diagnostic literature and treatment of this complication.
Case Report
A 50-years-old Brazilian man, diagnosed with GIST of the small intestine, was admitted to the emergency room reporting asthenia and drowsiness, in addition to abdominal pain and progressive increase in abdominal volume. Upon admission, he presented a blood glucose level of 20mg/dL. He had a medical history of type 2 diabetes mellitus, currently using metformin 850mg per day. As GIST treatment, he had been taking Sorafenib 800mg per day for about a month, as fourth-line systemic treatment. The previous systemic treatment options were Imatinib, Sunitinib and Regorafenib. Due to episodes of recurrent hypoglycemia, he was admitted to the intensive care unit (ICU). Despite of continuous replacement of 10% glucose solution, it persisted with glycemia lower than 60mg/dL, and treatment with glucagon 0.1mg per hour was started, with partial improvement of hypoglycemic episodes. Dexamethasone 12mg per day was associated, achieving better glycemic control, but still with occasional episodes of hypoglycemia. The serum insulin level was less than 1mU/L with the patient’s body mass index (BMI) equal to 31.55kg/m2 (reference value for BMI above 30kg/m2: 2 to 23mU/L) and the C-peptide value was 0.02ng/ml (reference value: 1.1 to 4.4ng/ml). IGF1 was 33ng/mL (reference value for age 25- 54 years: 105-362ng/mL). On the 5th day of hospitalization, no more hypoglycemia episodes occurred (Table 1). After 48 hours without a blood glucose level lower than 60mg/dL, the patient was discharged using corticosteroids (Dexamethasone 8mg per day), with a scheduled return for tumor embolization.
Table 1:Blood glucose values during hospitalization.
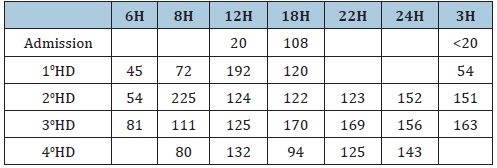
H: Hours; HD: Hospitalization Day; Blood Glucose: mg/dL
Discussion
Hypoglycemia can be related to several tumors, including
islet cell and non-islet cell tumors [2]. NICTH is a rare and
serious complication of malignancy, and its presence is usually
associated with a poor prognosis [2,5]. Several types of tumors
are associated with NICTH, most commonly mesenchymal tumors,
fibroids, carcinoids, myelomas, lymphomas, hepatocellular and
colorectal carcinomas; and GIST is rarely involved [1]. Symptoms
of hypoglycemia occur more frequently in the fasting state and may
include confusion, lethargy, diaphoresis, or progressive drowsiness,
with some patients presenting coma as the initial manifestation of
hypoglycemia [5]. The diagnosis of NICTH is based on clinical and
laboratory findings [5]. Medical history and physical examination
can usually help to find the cause of hypoglycemia in a patient with a
known tumor burden. The causes of tumoral hypoglycemia include
extensive liver or adrenal infiltration by the tumor, resulting in the
destruction of the liver or adrenal glands; tumor production of high
levels of IGF-II; or rarely, insulin production by the tumor cells [3,4].
The initial laboratory evaluation includes measurement of glucose,
insulin, proinsulin, C-peptide, during an episode of hypoglycemia
[8]. In contrast to the biochemical findings in individuals with hyper
insulinemic hypoglycemia, patients with NICTH have low serum
concentrations of insulin and C-peptide during hypoglycemia [7,8].
There are few other disorders that cause hypoglycemia with low
levels of serum insulin and C-peptide. In patients with NICTH, the
plasma glucose response to glucagon administration is typically
greater than 25mg/dL [9]. If the glucose response to glucagon
is less than 25mg/dL, the possibilities include extensive tumor
replacement of liver tissue, resulting in low hepatic glycogen stores
or an alternative mechanism [6,9]. The treatment of this condition
is related to the tripod: correction of hypoglycemia, control of the
underlying neoplasia and the prevention of recurrent hypoglycemia
if the tumor cannot be controlled [5,6]. The basis of treatment is
in the control of tumor malignancy. If it is not possible to perform
tumor resection, other treatment options can be used to control
the tumor and solve hypoglycemia, as systemic therapy, radiation,
cryoablation, radiofrequency ablation or selective embolization of
the blood vessels that feed the tumor [8].
In situations where the underlying malignancy cannot be
treated, medications are needed to prevent recurrent symptoms
of hypoglycemia. In case series and reports, hypoglycemia was
controlled with glucocorticoids, glucagon or recombinant human
growth hormone [6,10]. The somatostatin analogs and diazoxide
were not effective [10]. Glucocorticoids (30 to 60mg daily) are
a reasonable initial therapy [7]. Glucocorticoids decrease the
amount of IGF-II and increase its clearance and impair the action
of insulin. High-dose glucocorticoid-refractory hypoglycemia is
particularly found in patients with disseminated disease [6,7]. If
hypoglycemia persists, patients can use glucagon [9]. Obtaining a
glycemic response to glucagon, a long-term intravenous infusion
of glucagon (0.06 to 0.30mg/hour) is recommended [5]. Growth
hormone at supraphysiological doses of 3 to 12mg per day has
been shown to increase IGF-binding protein, which bind to IGF-II
and prevent interaction with the insulin receptor, thereby reducing
hypoglycemia, however, it increases IGF-I and has the potential to
increase tumor growth [4,10]. Despite NICTH is a rare condition,
it should be remembered whenever there are suggestible clinical
and laboratory signs and symptoms, once it is a crucial condition
and it gives the patient a worse prognosis. Its management is of
unquestionable importance to ensure the patient’s quality of life,
given that if not treated correctly and continually, hypoglycemia can
happen again and cause successive hospitalizations or even death.
Acknowledgement
1. Facanha ALBP: She reviewed the literature; she wrote the text.
2. Junior JEBR: He collected data from the patient’s case report;
He wrote the text.
3. Camandaroba MPG: He reviewed the literature; he wrote and
edited the text.
Conflict of Interest
We declare that there was no financial interest or conflict of interest.
References
- Michelle A, Stephen A (2014) Thyroid hormone inactivation in gastrointestinal stromal tumors. N Engl J Med 371(1): 86-87.
- Scott K (2009) Non-islet cell tumor hypoglycemia. J Pain Symptom Manage 37(4): e1-3.
- Morbois-Trabut L, Maillot F, De Widerspach A, Lamisse F, Couet C (2004) Big IGF-II-induced hypoglycemia secondary to gastric adenocarcinoma. Diabetes Metab 30(3): 276-279.
- Izumi F, Naomi H, Yukiko I, Kumiko Y, Yuko M, et al. (2006) Clinical features of insulin-like growth factor-II producing non-islet-cell tumor hypoglycemia. Growth Horm IGF Res 16(4): 211-216.
- Timothy W, Maria J, Massimo P (2014) Management of non-islet-cell tumor hypoglycemia: A clinical review. J Clin Endocrinol Metab 99(3): 713-722.
- Bourcigaux N, Arnault-Ouary G, Christol R, Périn L, Charbonnel B, et al. (2005) Treatment of hypoglycemia using combined glucocorticoid and recombinant human growth hormone in a patient with a metastatic non-islet cell tumor hypoglycemia. Clin Ther 27(2): 246-251.
- Teale JD, Marks V (1998) Glucocorticoid therapy suppresses abnormal secretion of big IGF-II by non-islet cell tumours inducing hypoglycaemia (NICTH). Clin Endocrinol (Oxf) 49(4): 491-498.
- De Boer J, Jager PL, Wiggers T, Nieboer P, MacHteld W, et al. (2006) The therapeutic challenge of a nonresectable solitary fibrous tumor in a hypoglycemic patient. Int J Clin Oncol 11(6): 478-481.
- Hoff AO, Vassilopoulou-Sellin R (1998) The role of glucagon administration in the diagnosis and treatment of patients with tumor hypoglycemia. Cancer 82(8): 1585-1592.
- Perros P, Simpson J, Innes JA, Teale JD, McKnight JA (1996) Non-islet cell tumour-associated hypoglycaemia: 111In-octreotide imaging and efficacy of octreotide, growth hormone and glucocorticosteroids. Clin Endocrinol (Oxf) 44(6): 727-731.
© 2021 Marcos Pedro Guedes Camandaroba. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






