- Submissions

Full Text
Gastroenterology Medicine & Research
Does Vitamin D Deficiency Correlates with Metabolic Syndrome in Egyptian Population
Rasha Ibrahem Salama1 and Aya Mohamed Mahros2*
1 Assistant consultant, Department of Tropical Medicine, Faculty of Medicine, Zagzig University, Egypt
2Lecturer at Department of Hepatology, gastroenterology and infectious diseases, Faculty of Medicine, Kafrelsheikh University, Egypt
*Corresponding author:Aya Mohammed Mahros, Lecturer at Department of Hepatology, Gastroenterology and infectious disease Faculty of Medicine, Kafrelsheikh University, Egypt
Submission: December 17, 2020;Published: February 17, 2021

ISSN 2637-7632Volume5 Issue4
Abstract
Background: Metabolic syndrome (MS) has become a serious health problem worldwide and it is a major cause of morbidity and mortality especially from cardiovascular diseases. Different factors involved in pathogenesis like environmental, genetic, and sedentary life. Recent studies demonstrates that Vitamin D3 deficiency has a growing role in pathogenesis of MS. Many studies had addressed the relationship between serum Vitamin D3 and metabolic syndrome but to the best of our knowledge, few studies about this relationship in Egyptian population.
Aims: To assess the relationship between deficiency of Vitamin D3 with metabolic syndrome in Egyptian population.
Patients and methods: This is cross sectional study invite 200 participants from healthy clubs but only 180 accept to participate. According to the presence or absence of metabolic syndrome, our participant were divided into two groups. All participants were subjected to detailed medical history, clinical and anthropometric assessment, and laboratory analysis including serum Vitamin D3
Result: The mean age of the studied patients was 40.91±72, and majority were female (66.7%). Metabolic syndrome cases were significantly higher as regard the age, SBP, DBP, TG, FBS, WC and BMI but significantly lower regard HDL and Vitamin D3, and no significant association with sex. Vitamin D deficiency cases were significantly higher as regard Age, SBP, DBP, TG, FBS, WC and BMI but sig lower regard HDL. There was significant different between patients with and without Vitamin D3 deficiency as regard the presence of metabolic syndrome (P value=.00). There was moderate negative correlation between Vitamin D3 deficiency and age, SBP, DBP, FBS, WC and BMI with positive weak correlation with HDL level. Vitamin D3 deficiency < 20ng/ml and BMI >35 were significant predictors for metabolic syndrome with (P value 0.00, 0.04) respectively.
Conclusion: Vitamin D3 level inversely correlates with the presence of metabolic syndrome in Egyptian Population.
Keywords: Metabolic syndrome; Vitamin D deficiency
Introduction
Metabolic syndrome (MS) has become a major health problem worldwide and it is a major cause of morbidity and mortality especially from cardiovascular diseases. Hypertension, dyslipidemia, hyperglycemia, insulin resistance, abdominal obesity is major component of MS [1]. Factors involved in pathogenesis of MS includes environmental, genetic, and sedentary life [2]. Vitamin D deficiency has a growing role in pathogenesis of MS [3]. A strong relationship of Vitamin D3 deficiency and the degree of obesity especially central one may be related to insufficient sun exposure and outdoor activities [4]. Vitamin D3 deficiency inversely affects the insulin secretion [5]. Many studies reported that the lower level of Vitamin D3 induce the development of insulin resistance and thus Type 2 DM by decreasing insulin sensitivity [6]. Vitamin D3 deficiency have been reported to upregulate the renin-angiotensin-aldosterone system (RAAS), resulting in systolic and diastolic hypertension [7]. Many studies addressed risk factors for MS, but there are few studies on the role of Vitamin D3 deficiency on MS especially in Egyptian population.
Aim of study
Our study aimed assess the relationship between deficiency of Vitamin D with metabolic syndrome in Egyptian population.
Patients and Methods
Our cross sectional study invite 200 subjects from healthy clubs at Kafrelsheikh and Zagzig governorate, Egypt. However, 180 only were enrolled into the study as 20 patients did not attend their appointment for the laboratory tests. The criteria for inclusion in the study were any sex, or age, and participant were divided into two groups according to presence or absence of MS. The exclusion criteria were refusal to participate and Vitamin D supplementation. All participants were subjected to detailed medical history, clinical and anthropometric assessment, and laboratory analysis. MS was diagnosed if the patient had at least 3 out of 5 of its components, in accordance with the modified criteria proposed by the IDF in 2009. These includes waist circumference≥80cm, fasting glycemia≥100mg/dL, triglyceride level≥150mg/dL, HDL cholesterol level <50mg/dL, and elevated blood pressure (sBP≥130 and/or dBP≥85mmHg) or related therapies to any of above conditions [8]. A digital scale were used to assess anthropometric measurements. Waist circumference was measured midway between the upper margin of the iliac crest and the lower rib margin. We considered a waist circumference≤80 Body mass index (BMI) in the range of 18.5- 24.9kg/m2 as normal, and between 25.0kg/m2 and 29.9kg/m2 denoted overweight, and I≥30kg/m2 indicated obesity. Blood pressure was measured using a manual manometer in a semi sitting participant after adjusting the cuff according to arm circumference at the heart level. Fasting blood samples were withdrawn for biochemical assessment: serum cholesterol, high density lipoprotein (HDL), triglycerides (TG,), and Vitamin D3. Vitamin D3 was measured by competitive radioimmunoassay kits (Cobas®; Roche Vitamin D Total first generation assay (25OHD-I), Roche Diagnostics, Indianapolis, IN, USA).
Ethics and consent
The study was approved by the Faculty’s ethics committee and permission was obtained from all departmental heads who ensured confidentiality was maintained and ethical principles were followed. Prior to participation in the study, the background and reasons for conducting the study were explained and prospective patients were not obliged to participate. Written informed consent was obtained from all participants
Statistical analysis
Statistical analysis was performed by using statistical package for social sciences (SPSS) version 22.0. Descriptive statistics was presented as proportion, Mean ± standard deviation (SD) and median with interquartile range. Comparative analysis was done by χ2 test. A P-value less 0.05 was considered significant.
Results
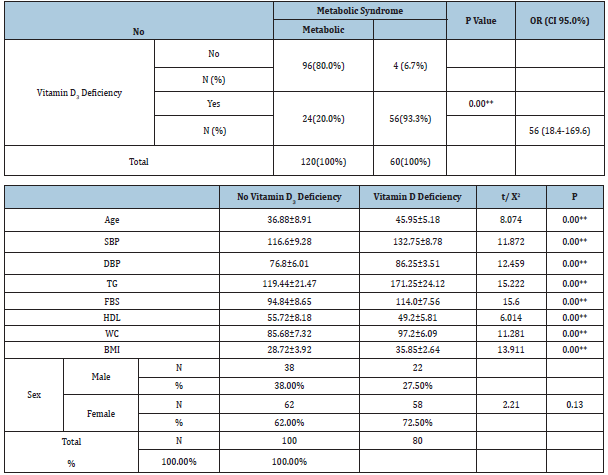
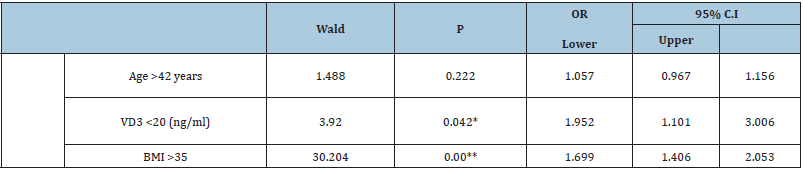
We initially invited 200 subjects, however, 180 only were enrolled into the study as 20 patients did not attend their appointment for the laboratory tests. The mean age of the studied patients was 40.91±8.72, and majority were female (66.7%). Metabolic syndrome was present in 60 participants (33.3%) while Vitamin D3 deficiency was present in 80 participants (44.4%) (Table 1). Table 2 show that metabolic syndrome cases were significantly higher as regard the age, SBP, DBP, TG, FBS, WC and BMI but significantly lower regard HDL and Vitamin D3, and no significant association with sex. Table 3 show there was significant different between patients with and without Vitamin D3 deficiency as regard the presence of metabolic syndrome P value=.00 with 95% confidence interval at 56(18.4-169.6). Significant association and significant risk between VD deficiency and MS. Table 4 show that Vitamin D3 deficiency cases were significantly higher as regard Age, SBP, DBP, TG, FBS, WC and BMI but significantly lower regard HDL and no significant association with sex. Table 5 show a spearman correlation analysis was run to determine the relationship between Vitamin D3 deficiency and variable risk factors'. There was moderate negative correlation between Vitamin D deficiency and age, SBP, DBP, FBS, WC and BMI. (r=. -0.495), (r=-0.610), (r=-0.661), (r=-0.622), (r=-0.692), (r=-0.632), (r=-0.617), (r=-0.617) respectively and positive weak correlation with HDL level (r=.339). Table 6 show multivariate logistic regression for independent predictors of metabolic syndrome demonstrate that Vitamin D3 deficiency <20ng/ml and BMI >35 were significant predictors with (P value 0.00, 0.04) respectively, while we found Age >42 were insignificant one (p value=.22) for metabolic syndrome.
Table 1:Age and sex distribution among studied group.
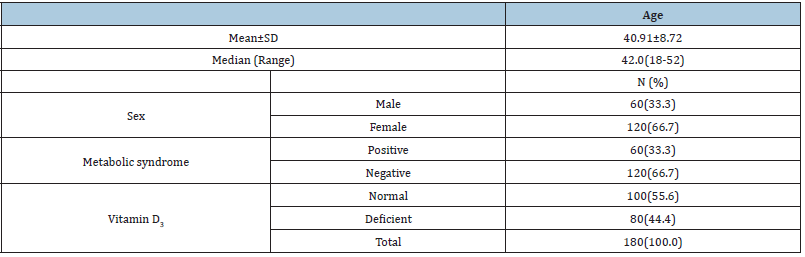
Table 2:Comparison between metabolic and non-metabolic syndrome.
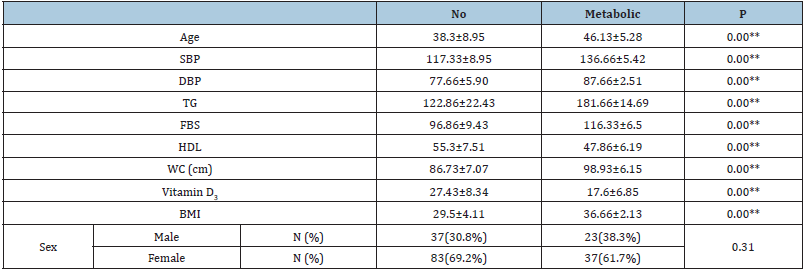
Table 3:Association and risk assessment between metabolic syndrome and Vitamin D deficiency.
SBP: Systolic Blood Pressure, DBP: Diastolic Blood Pressure, TG: Triglyceride, FBS: Fasting Blood Sugar, HDL: High Density Lipoprotein, WC: Waist Circumference, BMI: Body Mass Index.
Table 4:Relation with Vitamin D3 deficiency.
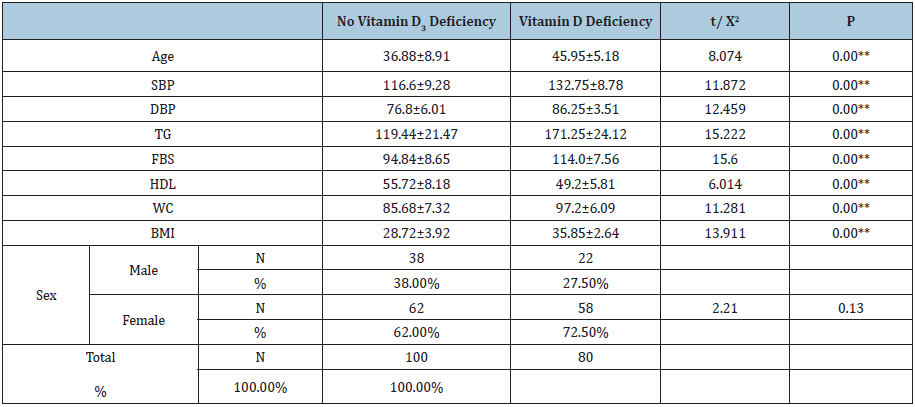
Table 5:Correlations between Vitamin D and other parameters.
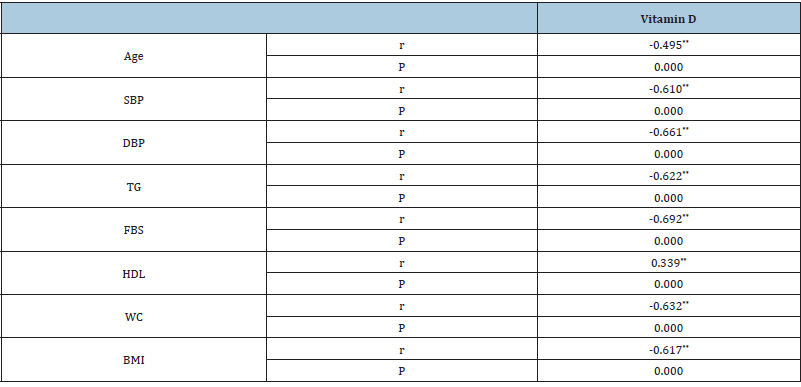
Table 6:Multivariate logistic regression for independent predictors of MS.
Discussion
MS is a group of abnormal metabolic disorders characterized by hypertension, insulin resistance, hyperglycemia, dyslipidemia, and central obesity. It is a major cause of morbidity and mortality [9]. In our study we divide participant into two groups according to the presence or absence of MS based on above mentioned criteria. Our study demonstrate that MS group have older age, higher systolic and diastolic blood pressure, TG level, waist circumference and BMI and lower level of Vitamin D and HDL and this are consistent with other studies [10-13] that concluded that MS is more prevalent in obese and elderly people. Our study demonstrated that was significant different between patients with and without Vitamin D3 deficiency as regard the presence of metabolic syndrome and this concordant with many studies [14,15] that concluded that Vitamin D3 deficiency has a growing role in the pathogenesis of MS. Our study showed that Vitamin D3 deficiency cases were significantly higher as regard Age, SBP, DBP, TG, FBS, WC and BMI. This in agreement with a study of Wieder-Huszla and his colleagues that concludes that Vitamin D3 deficiency was an independent factor for MS in the elderly [16]. Another study by Lee and his colleagues that found that lower Vitamin D level was associated with higher blood pressure and CVS risk [8]. Spearman correlation in our study revealed There was moderate negative correlation between Vitamin D3 deficiency and age, SBP, DBP, FBS, WC and BMI and positive weak correlation with HDL level. This was in agreement with many studies [14-16]. Interestingly, our study demonstrated that Vitamin D3 deficiency <20ng/ml and BMI >35 were significant predictors for metabolic syndrome. This in agreement with a study of Wang and his colleagues that concluded that low Vitamin D3 concentration is an independent risk factor for M.S [17,18].
References
- Wu Y, Ding Y, Tanaka Y, Zhang W (2014) Risk factors contributing to type 2 diabetes and recent advances in the treatment and prevention. Int J Med Sci 11(11): 1185-200.
- Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, et al. (2005) Diagnosis and management of the metabolic syndrome: An american heart association/national heart, lung, and blood institute scientific statement. Circulation 112(17): 2735-2752.
- Ford ES, Ajani UA, McGuire LC, Liu S (2005) Concentrations of serum Vitamin D and the metabolic syndrome among US adults. Diabetes Care 28(5): 1228-1230.
- Pereira-Santos M, Costa PR, Assis AM, Santos CA, Santos DB (2015) Obesity and Vitamin D deficiency: A systematic review and meta-analysis. Obes Rev 16(4): 341-349.
- Martin T, Campbell RK (2011) Vitamin D and diabetes. Diabetes Spectr 24(2): 113-118.
- Gagnon C, Daly RM, Carpentier A, Lu ZX, Shore-Lorenti C, et al. (2014) Effects of combined calcium and Vitamin D supplementation on insulin secretion, insulin sensitivity and β-cell function in multi-ethnic Vitamin D-deficient adults at risk for type 2 diabetes: A pilot randomized, placebo-controlled trial. PLoS One 9(10): e109607.
- Li YC, Qiao G, Uskokovic M, Xiang W, Zheng W, Kong J (2004) Vitamin D: A negative endocrine regulator of the renin-angiotensin-sin system and blood pressure. J Steroid Biochem Mol Biol 89-90(1-5): 387-392.
- Lee JH, O’Keefe JH, Bell D, Hensrud DD, Holick MF (2008) Vitamin D deficiency: An important, common, and easily treatable cardiovascular risk factor?. J Am Coll Cardiol 52(24): 1949-1956.
- Cornier MA (2008) The metabolic syndrome. Endocr Rev 29(7): 777-822.
- Al-Shoumer KA, Al-Essa TM (2015) Is there a relationship between Vitamin D with insulin resistance and diabetes mellitus?. World J Diabetes 6(8): 1057.
- Hyppönen E, Boucher BJ (2018) Adiposity, Vitamin D requirements, and clinical implications for obesity-related metabolic abnormalities. Nutr Rev 76(9): 676-692.
- Araghi SO (2015) BMI and body fat mass is inversely associated with Vitamin D levels in older individuals. J Nutr Health Aging 19(10): 980-985.
- Vimaleswaran KS (2013) Causal relationship between obesity and Vitamin D status: Bi-directional Mendelian randomization analysis of multiple cohorts. PLoS Med 10(2): e1001383.
- Strange RC, Shipman KE, Ramachandran S (2015) Metabolic syndrome: A review of the role of Vitamin D in mediating susceptibility and outcome. World J Diabetes 6(7): 896.
- Awad AB, Alappat L, Valerio M (2012) Vitamin D and metabolic syndrome risk factors: Evidence and mechanisms. Crit Rev Food Sci Nutr 52(2): 103-112.
- Janssen HC, Samson MM, Verhaar HJ (2002) Vitamin D deficiency, muscle function, and falls in elderly people. Am J Clin Nutr 75(4): 611-615.
- Wieder-Huszla S, Jurczak A, Szkup M (2019) Relationships between Vitamin D₃ and metabolic syndrome. Int J Environ Res Public Health 16(2): 175.
- Wang CM, Chang CS, Chang YF (2018) Inverse relationship between metabolic syndrome and 25-hydroxy Vitamin D concentration in elderly people without Vitamin D deficiency. Sci Rep 8(1): 17052.
© 2021 Aya Mohammed Mahros. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






