- Submissions

Full Text
Gastroenterology Medicine & Research
Obscure Cause of Upper Gastrointestinal Hemorrhage
Johannes Koch1*, Alison Lytle Perrin2 and Deepti Reddi3
1Department of Medicine, Division of Gastroenterology, University of Washington Medical Center, USA
2Department of Surgery, University of Washington Medical Center, USA
3Department of Laboratory Medicine and Pathology, University of Washington Medical Center, USA
*Corresponding author: Johannes Koch, Clinical Professor, University of Washington Medical Center Department of Medicine, Division of Gastroenterology, USA
Submission: September 01, 2020;Published: September 11, 2020

ISSN 2637-7632Volume5 Issue2
Abstract
A 31year-old man presented to an outside institution’s emergency department with headache, vomiting and no signs of bleeding. With decreased hemoglobin (hgb) of 4.6g/dl and normal head computerized tomography (CT), he was discharged on iron supplement. He presented to our emergency department 3 weeks later with weakness, tachycardia, hypotension, hgb of 5g/dl and a positive fecal occult blood test. With a normal colonoscopy and CT enterography, the patient was discharged to receive biweekly transfusions, and later underwent an outpatient small bowel capsule. Two months later the patient presented with weakness with no overt signs of bleeding and hgb was 4.2g/dl. Push enteroscopy identified a nearly circumferential mass in the proximal jejunum with stigmata of recent hemorrhage. Subsequently six months from the initial presentation, the patient underwent laparoscopic small bowel resection of a 7.3cm friable mass. The histopathology confirmed the endoscopic biopsy findings of a benign lymph vascular proliferation, favoring lymphangioma and an adjacent mesenteric lymph node with marked sinusoidal lymphangiectasia. One week post-surgery, the patient reported feeling well with an increased hgb of 7.1g/dl.
Keywords: IM: Small bowel capsule;Push enteroscopy;Lymphangioma
Introduction
Obscure causes of gastrointestinal bleeding pose a diagnostic challenge to the physician and also can cause delay in diagnosis. When the source of bleeding is not identified by upper and lower gastrointestinal tract endoscopic evaluation, then only the small bowel becomes the focus of investigation. Here, we present a case of jejunal lymphangioma diagnosed by push enteroscopy/endoscopy.
Case Presentation
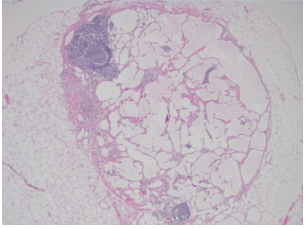
The patient is a 31 year-old second generation Korean American male with past medical history of attention deficit disorder, anxiety, Vitamin D deficiency, and obstructive sleep apnea, presented to an outside emergency department with headache, vomiting and no signs of bleeding. With hemoglobin (hgb) of 4.6g/dl and normal head computerized tomography (CT), he was discharged on iron supplement. He presented to our emergency department 3 weeks later with weakness, tachycardia, hypotension, hgb of 5g/dl and positive fecal occult blood test. A month later with hemoglobin 7.9g/dl, normal colonoscopy and CT enterography, the patient was discharged to receive biweekly transfusions. At the main campus, as an outpatient procedure the patient underwent small bowel capsule with delay in scheduling and interpretation amidst the COVID-19 crisis. Two months later the patient represented with weakness but no overt signs of bleeding with hgb of 4.2g/dl. Push enteroscopy identified a nearly circumferential mass in the proximal jejunum with stigmata of recent bleeding (Figure 1a). The parallel evaluation of the capsule study confirmed a bleeding lesion in the proximal small bowel corresponding to the endoscopy image. Subsequently six months from the initial presentation, the patient underwent laparoscopic small bowel resection showing a 7.3cm friable mass (Figure 1b). Histopathology confirmed the endoscopic biopsy findings of benign lymph vascular proliferation, favoring lymphangioma (Figure 1c), with focal thrombus and a mesenteric lymph node with marked sinusoidal lymphangiectasia (Figure 1d). One week post-surgery, the patient was well with an increased hgb of 7.1g/dl.
Figure 1a: Push enteroscopy/endoscopy showing a large fungating mass found in the proximal jejunum.
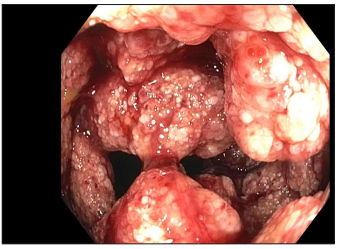
Figure 1b: By gross evaluation, 7.3 x 3.0 cm tanred polypoid soft friable mass.
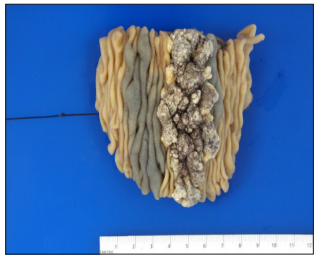
Figure 1c: By histology, a benign proliferation of lymphatic and vascular channels, primarily involving the mucosa and submucosa, but also extending into muscularis propria. (H&E, 200x magnification).
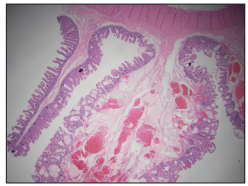
Figure 1c: One lymph node exhibits marked sinusoidal and perinodal lymphangiectasia. (H&E, 400x magnification).
Discussion
From literature search, this is a rare case of jejunal lymphangioma diagnosed by push enteroscopy/endoscopy. There are several prior reports of jejunal lymphangioma mostly diagnosed by double-balloon enteroscopy and Sonde endoscopy [1-3]. Our case highlights the role of push enteroscopy/endoscopy for the diagnosis of proximal jejunal lesions that can lead to significant small-bowel bleeding, protein-losing enteropathy and intussusception.
References
- Hsu SJ, Chang YT, Chang MC, Yu SC, Lee JC, et al. (2007) Bleeding jejunal lymphangioma diagnosed by double balloon enteroscopy. Endoscopy 39: E5-E6.
- Barquist ES, Apple SK, Jensen DM, Ashley SW (1997) Jejunal lymphangioma. An unusual cause of chronic gastrointestinal bleeding. Dig Dis Sci 42(6): 1179-1183.
- Soontornmanokul T, Angsuwatcharakorn P, Viriyautsahakul V, Rerknimitr R, Pantongrag-Brown L, et al. (2012) Jejunal lymphangioma: Rare case of GI bleeding. Gastrointest Endosc 76(4): 884-886.
© 2020 Johannes Koch. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






