- Submissions

Full Text
Gastroenterology Medicine & Research
Adrenal Incidentaloma: A Diagnostic Dilemma
Arcelia Guerson Gil1*, Pawan Rastogi2, Saeed Asiry3 and Sammy Ho4
1Internal Medicine, Jacobi Medical Center, USA
2Gastroenterology, Montefiore Medical Center, USA
3Pathology, Montefiore Medical Center, USA
4Gastroenterology, Montefiore Medical Center, USA
*Corresponding author: Arcelia Guerson Gil, MD, Internal Medicine, Jacobi Medical Center, USA
Submission: February 14, 2020;Published: February 24, 2020

ISSN 2637-7632Volume4 Issue3
Abstract
Adrenal incidentalomas (AI) are most commonly harmless detected through imaging procedures done for unrelated reasons. Some, if left untreated can have significant consequences. This in turn poses for the caring physician a dilemma as to whether or not to pursue a biopsy. As of now, surgery has been the only feasible diagnostic approach. Here, AI was successfully biopsied via EUS-FNA, which resulted in diagnostic yield. This case is important in that it highlights the use of endoscopic ultrasonography (EUS) with fine needle aspiration (FNA) as an alternative modality.
Keywords: Adrenal incidentaloma; EUS-FNA; Malignancy; Endoscopic ultrasonography; Fine needle aspiration
Introduction
Adrenal incidentalomas (AI) are most commonly benign and hormonally inactive, detected through imaging procedures done for unrelated reasons. The challenge is recognizing and treating the small percentage of AI that do pose a significant risk, either because of their malignant potential or because of their hormonal activity. We present an interesting case where an AI suspicious for metastatic disease was successfully biopsied by endoscopic ultrasonography (EUS) with fine needle aspiration (FNA).
Case Presentation
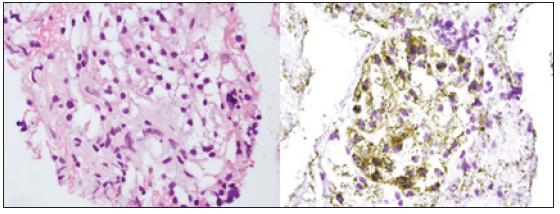
71-year-old African American woman recently diagnosed with poorly differentiated invasive ductal carcinoma of the left breast was found to have a 2cm left adrenal nodule on abdominal CT scan raising concern for metastasis (Figure 1). While the patient remained largely asymptomatic, discussion at our institution’s Multidisciplinary Tumor Board resulted in continued suspicion for a metastatic process. The gastroenterology team was then involved, and an EUS was conducted, revealing a round hypoechoic lesion in the left adrenal gland (Figure 2). FNA for cytology was successfully performed with cytology results being negative for malignant cells. Further, immunohistochemical staining confirmed benign adrenocortical tissue (Figure 3).
Figure 1: Contrast-enhanced computed tomography (CT) showed a new 2.5 x 1.5cm left adrenal nodule.
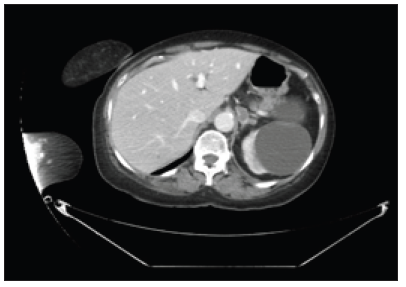
Figure 2: A round hypoechoic mass was identified endosonographically in the left adrenal gland. The mass measured 25mm in maximal cross-sectional diameter. Borders were well-defined.
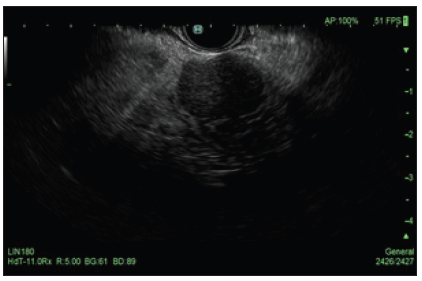
Figure 3: (Left) Adrenal EUS-FNA (Cell block): High power view (400X) of benign adrenocortical cells with bland round to oval nuclei and vacuolated cytoplasm. (Hematoxylin and Eosin stain) (Right) Adrenal EUS-FNA (Cell block): High power view (400X) of benign adrenocortical cells with Melan-A positive cytoplasmic granular staining. (Immunohistochemistry).
Discussion
Although most AI are harmless, some, if left untreated may lead to significant pathological processes [1]. This, in turn, proposes a dilemma for the physician as to whether or not to pursue a biopsy. Obtaining tissue diagnosis results in a significant burden on the overall health care system. Furthermore, a high probability exists that biopsy results may not alter the overall management of patient’s care. On the other hand, failure to identify a malignancy (or metastasis in our case) can be detrimental to the patient’s care. Prior studies have suggested that advanced age is associated with increasing frequency of adrenal masses, ranging from <1% among individuals less than 30 years of age to about 7% in those 70 years of age or older [2]. The optimal strategy for hormonal screening of a patient with AI is unknown. Up to this point, surgery has been the only definitive diagnostic and therapeutic approach [3]. Here we present a case where AI was successfully biopsied via EUS-FNA, resulting in diagnostic yield. This case highlights the use of EUSFNA as an alternative modality, and effective middle ground, for the evaluation of AI.
References
- Tsuji T, Sun T, Sugiyama A, Amano S, Mano T, et al. (2019) Endoscopic treatment of pancreatic diseases via duodenal minor papilla:135 cases treated by sphincterotomy, endoscopic pancreatic duct balloon dilation and pancreatic stenting. Ann of Clin Gastrointest and Hepato 3(1): 012-019.
- Chavan R, Kalapala R, Nabi Z, Lakhtakia S, Reddy DN, et al. (2017) Reverse sphincterotomy of the minor papilla via the major papilla for chronic pancreatitis with incomplete pancreas divisum. Endoscopy 49(1): E119-E120.
© 2020 Tadao Tsuji. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






