- Submissions

Full Text
Gastroenterology Medicine & Research
Hepatic Lymphoma
Jasim Radhi*
Laboratory Medicine, Canada
*Corresponding author: Jasim Radhi, Laboratory Medicine, Lake ridge Health, Oshawa, Ontario, Canada
Submission: March 13, 2018 ;Published: June 01, 2018

Volume1 Issue4 June 2018
Abstract
The liver is more commonly involved by lymphoma as part of the dissemination of the disease. However primary hepatic lymphoma is very rare and account for less than 1% of the extra nodal lymphoma. This represents a lympho proliferative disorder which is confined to the liver and no involvement of lymph node, bone marrow or spleen. The disease can affect immune compromise patient and patient on immune suppressive medication, and less commonly has been described in association with collagen vascular diseases, chronic hepatitis C, B, and EBV infection [1].
Introduction
Primary hepatic lymphoma is very rare in contrast to secondary involvement of the liver which is more common. The diagnosis of primary lymphoma is based on liver involvement with no distant lymphadenopathy and in the absence of leukemic blood manifestation or bone marrow involvements and no detection of disease during radiology staging [2]. Most studies found that the most common presentation of the disease is male predominance with abdominal pain and discomfort. Management options include surgery, chemotherapy, radiation or combination. The prognosis is generally poor and influence by age, constitutional symptoms and elevated liver enzymes [1,2].
Clinical presentation and imaging
Usually patients are middle-age presented with abdominal pain weight loss, fever, fatigue, jaundice, hepatomegaly or nonspecific manifestation or even symptomless. Liver function tests are variable and can be abnormal or sometime within normal limits. The radiological findings can be challenging and often mistaken with hepatocellular carcinoma, metastatic disease or amyloidosis. A CT scan may show single of multiple hypo dense nodules in the liver. The liver involvement can also be diffuse in certain type of lymphoma. Solitary lesion is the most common radiological finding and shows hypo echoic mass resembling cyst or abscess and multifocal lesions carry the differential diagnosis of tuberculosis, fungal infection, septic emboli and metastatic diseases. Therefore there are no pathognomonic diagnostic imaging features [3,4].
Pathological assessment
The most accurate method of diagnosis of hepatic lymphoma is biopsy, which can be used for staging of the disease in Hodgkin and non-Hodgkin lymphoma. The challenges facing the reading pathologist includes representative sample, adequate biopsy material for special studies, and proper clinical history and investigation results. Image guided fine-needle aspiration is another way for diagnosing liver involvement by lymphoma. These are more challenging due to small size of the sample. Many factors involve in the diagnostic yield of fine needle aspiration like the skill and the experience of radiologist and pathologist and the application of ancillary studies.
Most published series found that the most common type of hepatic primary lymphoma is diffuse large B-cell lymphoma, comprising 45% of the cases, followed by Burkitt lymphoma, lymphoblastic lymphoma, follicular lymphoma MALT lymphoma mantle cell lymphoma and T-cell lymphoma [1]. The cells are large with vesicular nuclei and prominent nucleoli. (Figure 1) from a hepatic mass biopsy is showing poorly differentiate malignant cells. This is required the application of proper immunohistochemical markers including CD45, CD20, CD5, CD10, CD79a, CD30, cyclin D, bcl2 and bcl6. The panel reveals lymphoma cells as the tumor cells were positive for CD45 lymphocyte marker. The cells were predominantly expressing CD20 (Figure 2), which is B-cell marker and support a diagnosis of large B cell lymphoma. Some subtypes of lymphoma like T-cell rich-B cell required molecular studies to establish the accurate diagnosis. Chronic lymphocytic leukemia/ small lymphocytic lymphoma tend to show portal infiltration. Other lymphoma type may show predominant diffuse infiltration [3-5].
The liver is more commonly involved as part of systemic dissemination of lymphoma or leukemia. Hodgkin and non- Hodgkin lymphoma can produce nodular hepatic lesion or diffuse infiltration of the liver [6]. Low grade lymphomas require good clinical history and application of immunohistochemistry marker and or flow cytometry to establish the diagnosis and differentiate these from reactive lymphoid cells (Figure 3). The management of patients with primary lymphoma reported in the literature is different from case to case and involves radiation, chemotherapy and surgical excision of localized lesion or combination [1].
Figure 1:High grade lymphoma mass lesion biopsy.
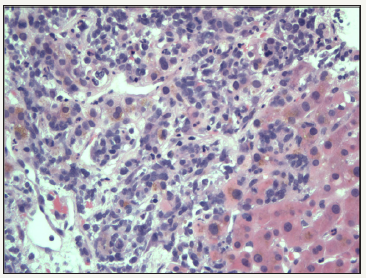
Figure 2:B cell marker CD20 expression.
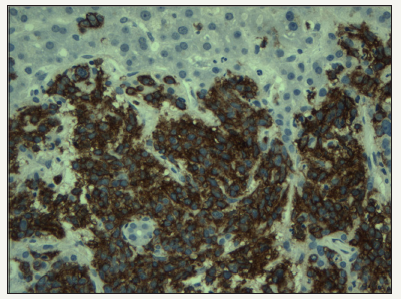
Figure 3:Low grade lymphoma with rather diffuse involvement of the liver.

Conclusion
References
- Myoteri D Dellaportas D, Arkoumani E, Marinis A, Zizi-Sermpetzoglou A (2014) Primary hepatic lymphoma: A challenging diagnosis. Case Reports in Oncologic Medicine.
- Ugurluer G, Miller RC, Li Y, Thariat J, Ghadjar P (2016) Primary Hepatic Lymphoma: A Retrospective, Multicenter Rare Cancer Network Study. Rare Tumors 8(3): 6502.
- Rajesh S, Bansal K, Sureka B, Patidar Y, Bihari C, et al. (2015) The imaging conundrum of hepatic lymphoma revisited. Insights into Imaging 6(6): 679-692.
- Padhan RK, Das P, Shalimar (2016) Primary hepatic lymphoma. Trop Gastroenterol 36(1): 14-20.
- Zentar A, Tarchouli M, Elkaoui H, Belhamidi MS, Ratbi MB, et al. (2014) Primary hepatic lymphoma. J Gastrointest Cancer 45(3): 380-382.
- Loddenkemper C, Longerich T, Hummel M, Ernestus K, Anagnostopoulos I, et al. (2007) Frequency and diagnostic pattern of lymphomas in liver biopsies with respect to WHO classification. Virchows Arch 450(5): 493- 502.
© 2018 Jasim Radhi. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






