- Submissions

Full Text
Global Journal of Endocrinological Metabolism
Prophylactic Use of Vitamin D to Maintain a Robust Immune System Against Infections Like SARS-CoV-2
Sunil J Wimalawansa*
Department of Medicine, Cardio Metabolic & Endocrine Institute, NJ, Brunswick, USA
*Corresponding author: Sunil J. Wimalawansa, MD, PhD, MBA, DSc Prof of Medicine, Department of Medicine, Cardio Metabolic & Endocrine Institute, NJ, Brunswick, USA
Submission: January 10, 2023; Published: March 13, 2023

ISSN 2637-8019Volume3 Issue4
Abstract
The robust activity of the human immune system depends on adequate concentrations of D3 and 25(OH) D- substrates for generating calcitriol within immune cells. This is crucial for maintaining a robust immune system, overcoming infections, and preventing hyper-immune syndromes and autoimmunity. As described in this paper, the most cost-efficient way to curb infections-infectious epidemics, endemic states, or pandemics-is to maintain the population’s immunity via vitamin D sufficiency. Such naturally robust immune system can be maintained through safe daily sun exposure and/or vitamin D supplements, as described here. Approximately 75% of immune cell activities are dependent on vitamin D. While the dietary vitamin D intakes are too low, a balanced diet rich in vitamins (B and C), minerals/ions (e.g., magnesium, zinc, selenium, etc.), and antioxidants (mostly provided via colored green leaves and nuts), helps bolster the immune system. These micronutrients work synergistically in maintaining the functions of the immune system. Besides, when a robust natural immunity of the population is maintained, other than those traditional immunizations, there is no necessity for most vaccines. This would improve health, have fewer adverse effects, less hospitalization, and save costs to taxpayers. Despite ample evidence, no health agency has taken steps to achieve such, even though this approach would cost less than 0.1% of any patented COVID medications or vaccines. Adhering to discussed methods could significantly reduce hospitalization from sepsis/infections by several orders of magnitude and reduce the prevalence and healthcare costs associated with several common chronic diseases.
Keywords: 25(OH)D; 1,25(OH)2D; Immune system; Mutations; Omicron; SARS-CoV-2
Introduction
The immune system comprises a network of intricately regulated biological processes comprising organs, a variety of cells, cellular interconnections, signaling molecules, and many secretory molecules (e.g., cytokines) designed to protect the organism. The immune system is strengthened, primarily with a balanced diet rich in vitamins, minerals, and antioxidants. Therefore, it is crucial to maintain such supplies for a robust immune system to overcome infections. Conversely, deficiency of essential micronutrients impairs immunity and leads to many health conditions, including autoimmune disorders and higher infection risks.
Vaccinations, booster doses, expensive antiviral medications, and monoclonal antibodies have been experimented with in COVID-19 but failed to prevent outbreaks or stop disease and deaths from SARS-CoV-2. During the first two waves of the pandemic, most people who developed complications and died, such as the elderly, those with comorbidities, institutionalized persons, and dark-skin persons living in temperate counties, had severe vitamin D deficiency. Therefore, it is logical to provide them with what they primarily lackedvitamin D supplements. This could have been achieved by targeting the population’s vitamin D sufficiency. This article discusses cost-effective, practical approaches to control and eradicate the COVID-19 pandemic.
Why are People White in Northern Regions and those Living Near the Equator Black?
The melanin pigment evolved in human ancestors who resided close to the equator to protect against potential damage from intense ultraviolet rays from the sunlight. Higher melanin content, however, limits the amounts of vitamin D generation in the skin, their natural environment-outdoor living compensated for the reduced vitamin D synthesis. Nevertheless, when they started to migrate north from central Africa, seeking better pastures for food, they began to receive lesser sunlight exposure. Having a darker skin color became a significant survival disadvantage- they were subjected to more diseases, had shorter survival, and less procreation. Those who developed mutations that reduced expression of the melanin gene developed a lighter skin color. Consequently, they had a greater survival advantage (hence the natural selection) in environments with less sunlight. A similar situation is observed currently-those with darker skin color (Black, Asian, and Minority Ethnic groups) [1], living in highly polluted environments or higher latitudes, and living and working indoors (sedentary lifestyles), had the highest death rates from COVID-19 [1,2]. They all had a common denominator-a high prevalence of severe vitamin D deficiency-low circulating vitamin D and 25(OH)D concentrations that weaken the immune system, increasing vulnerability [3,4]. Consequently, they were more prone vulnerable to chronic diseases like hypertension, diabetes, obesity, and infections, including COVID-19, and its consequences.
For those living in temperate/higher latitude countries, having a lighter skin color alone would not protect them from vitamin D deficiency and related disorders. For example, while those with an African heritage living in temperate countries like the UK had the highest death rates [1,5,6]. The death rates among whites were also higher than those living in tropical countries [7,8]. In addition to the increased prevalence of (auto)immune-related disorders, including multiple sclerosis, rheumatoid arthritis, and Chron’s diseases, the rates of acute respiratory infections are also higher because of insufficient sun exposure and consequent higher prevalence of vitamin D deficiency [9].
Mentioned disorders are more prevalent in those who live far from the equator, especially those in the northern hemisphere [5], unless they take vitamin supplements or regularly eat fatty fish, as with Scandinavians [10,11]. Because of the latter, during the first two waves of the COVID pandemic in 2020, Nordic countries had low COVID-related hospitalizations and deaths even without lockdowns and restrictions [12]. Other factors also increase vulnerability to chronic diseases and infections, such as environmental (air) pollution [13]. However, there is no scientific evidence that ‘climate change’ had any impact on rates of infections, including the spread of COVID-19.
Immune Deficiency, Vaccination, and Viral Mutations
Gene mutations occur randomly, primarily due to transcription errors; some mutants become dominant due to their higher infectiousness. Mutations and contagiousness accelerate in parallel with large-scale immunization programs, especially those using limited-capacity, narrow-spectrum vaccines, like mRNA vaccines [14]; these manifest as new mutants [15]. While the dominant Omicron variants, such as BQ.1.1 and XBB1.5, are more infectious but have become less virulent [16-18]. However, they have developed immune evasion capabilities [17,19]. Repeated booster doses lead to immune paresis with less production of neutralizing antibodies [20]; in conjunction with immune evasion, they become resistant to vaccines and antiviral agents [18,19,21]. mRNA-based COVIDvaccines generated limited immunity that lasted approximately six months. The effectiveness of the resultant neutralizing antibodies (also therapeutic monoclonal antibodies) faded away with immune evasion of new mutant viruses (e.g., BQ and XBB). The protection against complications from SARS-CoV-2 became significantly less with more booster doses (i.e., to less than 30% efficacy) [20]. Therefore, unsurprisingly, outbreaks continue in countries with the highest COVID-vaccine uptakes, like the USA, Israel, etc.
Continuing COVID Outbreaks
The endemic spread and outbreaks continue to occur as local transmission and through travelers via new variants like the B.1 and XBB series of mutants that evade vaccine-induced immune recognition [19,21]. From biological and evolutionary points of view, viruses change their behavior partly to increase the probability of finding new hosts to multiply within and then spread to other hosts. For the same reason, lethality goes down in dominant forms, like Omicron, to minimize the host’s deaths while maintaining the capacity to propagate. Suppose the virus becomes too virulent and kills its host, perish with the host and get eliminated: therefore, developing extreme virulence is counterproductive for the virus. This explains why new dominant variants (mutants) are becoming milder but incresed their ability to spread. Therefore, relatively milder mutant viruses like Omicron. Consequently, it became dominant and overcame the laboratorygenerated, original SARS-CoV-2. Most of the mutants are generated in immune-deficient or fully vaccinated people [22]. The higher the number of booster vaccine doses, the higher the likelihood of getting infected. The resultant weakening of the immune system increases the vulnerability to SARS-CoV-2 and its mutants [23], reinfections [24], and infections with dormant and commensal organisms (e.g., mycobacterium tuberculosis, RSV, herpes zoster, hemolytic streptococcus, candida albicans, etc.) [25]. This seems partly due to vaccine-induced immuno paresis [26]; the host’s immune system malfunctions for an extended period. Meanwhile, the mutation rate continues to increase in individuals with higher vaccine uptake and booster doses in highly vaccinated communities.
Having a Robust Immune System Reduces Rates of Infection and Death
Low vitamin D status is a risk factor for non-communicable [27] and communicable-infectious diseases [28], especially acute respiratory tract infections [29,30]. Vitamin D is a known immunomodulator that boosts innate and adaptive immune systems through multiple mechanisms [31,32]. In addition to stimulating the formation of neutralizing antibodies, vitamin D sufficiency also enhances other antiviral properties-enhancing the production of antimicrobial peptides and autophagy and dampening inflammatory responses. The latter works partly through down-regulating the renin-angiotensin axis and inflammatory cytokines [32,33]. It is necessary to maintain D3 and/or 25(OH)D concentration-the two precursor molecules of calcitriol-above 50ng/mL for a robust immune system [34,35]. Maintaining such levels will counteract pathogenic microbes and minimize complications and deaths from infections [35], including COVID-19 [36,37]. The serum 25(OH)D concentration is inversely correlated with the severity and rates of death from COVID-19. The goal is to maintain serum 25(OH)D concentrations above 50ng/mL to maintain the immune system on high alert to overcome infections such as COVID-19. In many countries, two years of intermittent COVID lockdowns increased the prevalence of vitamin D deficiency, obesity, and poverty-associated malnutrition, worsening clinical outcomes from infections like SARS-CoV-2 [26,27].
Boosting the Immune System with Vitamin D
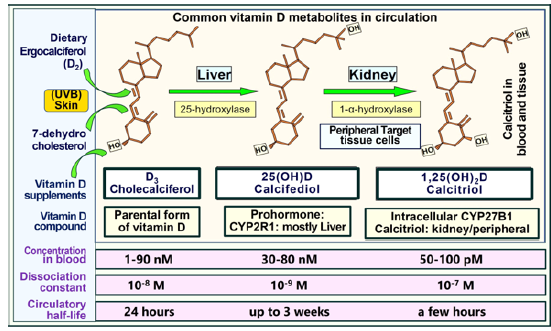
Strategies for eradicating SARS-CoV-2 include reducing viral survival outside the hosts, preventing infection, reducing virus entering human cells via ACE-2 receptors, intracellular viral replication, curtailing viremia, and the inactivation and elimination of viruses from the body. Approximately 75% of the biological activities of the immune system depend on having an intracellular generation of calcitriol in sufficient quantities. Figure 1 illustrates the biologically important three vitamin D metabolites. The sites of hydroxylation, the circulatory concentrations, half-lives, and dissociation constants of the clinically relevant and the most common three vitamin D metabolites are illustrated. Noticeably, D3 and 25(OH)D3 circulate in the bloodstream in nanomolar concentrations. In contrast, 1,25(OH)2D is in the picomolar range-approximately a thousand-fold lesser concentration, which is insufficient to enter peripheral target cells (adapted from Wimalawansa SJ et al. Nutrients, 2022 [33]). This beneficial cycle is initiated when the circulating 25(OH)D is maintained above 50ng/ mL [33], facilitating its diffusion into immune cells generating calcitriol [35]. The latter permits autocrine and paracrine local signaling, which is crucial for immune cells’ physiological and biological activities. These include stimulating innate and adaptive immune systems and suppressing the expression of inflammatory cytokines [38-41]. Maintaining vitamin D sufficiency is the most effective way to sustain a robust immune system.
Figure 1: The biologically important three vitamin D metabolites.
Once calcitriol is locked with its receptor, VDR, it is translocated to the nucleus and modulates immune-related genes. The CYP27B1 enzyme that converted calcifediol to calcitriol: VDRs are highly expressed in immune cells, like macrophages, monocytes, T and B cells, Natural Killer (NK) cells, and dendritic cells [40,41]. Through the Vitamin D Response Element (VDRE), calcitriol/VDR complexes regulate many target genes involved in the immune response, enhancing their ability to overcome infections [39,40]. Many observational and a few Randomized Control Clinical Studies (RCTs) have demonstrated that serum 25(OH)D concentrations are inversely correlated with the severity from COVID-19 [42-44]. Analysis of recent six RCTs (n=551) demonstrated that in persons with COVID-19, serum 25(OH)D concentrations are inversely correlated with less severity from COVID-19 (RR=0.60, 95%; CI 0.40 to 0.92; p=0.02). Similarly, the rate of PCR positivity was reduced in vitamin D intervention groups compared to non-vitamin D groups (RR=0.46; 95% CI 0.24 to 0.89; p=0.02) [45].
Daily and Weekly Maintenance Dose
Maintaining those above-mentioned therapeutic 25(OH) D concentrations between 40 and 80ng/mL can be achieved by longer-term daily intake of vitamin D 5,000 IU (0.125mg) (between 4,000 and 8,000 IU)/day, or 50,000 IU every tenth day (or once a week), for a 70kg (non-obese) person [33]. In contrast, those taking anti-epileptic or anti-retroviral agents that increase the activity of the P450 catabolic enzyme, 24-hydroxylase (CYP24A1), having gastrointestinal fat malabsorption, or being overweight or obese, require two to fourfold higher vitamin D3 intake than those mentioned above [33,35,46]. However, even with the mentioned daily maintenance doses, raising circulatory 25(OH) D concentrations to an adequate therapeutic level will take a few months [33]. In persons with vitamin D deficiency [serum 25(OH) D concentrations <20ng/mL], mentioned doses might not achieve the therapeutic level necessary to prevent or overcome infections [33]. Such individuals require higher upfront loading doses to replenish their depleted body stores before sustainably increasing serum 25(OH)D concentrations [33,47]. A recent article describes easy-to-use tables for calculating the vitamin D doses needed when serum 25(OH)D concentrations are known or using body weightbased calculations [33].
Upfront Loading Doses of Vitamin D
Because of extensive deficits, the use of mentioned daily doses of vitamin D in those with vitamin D deficiency unlikely to reach therapeutic serum levels. For them, an upfront loading (i.e., a bolus) dose of vitamin D, between 100,000 IU and 4000,000 IU, as a single or divided dose, would lead to a rapid increase of circulatory 25(OH)D concentration [47]. Even with such high doses, achieving it takes about three days [33,35,46,48]. The body weightbased proper doses are published in Nutrients [33]. For 25(OH)D formation, vitamin D must be 25-hydroxylated in the liver-a ratelimiting enzymatic step. Therefore, even with the above-mentioned larger dose, it would take two to four days to raise serum 25(OH) D concentrations above 50ng/mL [33]. Therefore, using vitamin D a loading dose in medical emergencies, like COVID-19 infection or sepsis, is not ideal. In those acutely ill or intensive care units, it could take up to a week to elevate their serum 25(OH)D concentrations to the target range [35].
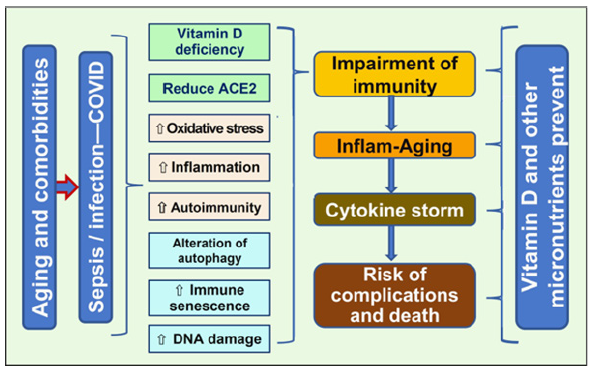
While repeated administration of high doses of vitamin D is counterproductive, there is no evidence that a single dose of vitamin D3 up to 500,000 IU, downregulating CYP27B1, which negatively affects the conversion of 25(OH)D to calcitriol or upregulating CYP24A1 that catabolize 25(OH)D and 1,25(OH)2D [33,34,40,41], or any other undesirable known effects [22,35,36]. In addition, micronutrients, such as zinc, quercetin, magnesium, omega-3 fatty acids, etc., also help optimize the functions of the immune system. These elements are necessary for activating cofactors in several enzymes, the biological activity of hormones, and calcitriol-receptors interactions [27-30]. Vitamin D and supporting micronutrients have a significant impact on the immune system. It prevents the dysfunction of the immune system and cytokine storms, thereby impeding complications and death from SARSCoV- 2 and other enveloped viruses (Figure 2).
Figure 2: Schematic illustration of the global effects of vitamin D in preventing immune dysregulation, preventing complications, and deaths from infections.
Ways to Raise Circulating 25(OH)D Levels in Emergencies
In emergencies like SARS-CoV (becoming PCR-positive, symptomatic, and admitted to a hospital, developing complications, acute post-vaccination complications, etc.), administering a single oral dose of 0.5 to 1mg of calcifediol (~0.014mg/kg body weight) is a reasonable option to rapidly raise serum 25(OH)D concentration and boost the immune system [33]. Since calcifediol does not require 25-hydroxylation in the liver and is absorbed into the portal vein and the circulation directly, bypassing the lymphatic system, 25(OH)D concentrations increase rapidly, and the immune system is boosted within a day [33]. Prompt administration of the bodyweight- based correct dose of calcifediol would significantly reduce complications and deaths from COVID-19. Several observational and RCTs have demonstrated the efficacy of vitamin D and calcifediol in these situations (pre-infection or on admission) [49- 52]. The most practical option is administering a single dose of calcifediol (25-hydroxylated vitamin D) to raise serum 25(OH)D concentrations rapidly to above 50ng/mL within four hours [33]. This regimen has no adverse effects [52,53] and boosts the immune system within a day to combat invading organisms [49,54]. In emergencies like hospitalizationsor becoming PCR positive, it is best to administer the body-weight-abased proper loading doses of D3 together with calcifediol, published as body weight-based vitamin D and calcifediol dose regimens [33]
Strategies for Raising Population Vitamin D Sufficiency
The goal for achieving the population’s vitamin D sufficiency is maintaining serum 25(OH)D concentrations above 40ng/mL (100nmol/L). Adequate daily exposure to the summer-like sun facilitates achieving this without cost. Daily exposure of a third of the surface area of the skin to direct sunlight for 30 to 60 minutes can be generated over 2,000IU up to a maximum of 10,000IU [55,56]. Besides sun-exposed mushrooms and fatty fish, food contains little vitamin D. However, for most individuals who do not have this opportunity for adequate daily sun exposure, vitamin D supplementation is the best strategy to advance [33,57]. A population with vitamin D sufficiency would allow individuals to generate and maintain a robust immune system. When vitamin D sufficiency is maintained, viruses running out of hosts to infect and replicate naturally compromise the survival of the virus without increasing the rate of mutations: thus, gradually eliminating it from the community and the globe. This naturally creates a state like the traditional “herd immunity” concept via global immune sufficiency. The cost of achieving this is only a small fraction of patented anti- COVID medications or vaccines. Maintaining the population’s vitamin D sufficiency is straightforward: it costs less than 0.1% of any patented COVID medications or vaccines. Despite the evidence, no healthcare-related agencies like CDC and WHO have taken steps or are willing to implement such cost-effective programs [58].
The Importance of Maintaining Population Vitamin D Sufficiency
Population serum 25(OH)D concentrations during winter are reduced, weakening individual’s the immune system. With the increased winter-associated cold and dryer indoor weather conditions in conjunction with the high prevalence of hypovitaminosis D, unsurprisingly, the virulence of SARS-CoV-2 increases during the peak of winter. The efficacy of COVID vaccines is dwindling, partly due to Spike protein-related viral mutations and associated immune evasion. However, mutated variants do not impair the efficacy of repurposed agents like vitamin D and ivermectin. Consequently, the recommended vitamin D and ivermectin doses remain the same as the preventative and adjunct therapies. Suppose governments worldwide had spent 1% of the costs paying for vaccines for their country-wide vitamin D supplementation program to enhance and maintain a robust population immunity. It could have brought the pandemic to an end in 2020 or 2021. This course of action would have been sufficient for eradicating the virus from the earth without the reliance on vaccines or herd immunity, which both failed. Such an approach is equivalent to generating and maintaining worldwide natural herd immunity simultaneously, facilitating the eradication of the SARSCoV- 2 virus and the pandemic.
In the interim, vitamin D sufficiency would have markedly reduced the need for hospitalization and ICU use and the severity and deaths from COVID-19, reducing the incidence and severity of several chronic health conditions [59,60]. In addition to millions of lives lost, these measures would have saved billions of dollars in healthcare costs that would have easily offset the cost of achieving global vitamin D sufficiency.
Global Population Immunity Could Eradicate SARS-CoV-2
The most cost-effective way to curtail the pandemic-now an endemic-is to raise the population’s immunity as described abovemaintaining a naturally robust immune system through vitamin D supplements and safe sun exposure guidance [37,61]. However, no health agencies have taken even the first step to achieving that, even though this approach would cost less than 1% of any patented COVID medications or vaccines [58]. The costs associated with hospitalization are several orders of magnitude higher. Along with the rapidly spreading Omicron variants and post-infectious natural immunity, a globally coordinated effort using vitamin D is still feasible to eradicate SARS-CoV-2 in 2023. However, no big pharma, leading health agencies, or administration are not interested in this approach due to conflicts of interest, as eradicating SARS-CoV-2 would not economically benefit them.
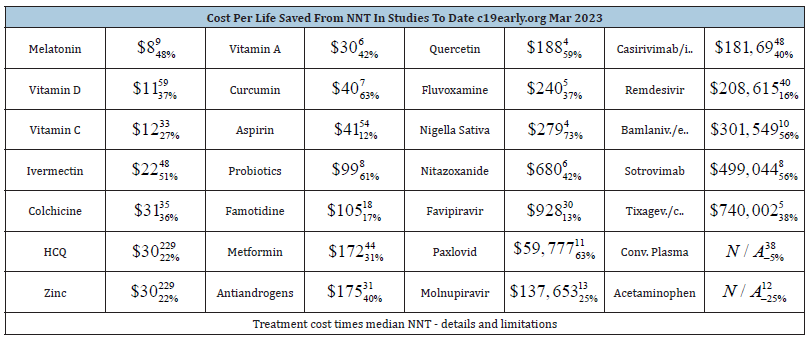
When higher population immunity is attained through vitamin D sufficiency-even when infected with the SARS-CoV-2 mutantsthe virus fails to replicate in adequate numbers to infect others (i.e., low Ro) [8]. Unlike vaccination-derived narrow immunity, the robust immunity generated via natural means from micronutrients like vitamin D sufficiency is comprehensive. The risk of developing complications or perishing from the virus is significantly less with individual or the population’ vitamin D sufficiency. Several metaanalyses reported that vitamin D is more potent and highly costeffective than all patented antiviral agents, monoclonal antibodies, and vaccines. For example, vitamin D costs about $2 per person to treat (or about $10 per person, per year for prophylactic use). In contrast, patented agents used for COVID cost between $500 to $2,000 per person for a single course of treatment [62,63]. Table 1 summarizes the cost-effectiveness of various agents in preventing hospitalization. (Table 1) confirms the data from others that the most cost-effective medications to overcome SARSCoV- 2 are repurposed therapies administered as soon as possible (the left column). Melatonin (fewer studies), vitamin C, vitamin D, and ivermectin are significantly more cost-effective than all three approved patented antiviral agents (Paxlovid, Molnupiravir, and Remdesivir), preventing hospitalizations and deaths from COVID-19. They also have remarkably fewer adverse effects than patented medications. For example, vitamin D is 36,900- and ivermectin is 18,545 times more cost-effective based on the average cost of an antiviral agent in saving one life. Comparative data are not reported yet for mRNA vaccines (and challenging to integrate due to hidden costs). However, they are estimated to be approximately 12,000 times costlier than vitamin D in saving one life.
Table 1: Cost of medications used for COVID-19 per one life saved: Treatment cost multiplied by the Number of Persons Needed to Treat (NNT) to save one life (from https://c19early.org).
The Use of Vitamin D Analogs, Including Calcifediol
Parental vitamin D (D3) is the best supplement for deficiency, osteoporosis, and maintenance of long-term circulatory 25(OH)D concentration. None of the synthetic vitamin D analogs should be used for these purposes. There are specific indications for using synthetic analogs of vitamin D. For example, 25-hydroxylation is impaired in liver failure, where administration of oral calcifediol (25-hydroxylated vitamin D; [25(OH)D]) is indicated. In emergencies, calcifediol can be lifesaving when used on a body weight base dose (0.014mg/kg body weight) [33]. Considering its relatively long half-life, calcifediol can also be administered once a week as a maintenance dose. Apart from liver failure and rare genetic abnormality with 25-hydroxylase (CYP2R1) enzyme, calcifediol is indicated in emergencies to raise serum 25(OH)D concentration, in infection/sepsis, as in COVID-19, as demonstrated in Table 1 in Wimalawansa SJ, et al. Nutrients, 2022 [33,35].
In contrast, in renal failure and hypoparathyroidism, and in rare genetic abnormalities of activating enzyme CYP27B1; or vitamin D receptors, there is an impairment of synthesis of the hormonal form of calcitriol from tubular cells and elsewhere. In these conditions, one of the activated vitamin D analogs, calcitriol [1,25(OH)2D] or 1α(OH)D analogs or 1,25(OH)2D, is essential to maintain serum Ca2+ and mineral homeostasis [35]. These synthetic analogs are expensive and have low ED50: Thus, they must be used under medical supervision to minimize adverse effects and to obtain optimal results. There are no other common conditions for using these analogs.
Calcitriol Should not be Used for Treating Infections Like COVID-19
The key indications for calcitriol are advanced renal failure (preventing secondary hyperparathyroidism) and hypoparathyroidism with clinically significant hypocalcemia that needs correction [33]. Because of high cost, adverse effects, and minimal benefits, calcitriol and 1α-analogs should not be used in osteoporosis. Beyond those mentioned above, there is no rationale for using synthetic vitamin D analogs: These are expensive and have unjustifiable adverse health risks. Since calcitriol does not get into immune cells, its administration does not benefit from combating infections and should not be used. Irrespective of the route of administration, calcitriol has little or no benefit in infections, including SARS-CoV-2. Since the ED50 is narrow, the potential toxicity is high when calcitriol is used for indications other than advanced renal failure and hypoparathyroidism. Inappropriate use of calcitriol increases the risks of hypercalcemia, hypercalciuria, and serious cardiovascular adverse issues [64]. Unlike in chronic renal failure [65], using calcitriol in infections [66], including patients and subjects in RCTs is unphysiological. Such uses are due to the failure to understand the biology of vitamin D and its interactions with immune cells [66]-how the immune system functions.
Discussion
In pandemics, it is essential to maintain the population’s immune sufficiency through vitamin D adequacy. It is the most cost-efficient way to overcome infectious epidemics and pandemics in conjunction with basic public health measures. This can be achieved and maintained via adequate public education on daily sun exposure and efficient vitamin D supplementation. Not medicine, vaccine, and mandates, but a healthy, robust immune system should be used as internal armor in preventive medicine against infections, especially against SARS-CoV-2, to prevent symptomatic disease, complications, and deaths. Despite the emerging therapeutic paradigms, robust healthy immunity is, undoubtedly, and will always be, the best and the most relevant measure in preventing COVID-19 and other invading pathogens.
Long-term vitamin D repletion and the maintenance of serum 25(OH)D concentrations above 50ng/mL (125nmol/L) is the most cost-effective and practical way to enhance immunity in the population and reduce the prevalence and severity of chronic diseases and mortality [67]. Maintaining a higher serum of 25(OH) D before sicknesses, such as prior to contracting COVID-19 and before vaccination, would significantly reduce complications and deaths. If the population had been supplemented, as discussed here, with adequate doses of vitamin D, and maintain serum 25(OH)D concentrations above 40 ng/mL, the pandemic would have been less severe, One would have observed fewer admissions to hospitals and intensive care units and fewer deaths.
Raising and maintaining the population’s immunity should be a target in any infectious outbreaks, including COVID-19: but this failed to materialize. It would have optimize the immune responses in the population and preferentially generated neutralizing antibodies, prevented adverse effects and autoimmunity reactions following immunization and infections. The post-infection natural immunity that derived from immunization in communities primed with naturally robust immune systems, would have prevented the new mutants like Delta and Omicron and allowed eradication of the SARS-CoV-2 [68] in 2021/21. However, the refusal to recognize natural immunity, non-approval of cost-effective repurposed agents, and misguiding by leading health authorities, prevented achieving them.
Conclusion
The current medical system, and scientific methodologies, are highly compartmentalized. Thus, physicians and scientists in this system failed to understand the biology of the virus and micronutrients, particularly vitamin D, and their intricate relations with the immune system. In addition, many who advise administrations and policymakers are directly or indirectly remunerated by big pharma, such as advisory board members, recipients of research grants, and journal editors, were biased toward vaccines. Consequently they provided improper and conflicted advices which continues. In conjunction with widespread conflicts of interest among decision-makers, prioritizing business interests, and exclusive reliance on vaccines, the world failed to eradicate SARS-CoV-2. Meanwhile, none of the COVID vaccines prevented SARS-CoV-2 transmission; thus, the concept and the coercion for vaccine passports and the recent deceitful attempts by the self-appointed world economic forum using the WHO to mandate digital identities are annihilations.
Conflicts of Interest
The author declares no conflicts of interest. He did not receive any funding or writing assistance.
Acknowledgment
The author appreciates the input from Eugene Heyden and Dr. Athula Polonowita.
References
- Aldridge RW, Lewer D, Katikireddi SV, Mathur R, Pathak N, et al. (2020) Black, Asian and minority ethnic groups in England are at increased risk of death from COVID-19: Indirect standardisation of NHS mortality data. Wellcome Open Res 5: 88.
- Holmes L, Enwere M, Williams J, Ogundele B, Chavan P, et al. (2020) Black-white risk differentials in COVID-19 (SARS-COV2) transmission, mortality and case fatality in the United States: Translational epidemiologic perspective and challenges. Int J Environ Res Public Health 17(12): 4322.
- Rhodes JM, Subramanian S, Laird E, Griffin G, Kenny RA (2021) Perspective: Vitamin D deficiency and COVID-19 severity - plausibly linked by latitude, ethnicity, impacts on cytokines, ACE2, and thrombosis. J Intern Med 289(1): 97-115.
- Kakodkar P, Kaka N, Baig MN (2020) A comprehensive literature review on the clinical presentation, and management of the pandemic coronavirus disease 2019 (COVID-19). Cureus 12(4): e7560.
- Ames BN, Grant WB, Willett WC (2021) Does the high prevalence of vitamin D deficiency in African Americans contribute to health disparities? Nutrients 13(2): 499.
- Bianconi V, Mannarino MR, Figorilli F, Cosentini E, Batori G, et al. (2021) Prevalence of vitamin D deficiency and its prognostic impact on patients hospitalized with COVID-19. Nutrition 91-92: 111408.
- Rosario DKA, Mutz YS, Bernardes PC, Conte-Junior CA (2020) Relationship between COVID-19 and weather: Case study in a tropical country. Int J Hyg Environ Health 229: 113587.
- Wimalawansa SJ (2020) Modes of preventing secondary community spread and future epidemics of COVID-19. J Immuno Biol 5(1): 1-5.
- Bellan M, Andreoli L, Mele C, Sainaghi PP, Rigamonti C, et al. (2020) Pathophysiological role and therapeutic implications of vitamin D in autoimmunity: Focus on chronic autoimmune diseases. Nutrients 12(3): 789.
- Sun L, Arbesman J, Piliang M (2021) Vitamin D, autoimmunity, and immune-related adverse events of immune checkpoint inhibitors. Arch Dermatol Res 313(1): 1-10.
- Bossak BH, Turk CA (2021) Spatial variability in COVID-19 mortality. Int J Environ Res Public Health 18(11): 5892.
- Ludvigsson JF (2020) The first eight months of Sweden's COVID-19 strategy and the key actions and actors that were involved. Acta Paediatr 109(12): 2459-2471.
- Ismail IMI, Rashid MI, Ali N, Altaf BAS, Munir M (2022) Temperature, humidity and outdoor air quality indicators influence COVID-19 spread rate and mortality in major cities of Saudi Arabia. Environ Res 204(Pt B): 112071.
- Guerin P, Yahi N, Azzaz F, Chahinian H, Sabatier JM, et al. (2022) Structural dynamics of the SARS-CoV-2 Spike protein: A 2-year retrospective analysis of SARS-CoV-2 variants (from alpha to omicron) reveals an early divergence between conserved and variable epitopes. Molecules 27(12): 3851.
- Cao Y, Yisimayi A, Jian F, Song W, Xiao T, et al. (2022) BA.2.12.1, BA.4 and BA.5 escape antibodies elicited by omicron infection. Nature 608(7923): 593-602.
- Uraki R, Ito M, Furusawa Y, Yamayoshi S, Horimoto KI, et al. (2023) Humoral immune evasion of the omicron subvariants BQ.1.1 and XBB. Lancet Infect Dis 23(1): 30-32.
- Zhang X, Chen LL, Daniel IPJ, Chan WM, Hung IFN, et al. (2023) Omicron sublineage recombinant XBB evades neutralising antibodies in recipients of BNT162b2 or CoronaVac vaccines. Lancet Microbe 4(3): e131.
- Takashita E, Yamayoshi S, Simon V, Bakel HV, Sordillo EM, et al. (2022) Efficacy of antibodies and antiviral drugs against omicron BA.2.12.1, BA.4, and BA.5 subvariants. N Engl J Med 387(5): 468-470.
- Lind ML, Copin R, McCarthy S, Coppi A, Warner F, et al. (2023) Use of whole genome sequencing to estimate the contribution of immune evasion and waning immunity on decreasing COVID-19 vaccine effectiveness. J Infect Dis 227(5): 663-674.
- Schiek WK, Piechotta V, Pilic A, Batke M, Dreveton LS, et al. (2022) Facing the Omicron variant-how well do vaccines protect against mild and severe COVID-19? third interim analysis of a living systematic review. Front Immunol 13: 940562.
- Samanovic MI, Oom AL, Cornelius AR, Gaillard SLG, Karmacharya T, et al. (2022) Vaccine-acquired SARS-CoV-2 immunity versus infection-acquired immunity: A comparison of three COVID-19 vaccines. Vaccines (Basel) 10(12): 2152.
- Wang Q, Iketani S, Li Z, Liu L, Guo Y, et al. (2023) Alarming antibody evasion properties of rising SARS-CoV-2 BQ and XBB subvariants. Cell 186(2): 279-286.e8.
- Shrestha N, Burke PC, Nowacki AS, Simon JF, Hagen A, et al. (2022) Effectiveness of the coronavirus disease 2019 (COVID-19) bivalent vaccine. Preprint: MedRxiv.
- Hwang MJ, Hwang I, Park C, Park H, Son T, et al. (2022) Evaluation of clinical severity according to primary infection variants in patients with suspected SARS-CoV-2 reinfection. Epidemiol Health: e2023007.
- MacIntyre CR, Costantino V, Heslop DJ (2020) The potential impact of a recent measles epidemic on COVID-19 in Samoa. BMC Infect Dis 20(1): 735.
- Aslam S, Isakov LD, Mehra MR (2021) COVID-19 vaccination immune paresis in heart and lung transplantation. J Heart Lung Transplant 40(8): 763-766.
- Autier P, Boniol M, Pizot C, Mullie P (2014) Vitamin D status and ill health: A systematic review. Lancet Diabetes Endocrinol 2(1): 76-89.
- Aibana O, Huang CC, Aboud S, Pena AA, Becerra MC, et al. (2019) Vitamin D status and risk of incident tuberculosis disease: A nested case-control study, systematic review, and individual-participant data meta-analysis. PLoS Med 16(9): e1002907.
- Sabetta JR, DePetrillo P, Cipriani RJ, Smardin J, Burns LA, et al. (2010) Serum 25-hydroxyvitamin d and the incidence of acute viral respiratory tract infections in healthy adults. PLoS One 5(6): e11088.
- Brenner H, Holleczek B, Schottker B (2020) Vitamin D insufficiency and deficiency and mortality from respiratory diseases in a cohort of older adults: Potential for limiting the death toll during and beyond the COVID-19 pandemic? Nutrients 12(8): 2488.
- Zhang Y, Leung DYM, Richers BN, Liu Y, Remigio LK, et al. (2012) Vitamin D inhibits monocyte/macrophage proinflammatory cytokine production by targeting MAPK phosphatase 1. J Immunol 188(5): 2127-2135.
- Rosa MD, Malaguarnera M, Nicoletti F, Malaguarnera L (2011) Vitamin D3: A helpful immuno-modulator. Immunology 134(2): 123-139.
- Wimalawansa SJ (2022) Rapidly increasing serum 25(OH)D boosts the immune system, against infections-sepsis and COVID-19. Nutrients 14(14): 2997.
- Quraishi SA, Bittner EA, Blum L, McCarthy CM, Bhan I, et al. (2014) Prospective study of vitamin D status at initiation of care in critically ill surgical patients and risk of 90-day mortality. Crit Care Med 42(6): 1365-1371.
- Wimalawansa SJ (2022) Overcoming infections including COVID-19, by maintaining circulating 25(OH)D concentrations above 50ng/mL. Pathology & Lab Medicine Int 14: 37-60.
- Rastogi A, Bhansali A, Khare N, Suri V, Yaddanapudi N, et al. (2022) Short term, high-dose vitamin D supplementation for COVID-19 disease: A randomised, placebo-controlled, study (SHADE study). Postgrad Med J 98(1156): 87-90.
- Wimalawansa SJ, Polonowita A (2021) Boosting immunity with vitamin D for preventing complications and deaths from COVID-19. in COVID 19: Impact, mitigation, opportunities and building resilience “From adversity to serendipity,” perspectives of global relevance based on research, experience and successes in combating COVID-19 in Sri Lanka. National Science Foundation, Colombo, Sri Lanka.
- Chun RF, Liu PT, Modlin RL, Adams JS, Hewison M (2014) Impact of vitamin D on immune function: lessons learned from genome-wide analysis. Front Physiol 5: 151.
- Aygun H (2020) Vitamin D can prevent COVID-19 infection-induced multiple organ damage. Naunyn Schmiedebergs Arch Pharmacol 393(7): 1157-1160.
- Bishop E, Ismailova A, Dimeloe S, Hewison M, White JH (2020) Vitamin D and immune regulation: Antibacterial, antiviral, anti-inflammatory. JBMR Plus 15(1): E10405.
- Jeffery LE, Burke F, Mura M, Zheng Y, Qureshi OS, et al. (2009) 1,25-Dihydroxyvitamin D3 and IL-2 combine to inhibit T cell production of inflammatory cytokines and promote development of regulatory T cells expressing CTLA-4 and FoxP3. J Immunol 183(9): 5458-5467.
- Cedillo PEV, Chavolla OYB, Pedraza NR, Encinas BR, Carrión CIP, et al. (2022) Serum vitamin D levels are associated with Iincreased COVID-19 severity and mortality independent of whole-body and visceral adiposity. Front Nutr 9: 813485.
- Kumar P, Kumar M, Bedi O, Gupta M, Kumar S, et al. (2021) Role of vitamins and minerals as immunity boosters in COVID-19. Inflammopharmacology 29(4): 1001-1016.
- DrorI A, MorozovI N, Daoud A, Namir Y, Yakir OO, et al. (2022) Pre-infection 25-hydroxyvitamin D3 levels and association with severity of COVID-19 illness. PloS One 17(2): e0263069.
- Varikasuvu SR, Thangappazham B, Vykunta A, Duggina P, Manne M, et al. (2022) COVID-19 and vitamin D (Co-VIVID study): A systematic review and meta-analysis of randomized controlled trials. Expert Rev Anti Infect Ther 20(6): 907-913.
- Veugelers PJ, Pham TM, Ekwaru JP (2015) Optimal vitamin D supplementation doses that minimize the risk for both low and high serum 25-hydroxyvitamin D concentrations in the general population. Nutrients 7(12): 10189-10208.
- Wimalawansa SJ, Whittle R (2022) Vitamin D: A single initial dose is not bogus if followed by an appropriate maintenance intake. JBMR Plus 6(3): e10606.
- Ekwaru JP, Zwicker JD, Holick MF, Giovannucci E, Veugelers PJ (2014) The importance of body weight for the dose response relationship of oral vitamin D supplementation and serum 25-hydroxyvitamin D in healthy volunteers. PLoS One 9(11): e111265.
- Gomez JMQ, Miranda JL, Castillo ME, Díaz AC, Solans XNY, et al. (2022) Vitamin D endocrine system and COVID-19: Treatment with calcifediol. Nutrients 14(13): 2716.
- Maghbooli Z, Sahraian MA, Jamalimoghadamsiahkali S, Asadi A, Zarei A, et al. (2021) Treatment with 25-hydroxyvitamin D3 (calcifediol) is associated with a reduction in the blood neutrophil-to-lymphocyte ratio marker of disease severity in hospitalized patients with covid-19: A pilot multicenter, randomized, placebo-controlled, double-blinded clinical trial. Endocr Pract 27(12): 1242-1251.
- Castillo ME, Costa LE, Barrios JV, Díaz JA, Miranda JL, et al. (2020) Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study. J Steroid Biochem Mol Biol 203: 105751.
- Diaz JFA, Perez LL, Huelgas RG, Escalante MM, Rodríguez BC et al. (2021) Calcifediol treatment and hospital mortality due to COVID-19: A cohort study. Nutrients 13(6): 1760.
- Negre JMS (2016) Calcifediol soft capsules, W. patent.v
- Negre JS, Azpitarte IO, Barrios PDA, Herrero GH (2016) Calcifediol soft capsules.
- Vieth R (2004) Why the optimal requirement for vitamin D3 is probably much higher than what is officially recommended for adults. J Steroid Biochem Mol Biol 89-90(1-5): 575-579.
- Wimalawansa SJ, Razzaque DS, Daghri NA (2018) Calcium and vitamin D in human health: Hype or real? J Steroid Biochem Mol Biol 180: 4-14.
- Pludowski P, Holick MF, Grant WB, Konstantynowicz J, Mascarenhas MR, et al. (2018) Vitamin D supplementation guidelines. J Steroid Biochem Mol Biol 175: 125-135.
- Wimalawansa SJ (2020) COVID-19: Evolution and prevention. Trends Telemed E-Health 2(3): 1-5.
- Grant WB, Boucher BJ, Pludowski P, Wimalawansa SJ (2022) The emerging evidence for non-skeletal health benefits of vitamin D supplementation in adults. Nat Rev Endocrinol 18(5): 323.
- Wimalawansa SJ (2018) Non-musculoskeletal benefits of vitamin D. J Steroid Biochem Mol Biol 175: 60-81.
- Wimalawansa SJ (2021) Effective and practical ways to overcome vitamin D deficiency. J Family Med Community Health 8(1): 1-8.
- Wimalawansa SJ (2020) Achieving population vitamin D sufficiency will markedly reduce healthcare costs. EJBPS 7(3): 136-141.
- Wimalawansa SJ (2020) Reducing risks from COVID-19: Cost-effective ways of strengthening individual’s and the population immunity with vitamin D. J Endocrinol Sci 2(2): 5-13.
- Tebben PJ, Milliner DS, Horst RL, Harris PC, Singh RJ, et al. (2012) Hypercalcemia, hypercalciuria, and elevated calcitriol concentrations with autosomal dominant transmission due to CYP24A1 mutations: Effects of ketoconazole therapy. J Clin Endocrinol Metab 97(3): E423-427.
- Oristrell J, Oliva JC, Subirana I, Casado E, Domínguez D, et al. (2021) Association of calcitriol supplementation with reduced COVID-19 mortality in patients with chronic kidney disease: A population-based study. Biomedicines 9(5): 509.
- Elamir YM, Amir H, Lim S, Rana YP, Lopez CG, et al. (2022) A randomized pilot study using calcitriol in hospitalized COVID-19 patients. Bone 154: 116175.
- Wimalawansa SJ (2020) Global epidemic of coronavirus-COVID-19: What can we do to minimize risks? European J. Biomed & Pharma Sci 7(3): 432-438.
- Chen J, Liu X, Zhang X, Lin Y, Liu D, et al. (2021) Decline in neutralizing antibody responses, but sustained T-cell immunity, in COVID-19 patients at 7 months post-infection. Clin Transl Immunology 10(7): e1319.
© 2023 Sunil J Wimalawansa. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






