- Submissions

Full Text
Global Journal of Endocrinological Metabolism
The Role of Diet in Normalising Blood Sugar Levels in a Patient with Type 2 Diabetes after a Covid-19 Infection
Rangelova L1* and Nikolova M2
1Department of National Center of Public Health and Analyses, Bulgaria
2Department of Epidemiology and Hygiene, Bulgaria
*Corresponding author: Rangelova L, Department of National Center of Public Health and Analyses, Bulgaria
Submission: May 23, 2022; Published: June 09, 2022

ISSN 2637-8019Volume3 Issue3
Summary
The described case refers to a patient suffering from type 2 diabetes and obesity after a Сovid-19 infection. Despite maintaining high blood glucose levels, the role of diet in normalising some main metabolic parameters is beyond dispute.
Keywords: Covid-19; Diabetes; Obesity; Adult
Introduction
Type 2 diabetes mellitus, known as Non-Insulin Dependent Diabetes Mellitus (NIDDM), is a metabolic disorder characterized by elevated levels of blood glucose in the context of insulin resistance and relative insulin deficiency. Type 2 diabetes cases accounts for 90% of all diabetes cases. The type 2 diabetes development is caused by a combination of genetic and lifestyle risk factors. Although a person cannot change risk factors such as age, female sex or genetics, a patient can control some risk factors such as diet. Obesity is considered a major cause for type 2 diabetes progression in people who are genetically susceptible to the disease. The classic symptoms are extreme thirst, frequent urination and persistent hunger. Diabetes significantly increases the risk of cardiovascular conditions, including high blood pressure, heart attack, stroke, coronary heart disease, atherosclerosis. High blood sugar can result in damage to the nerves, especially in the legs and feet. Diabetes can damage the circulatory system of the kidneys, leading to kidney disease or renal failure. Diabetic retinopathy can cause blindness. In addition, diabetes increases the risk of cataract and glaucoma. Diabetes leads to an increased risk, frequency and more severe course of infections, including Covid-19 [1-3]. Covid-19 infection can cause both the development of newly diagnosed diabetes mellitus and complications of pre-existing disease [4,5]. Potential mechanisms for the development of hyperglycaemia in COVID-19 infection are associated with the available stress response to the severe infection, treatment with corticosteroids, impaired beta-cell function, followed by impaired insulin secretion due to direct acute viral damage to beta cells with expression of elevated levels of pro-inflammatory cytokines [6,7].
Case History
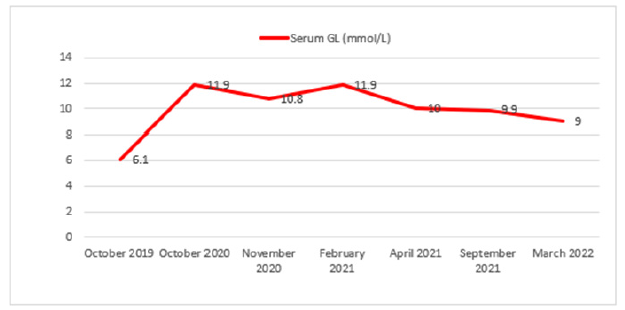
A 55-year-old man with long-standing diabetes and obesity, with repeated dietary nonadherence, with repetitive attempts to reduce body weight with yo-yo effect, orally treated with medication-Eucreas 2x1 tablet, having good control of blood sugar levels (glycated hemoglobin HbA1c 6.0-6.7%), who experienced a Covid-19 infection in October 2020 with a one-day increase in temperature with chills and body aches, without developing symptoms of a respiratory infection. The patient was diagnosed through an antibody test to the covid virus. Routine blood sugar testing on 19th October 2020 revealed fasting serum glucose level of 11.99mmol/L, increased uric acid level-44μmol/L, increased triglycerides-1.80mmol/L and reduced HDL-cholesterol - 0.98mmol/L. As of that date, the patient’s body mass index was 35.2kg/m2. A correction in the drug therapy was made by adding 1 tablet of Metformin at lunch and diet and exercise recommendations. Regular monitoring of blood parameters: serum glucose levels through blood sugar profile and glycated hemoglobin, cholesterol fractions, uric acid, liver enzymes. Although the patient strictly adhered to medication therapy, elevated fasting glucose levels were observed (Figure 1). On 16th November 2021, on the recommendation from the treating endocrinologist, the drug therapy was changed by replacing Eucreas with Synjardy 2x1 tablet of 1000mg and one tablet of Metfogamma of 850mg at lunch. On 28th March 2022, fasting blood sugar level of 9mmol/L was measured in glycated hemoglobin HbA1c-7.3%. As of that date, the patient’s BMI was 31.6kg/m2.
Figure 1:Values of fasting blood sugar of the patient for the period 2019-2022.
Discussion
Since the beginning of the COVID-19 pandemic, people with diabetes have been identified as a risk group. Doctors explain that these patients experience the virus infection with more complications, as the number of hospitalizations is higher. It has been proved that Covid-19 often causes changes in blood sugar levels even in people without diabetes-in other words, new-onset diabetes in patients with COVID-19. In diabetes and Covid-19 cases complications are more common and it takes longer to produce negative test results. Therefore, a discussion on a change in therapy with an emphasis on diet and physical activity is needed [8-11]. Since 16th November 2021 the patient has had to follow a significantly restrictive 3 times, low-carbohydrate diet, excluding all sugar and confectionery, sugar-sweetened soft drinks and alcohol with significantly reduced consumption of bread, potatoes and rice, and sweet fruits. The dinner consisting mainly of vegetables has to be not later than 20pm. Meat and fish are included three times a week. Liquid intake is increased to 2.5-3 liters per day. As of 28th March 2022, the patient lost 13kg weight. Despite the fact that glucose levels remained high, there was an improvement and normalisation of some main metabolic indicators such as HDLcholesterol, uric acid, triglycerides, liver enzymes. As the patient loses weight, his motivation for lifestyle change increases. The goal of the diet in patients suffering from diabetes is to achieve and maintain optimal metabolic outcomes. Blood glucose levels have to be normal or close to normal values. This is essential to prevent the complications which are common in diabetes. Maintaining good lipid profile leads to better vascular health. Maintaining blood sugar levels within normal range is necessary to prevent the risk of cardiovascular events.
Conclusion
The described case of a patient with type 2 diabetes mellitus and obesity after Covid-19 infection demonstrates the role of diet in normalising some main metabolic parameters in the context of nutritional status improvement.
References
- Fadini GP, Morieri ML, Longato E, Avogaro A (2020) Prevalence and impact of diabetes among people infected with SARS-CoV-2. J Endocrinol Invest. 43(6): 867-869.
- Gupta R, Ghosh A, Singh AK, Misra A (2020) Clinical considerations for patients with diabetes in times of COVID-19 epidemic. Diabetes Metab Syndr 14(3): 211-212.
- Guo W, Li M, Dong Y, Zhou H, Zang Z, et al. (2020) Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev p. 3319.
- Li C, Islam N, Gutierrez JP, Lacey B, Moolenaar RL, et al. (2021) Diabetes, obesity, hypertension and risk of severe COVID-19: a protocol for systematic review and meta-analysis. BMJ 11(11): e051711.
- Apicella M, Campopiano MC, Mantuano M, Mazoni L, Coppelli A, at al. (2020) COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol 8(9): 782-792.
- Sathish T, Tapp RJ, Cooper ME, Zimmet P (2021) Potential metabolic and inflammatory pathways between COVID-19 and new-onset diabetes. Diabetes Metab 47(2): 101204.
- Liuliu Y, HanY, Nilsson-Payant B, Gupta V, Wang P, at al. (2020) A Human pluripotent stem cell-based platform to study SARS-CoV-2 tropism and model virus infection in human cells and organoids. Cell Stem Cell 27 (1): 125-136.
- Evert AB, Dennison M, Gardner CD, Garvey WT, Lau KHK, at al. (2019) Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care 42(5): 731-754.
- Franz MJ, MacLeod J, Evert A, Brown C, Gradwell E, et al. (2017) Academy of nutrition and dietetics nutrition practice guideline for type 1 and type 2 diabetes in adults: systematic review of evidence for medical nutrition therapy effectiveness and recommendations for integration into the nutrition care process. J Acad Nutr Diet 117(10): 1659-1679.
- Evert AB, Boucher JL, Cypress M, Dunbar SA, Franz MY, et al. (2014) Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 37(1): 120-143.
- Sainsbury E, Kizirian NV, Partridge SR, Gill T, Colagiuri S, at al. (2018) Effect of dietary carbohydrate restriction on glycemic control in adults with diabetes: a systematic review and meta-analysis. Diabetes Res Clin Pract 139: 239-252.
© 2022 angelova L. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






