- Submissions

Full Text
Global Journal of Endocrinological Metabolism
Relationship between Neutrophil/Lymphocyte Ratio and Cardiometabolic Values in Patients with Prediabetes
Isa Ardahanli1, Mehmet Celik2* and Mümtaz Takir3
1 Department of Cardiology, Bilecik State Hospital, Turkey
2 Department of Endocrinology and Metabolism, Bilecik State Hospital, Turkey
3 Department of Endocrinology and Metabolism, Medeniyet University, Göztepe Training and Research
*Corresponding author: Mehmet Celik, Department of Endocrinology and Metabolism, Bilecik State Hospital, Bilecik, Turkey, Email: drmehmetcelik@hotmail.com
Submission: October 11, 2018; Published: October 24, 2018

ISSN 2637-8019Volume2 Issue5
Abstract
Objective: The neutrophil/lymphocyte ratio (NLR) is associated with atherosclerosis. In many prior studies, the relationship between prediabetes and cardiovascular disease (CVD) has been clearly established. In this study, we investigated the relationship between the NLR in prediabetic patients.
Method: Fifty-three consecutive patients without coronary artery disease who were diagnosed with prediabetes and 48 otherwise healthy subjects were enrolled in the study. Fasting blood glucose levels, HbA1c values and NLR were measured from venous blood samples.
Result: There were no statistical difference between the groups in terms of age, gender, body mass index. In the prediabetic group, the mean blood fasting glucose was 115±4mg/dl, whereas in the control group it was 90±5mg/dl. Mean HbA1c levels was % 5,9±0,4 in prediabetic group, whereas in the control group it was % 5,1±0,3. The NLR, was meaningfully higher in the prediabetic group than control group. Furthermore, there was a significantly positive correlation between the NLR in both the control group and prediabetic group.
Conclusion: In prediabetic group, NLR was detected higher than in healthy subjects.
Keywords: Neutrophil/lymphocyte ratio; Prediabetes
Introduction
Cardiovascular disease (CVD) remains a leading cause of death worldwide. Therefore, prevention of CVD has become a public health precedence. Hyperglycemia is a well-established risk factor for cardiovascular disease [1-3]. Prediabetes is defined as the first stage of diabetes mellitus. According to the definition of American Diabetes Association (ADA), prediabetes is a combination of impaired fasting glucose (IFG), impaired glucose tolerance (IGT) or both and HbA1c is between 5.7% and 6.4% [4]. In previous studies, approximately 25-30% of patients with prediabetes had progressed to DM within 3 to 5years [5]. Neutrophil/lymphocyte ratio (NLR), which can be derived from the white blood cell (WBC) count, is a novel marker of prognosis in patients with cardiovascular disease [6,7]. The neutrophil/lymphocyte ratio (NLR) and epicardial adipose tissue thickness (EAT) are newly established cardiovascular risk markers currently used in the clinical setting. They indicate exposure to long-term risk factors. For this reason, these parameters may provide information on the risk of atherosclerosis in prediabetic patients. In addition, they can help in determining the intensity of the treatment. In this study, the relationship between cardiometabolic values and NLR was evaluated in patients who had been diagnosed prediabetes.
Methods
Inclusion and exclusion criteria
In this prospective study, prediabetic patients matured 18 to 55years who had been admitted to the Cardiology and Endocrinology Department for echocardiography were incorporated into the study. Patients with a fasting blood glucose of 100-125mg/dl were identified as impaired fasting glucose (IFG). Patients with a blood glucose of 140-199mg/dl measured 2hours after OGTT were considered impaired glucose tolerance (IGT). Patients with IFG, IGT, or both (IFG+IGT) constituted the prediabetic patient group. HbA1C levels between 5.7 and 6.4 were identified prediabetic. Fasting blood glucose < 100mg/dl and 2nd hour glucose values < 140 and HbA1C (%)< 5.7 were taken as control group. Exclusion criteria were clinically significant valvular heart disease, congestive heart failure, patient with known coronary artery disease, hematological disease, malignancy, chronic renal disease (glomerular filtration rate of < 60ml/min), liver disease, active infection or systemic inflammatory conditions, autoimmune disease, pregnant women, type1 or 2 diabetes mellitus, obesity (BMI≥30kg/m2) and patients with poor echocardiographic images.
General assessment and measurements
An entire medical history and physical examination were performed and recorded in every one of the cases contemplated. The body weight, waist circumference and body height measured, and body mass index (BMI) was calculated utilizing the following formula: BMI=weight (kg)/height (m²). In terms of abdominal obesity, the smallest waist circumference between the lowest costa and the spina iliaca anterior superior; was measured by measuring the transverse mass parallel to the side of the umbilicus. The waist circumference of ≥88cm for women and ≥102 for men was acknowledged as in expanded waist circumference [8].
Laboratory measurements
Blood samples were obtained from the antecubital vein after the first admission and following a 12hour fasting. Biochemical analyses were performed with an Architect Ci 8200 (Abbott Laboratories, Lake Bluff, IL, USA), Full blood counts were performed with an XN-1000 Automated Hematology Analyzer (Sysmex, Tokyo, Japan), and biochemical analyses were performed with an Architect Ci8200 (Abbott Laboratories, Lake Bluff, IL, USA). Fasting blood glucose, creatinine, albumin, total protein, sodium, potassium, blood urea nitrogen, total cholesterol, low-density lipoprotein, very low- density lipoprotein, high-density lipoprotein, and triglycerides were measured during the biochemical analysis. NLR was calculated by dividing the neutrophils count by the lymphocyte count. HbA1c level was measured using Agilent HPLC methods.
Statistical analysis
For the statistical analysis of the data, the package program SPSS 18.0 (Statistical Package for Social Sciences - SPSS, Inc. Chicago, Illinois, USA) was used. Categorical variables were expressed as a percentage. Numerical variables are shown as mean±standard deviation (SD). The one-sample Kolmogorov-Smirnov test was used to evaluate whether the variables showed a normal distribution. The existence of a linear relationship between parameters with a normal distribution was assessed using Pearson’s correlation test, while the existence of a linear relationship between parameters without a normal distribution was evaluated using Spearman’s correlation test. Student t-test was used for the normal distribution of the parameters for evaluating the differences between the groups, Mann-Whitney U test was used for parameters without a normal distribution. Statistical significance was based on a value of p< 0.05. The study was approved by the institutional ethics committee and conducted in accordance with the Declaration of Helsinki. All patients and control groups provided written informed consent before study.
Result
Table 1:Demographic data.
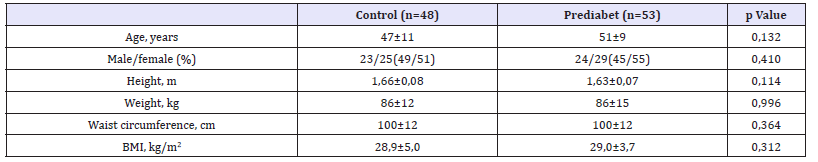
BMI: Body mass index.
Table 2:Echocadiographic measurements.

LVEDD: Left Ventricular End Diastolic Diameter; EF: Ejection Fraction; IVS: Inter Ventricular Septum; PW: Posterior Wall; PASB: Pulmonary Artery Systolic Pressure
In this study, forty-eight consecutive normal individuals (control group) and 53 consecutive prediabetic patients (prediabetic group) were matched and analyzed. Both groups were statistically similar in age, height, body weight, BMI and waist circumference (Table 1). The number of patients with an increased waist circumference was higher in the prediabetic group (n=27) than the control group (n=24) but this difference was not statistically significant. The number of obese patients in the prediabetic group (n=20) was like that in the control group (n=18). There was an anticipated positive correlation between BMI and waist circumference (r=0.723; p< 0.001). The number of patients with hypertension in the prediabetes group (n=12) was higher than the control group (n=10) but not statistically significant. LVEF, LVEDD, wall thickness, aortic diameter, left atrium size and pulmonary artery systolic pressure were statistically similar in both groups (Table 2). The mean NLR value of the prediabetic group was significantly higher than that of the control group (2,67±1,76 vs. 1,70±0,9 p< 0.001). The laboratory values in each group are shown in Table 3. As expected in the prediabetes group, the value of fasting blood glucose and HbA1C was statistically significantly higher than the control group. The CRP level in the prediabetic group was significantly higher than that in the control group. It was statistically significant (p< 0,001). Among all patients, age was no correlated with the NLR (r=0.012). In a correlation analysis including all patients, HbA1c levels was positively correlated with NLR (r=0.426, p< 0.001) values.
Table 3:Laboratory values.
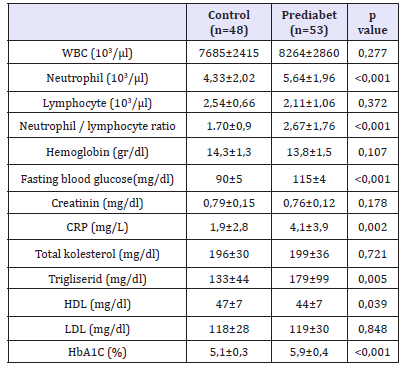
WBC: White Blood Cells; CRP: C-Reactive Protein; HDL: High Density Lipoprotein; LDL: Low Density Lipoprotein
Discussion
In this study, NLR was found to be high in patients with prediabetes newly diagnosed. Previous studies in the literature have been associated with diabetes mellitus (DM) [9,10]. Prediabetes is defined as prediabetes when the plasma glucose level is normally high but does not reach the diagnostic limits of diabetes. Prediabetes is associated with increased cardiovascular risk and mortality [11,12]. It is stated that the rate of developing diabetes in prediabetic patients is 70% in some publications. Therefore, prevention of diabetic development and diabetic clinical complications with early diagnosis increases the clinical significance of the disease [13]. Lou et al. [10] compared 310 patients with insulin resistance and 130 healthy groups. As a result of the study, it was determined that the insulin resistance increased by an odds ratio of 7,231 for each unit increase in NLR. In our study, we found statistically higher NLR in patients with prediabetes than healthy controls. Logistic regression analysis showed that the risk predictors of prediabetes include NLR, HbA1c.
Akbaş et al. [14] and Huang et al. [15] have been suggested that high levels of NLR in patients are a safe predictor of early stage diabetic nephropathy. In 1377 individuals, NLR was found to be high in diabetic patients by Verdoia et al. [16]. It has also been found that high NLR in diabetic cases is associated with prevalence and severity of coronary artery disease [16]. Yilmaz et al. [17] that NLR values were higher in obese individuals, in which the body mass index was found to be significantly higher in patients with high NLR.
Conclusion
An important finding of this study was that the NLR value was a predictor of diabetes mellitus is significantly higher in prediabetic patients. If this finding is confirmed by studies with larger series and different patient groups, NLR values can be used as a simpler and more cost-effective alternative to prediabetes diagnosis
References
- Coutinho M, Gerstein HC, Wang Y, Yusuf S (1999) The relationship between glucose and incident cardiovascular events: A meta regression analysis of published data from 20 studies of 95,783 individuals followed for 12.4 years. Diabetes Care 22(2): 233-240.
- Levitan EB, Song Y, Ford ES, Liu S (2004) Is nondiabetic hyperglycemia a risk factor for cardiovascular disease? A meta-analysis of prospective studies. Arch Intern Med 164(19): 2147-2155.
- Danaei G, Lawes CM, Vander HS, Murray CJ, Ezzati M (2006) Global and regional mortality from ischaemic heart disease and stroke attributable to higher-than-optimum blood glucose concentration: comparative risk assessment. Lancet 368(9548): 1651-1659.
- Michael M, Engelgau KM, Venkat N, William HH (2000) Screening for type 2 diabetes. Diabetes Care 23(10): 1563-1580.
- Nichols GA, Hillier TA, Brown JB (2007) Progression from newly acquired impaired fasting glusose to type 2 diabetes. Diabetes Care 30(2): 228-233.
- Shen XH, Chen Q, Shi Y, Li HW (2010) Association of neutrophil/ lymphocyte ratio with long-term mortality after ST elevation myocardial infarction treated with primary percutaneous coronary intervention. Chin Med J 123(23): 3438-3443.
- Kaya H, Ertas F, Islamoglu Y, Kaya Z, Atilgan ZA (2013) Association between neutrophil to lymphocyte ratio and severity of coronary artery disease. Clin Appl Thromb Hemost 20(1): 50-54.
- Shetty P, Kumanyika S, Ko GT (2008) Waist circumference and waist-hip ratio: report of a WHO expert consultation, Geneva, pp. 1-47.
- Sefil F, Ulutas KT, Dokuyucu R, Sumbul AT, Yengil E, et al. (2014) Investigation of neutrophil lymphocyte ratio and blood glucose regulation in patients with type 2 diabetes mellitus. J Int Med Res 42(2): 581-588.
- Lou M, Luo P, Tang R, Peng Y, Yu S, et al. (2015) Relationship between neutrophil-lymphocyte ratio and insulin resistance in newly diagnosed type 2 diabetes mellitus patients. BMC Endocr Disord 15: 4-9.
- Seshasai SR, Kaptoge S, Thompson A, Gao P, Sarwar N, et al. (2011) Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 364(9): 829-841.
- Balkau B (2000) The DECODE study. Diabetes epidemiology: collaborative analysis of diagnostic criteria in Europe. Diabetes Metab 26(4): 282-286.
- (2004) American diabetes association screening for type 2 diabetes. Diabetes Care 27(Suppl 1): 11-14.
- Akbas EM, Timuroglu A, Ozcicek A, Ozcicek F, Demirtas L, et al. (2014) Association of uric acid, Atherogenic index of plasma and albuminuria in diabetes mellitus. Int J Clin Exp Med 7(12): 5737-5743.
- Huang W, Huang J, Liu Q, Lin F, He Z, et al. (2015) Neutrophil-lymphocyte ratio is a reliable predictive marker for early-stage diabetic nephropathy. Clin Endocrinol (Oxf) 82(2): 229-233.
- Verdoia M, Schaffer A, Barbieri L, Aimaretti G, Marino P, et al. (2015) Impact of diabetes on neutrophil-tolymphocyte ratio and its relationship to coronary artery disease. Diabetes Metab 41(4): 304-311.
- Yilmaz H, Ucan B, Sayki M, Unsal I, Sahin M, et al. (2015) Usefulness of the neutrophil-to-lymphocyte ratio to prediction of type 2 diabetes mellitus in morbid obesity. Diabetes Metab Syndr 9(4): 299-304.
© 2018 Mehmet Celik. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






