- Submissions

Full Text
Global Journal of Endocrinological Metabolism
The Effect of Bedtime or Morning Intake of Levothyroxine in Patients with Hypothyroidism
Mahmut Apaydin*, Selvihan Beysel, Muhammed Kizilgul, Seyfullah Kan, Bekir Ucan, Mustafa Caliskan, Ozgur Ozcelik, Taner Demirci, Mustafa Ozbek and Erman Cakal
Department of Endocrinology and Metabolism, Diskapi Yildirim Beyazit Teaching and Research Hospital, Ankara, Turkey
*Corresponding author: Mahmut Apaydin, Irfan Bastug Cad. 06110, Altindag / Ankara, Turkey
Submission: January 16, 2018; Published: January 25, 2018

ISSN: 2637-8019Volume1 Issue3
Abstract
Background: Patients with hypothyroidism are generally recommended to take their levothyroxine(LT4) half an hour or one hour before breakfast because LT4 absorption increases with fasting. However, data related to whether bedtime or morning intake of levothyroxine has a better influence thyroid-stimulating hormone (TSH) equilibrium limited. This aim of this study was to compare the effect of switching the intake time of LT4 from morning to bedtime clinical, hormonal, and biochemical parameters.
Material and Methods: A total of 60 patients (55 females, 5 males) with a mean age of 45.5±13.3 years (range, 21-74years) were enrolled in the study. The route of LT4 administration in patients with routine dosing schedules for LT4 treatment of 60minutes before breakfast was switched to bedtime (at least three hours after the evening meal), and patients were followed up for 12 weeks.
Results: A slight but insignificant increase in TSH levels (2.8±1.3 to 3.6±3.8IU/L, p>0.05) was observed. The serum-free T4 levels in patients taking LT4 at bedtime were significantly higher than in patients taking LT4 at breakfast (1.2±0.1 vs.1.1±0.1ng/dL, p<0.05). Body weight (73.5±15.7 to 74.5±16.2kg, p<0.05) and body mass index (28.8±5.7 to 29.1±6.0kg/m2, p<0.05) were significantly increased during follow-up. Ten(16.7%) patients reported newly developed night sweats and 8 (13.3%) had increased appetite at the end of the study.
Conclusions: Physicians may recommend bedtime LT4 regimens to patients with hypothyroidism who have poor adherence to regular morning medical treatment. However, the possibility of an increase in some symptoms should be kept in mind.
Keywords: Levothyroxine; Hypothyroidism; Timing of intake
Introduction
Levothyroxine (LT4) is one the most commonly prescribed medications worldwide because the prevalence of primary hypothyroidism is high among the general population [1]. Optimal intestinal absorption of LT4 under fasting conditions reduced from approximately 80% to 40-64% with concurrent food ingestion [2]. The biochemical response to LT4 treatment is evaluated through the serum thyroid-stimulating hormone (TSH) concentration in patients with hypothyroidism [3]. The adherence to LT4 treatment and pharmacologic conditions related to malabsorption are the two major determinants of the biochemical response [4].
The guidelines recommend LT4 administration either 60minutes before breakfast or at bedtime, three hours after the evening meal [2]. As a stringent recommendation, taking LT4 on an empty stomach may interfere with the patient treatment adherence. However, data related to whether bedtime or morning intake of levothyroxine has a better influence on the TSH equilibrium limited. A study showed that serum TSH concentrations were unchanged when the LT4 intake time was switched from 1-2h after breakfast to midnight in older patients [5]. A pilot study of 12 patients showed that the participants had lower serum TSH concentrations and higher thyroid hormone concentrations when their LT4 intake was switched from bedtime to 30minutes before breakfast [6]. A randomized double-blind crossover trial demonstrated a decrease in TSH levels and an increase in free T4 (FT4) and total T3 levels when levothyroxine was taken at bedtime [7]. Bach-Huyn et al. [8] reported that patients had significantly higher concentrations when taking their LT4 at bedtime when compared with levothyroxine administered in the fasting state. In a study of 152 drug-naive patients with primary hypothyroidism, no significant difference in thyroid function tests was seen in the morning and evening dose groups after 6 and 12 weeks of treatment [9]. The aim of our study was to evaluate the effect of switching the intake time of LT4 from early morning to bedtime on clinical, hormonal, and biochemical parameters.
Material and Methods
Patients aged 18-75years with hypothyroidism who were under LT4 treatment were enrolled in the study. Patients were eligible for the study if their serum TSH was within the laboratory reference range (0.5-5mIU/L). Patients with celiac disease, autoimmune gastritis, inadequate gastric acid secretion, pregnancy, and significant renal or cardiac disease were excluded. Patients taking bile acid sequestrants, antacids, cholestyramine, colestipol, and those taking medications that might potentially affect serum TSH concentrations, such as steroids, T3 preparations, dopamine analogs, somatostatin analogs, phenytoin, and carbamazepine were also excluded. Patients were required to have been on the same dose of LT4 consistently for the last 6months in order to qualify for enrollment in the study. A total of 65 adult patients with hypothyroidism due to Hashimoto's thyroiditis, prior radioiodine treatment for Graves' disease, or thyroidectomy due to a nodular goiter receiving LT4 regularly met the inclusion criteria. Five patients were withdrawn from the study, three due to palpitations and two because of non-adherence to treatment. LT4 intake 1hour before breakfast (fasting breakfast regime) was switched to bedtime (at least three hours after evening meal) in patients with hypothyroidism. The patients were monitored for 12weeks. Telephone follow-ups were conducted every 4weeks in which the patients were reminded to adhere to the timing and dietary directions. Blood for thyroid function tests was drawn at the study initiation and at the end of the 12-week period. The Medical Ethics Committee of Ankara Outdoors Training and Research Hospital approved the study protocol and written informed consent was obtained from each patient.
Statistical Analysis
Statistical analysis was performed using SPSS 18.0 (SPSS, Inc) software. Descriptive analyses are expressed as the median±standard deviation (SD) or percentages (%).Normality was tested using the Kolmogorov-Smirnov and Shapiro-Wilk W test. The effects of switching treatment regimen on all variables were measured by performing an independent-sample t-test. Statistical significance was considered as p<0.05.
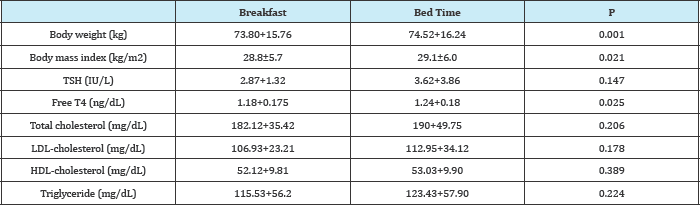
Table 1: The clinical and laboratory results after 12 weeks of bedtime and morning levothyroxine treatments.
Results
The clinical characteristics of the study subjects are summarized in Table 1. A total of 60 patients (55 females, 5 males) with a mean age of45.5±13.3years (range, 21-74years) were analyzed after 12weeks of switching LT4 from early morning to bedtime. A slight but insignificant increase in TSH levels (2.8±1.3 to 3.6±3.8IU/L, p>0.05) was observed. The serum-free T4 levels in patients taking LT4 at bedtime were significantly higher than in patients taking LT4 before breakfast (1.2±0.1 vs.1.1±0.1ng/dL, p<0.05). Body weight (73.5±15.7 to 74.5±16.2kg, p<0.05) and body mass index (BMI) (28.8±5.7 to 29.1±6.0kg/m2, p<0.05) were significantly increased during follow-up.Total cholesterol, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglyceride, and cortisol levels were not changed during follow-up (p>0.05). Serum TSH, FT4, BMI, body weight, and lipid levels were similar between bedtime and morning LT4 treatment regimens in patients aged over 60years (p>0.05). Ten (16.7%) patients reported newly developed night sweats and 8 (13.3%) patients had increased appetite at the end of the study.
Discussion
Our results showed a significant increase in BMI, body weight, and FT4 levels after switching LT4 intake from prebreakfast to bedtime in patients with hypothyroidism. However, the two regimens did not result in a significant difference in terms of serum TSH levels. Additionally, serum TSH, FT4, BMI, body weight, and lipid levels were similar between the bedtime and morning LT4 treatment regimens in patients aged more than 60years.
Fasting intake of LT4 is recommended because the presence of food inhibits the gastrointestinal absorption of LT4. Many patients consume coffee during the morning hours and take concomitant medications may impair LT4 absorption; therefore, in addition to the general recommendation of taking LT4 1h before breakfast, it is also recommended that LT4 should not be taken within 4hours of taking other medicines that may impair its absorption and complicate the dosing schedule [5,6,8,10]. In general clinical practice, LT4 taken before breakfast, i.e. during the fasting state, is recommended to avoid the adverse effects of food or medications on LT4 absorption [7]. In this regard, bedtime LT4 intake may be more practical for many patients [6]. When our patients switched from pre-breakfast LT4 intake to bedtime LT4, a significant increase in FT4 without a change in TSH levels was observed. This increase in FT4 may be explained on the basis of several factors. First, even if taken 1hour before breakfast, the food ingested during breakfast can impair LT4 intestinal absorption. Increased LT4 uptake due to slowing intestinal motility during the night, which may lead to longer exposure of LT4 to the intestinal wall might be another explanation [6]. Bolk et al. [7] compared pre-breakfast and bedtime LT4 intake, and decreased TSH and increased FT4 and FT3 were observed with bedtime LT4 intake. Lipid profile and quality of life were similar between the two treatment regimens in that study. In the present study, no effects on lipid profile were observed.
An increase in FT4 levels in bedtime regimens may be associated with patients' treatment adherence. For instance, coffee intake in the morning may impair absorption [8]. A previous study reported no changes in serum TSH levels when older patients switched from LT4 intake lhour after breakfast to nighttime regimen. However, in that study, LT4 was given after a snack in the night hours or 1hour after breakfast, i.e. both intakes occurred in the postprandial state [5]. In our study, no differences in serum TSH, FT4, and body weight were found between the two regimens among those over 60years of age. In another study, an increase in FT3 and FT4 and a decrease in TSH was observed with bedtime LT4 intake. In previous studies involving non-fasting administration following breakfast, an increase in serum TSH was observed with a more variable TSH as compared with fasting regimes [5,8]. In our study, no significant changes in serum TSH levels occurred when patients switched from fasting breakfast intake to the bedtime regimen, suggesting that variability in TSH might be closely related with patients' adherence to therapy in real-life conditions. The increase in fT4 levels in our study might be related to increased LT4 absorption due to the maximal levels of basal gastric acid secretion that occurs in late night hours [5,6,8]. In contrast with previous studies [7], an increase in BMI and body weight was found following 3months of bedtime LT4 intake, which might be due to increased appetite. Weight gain or inability to lose weight has been reported in patients receiving treatment for either hypo- or hyperthyroidism [5,6,8]. Also, the new-onset appetite increase and night sweats in our patients might be associated with high serum FT4 levels. Bach- Huynh et al. compared the effect of LT4 intake with breakfast or at bedtime on the biochemical response and an increase in serum TSH and no change in FT4 or TT3 was observed [8]. Elliott [5] found no change in serum TSH when patients switched from pre-breakfast LT4 to bedtime LT4, which is similar to our findings. Non-fasting LT4 regimens were reported to cause more variability in TSH levels, whereas fasting LT4 intake was able to achieve the target TSH range and prevent iatrogenic subclinical thyroid disease [5,6,8]. According to a recent review article, bedtime intake of LT4 could be a choice for patients who prefer not to take their medication with food [10].
To our knowledge, our study is the first from Turkey to evaluate the effect of timing on different LT4 regimens'on the biochemical response and clinical parameters. Our study has to be viewed within the context of some potential limitations, however. The effect of eating habits in a certain geographic location within a certain cultural context cannot be excluded because the present study was a single-center study. Also, our study had a short duration of follow- up and a small sample size.
Conclusion
In conclusion, an increase in FT4 with no change in TSH was observed when the fasting pre-breakfast regimen was switched to a fasting bedtime regimen of LT4 intake. Based on our results, physicians might recommend a bedtime LT4 regimen to patients with hypothyroidism who are more likely to exhibit poor adherence to morning regimens, but who also desire a convenient regimen.
References
- Tunbridge WM, Evered DC, Hall R, Appleton D, Brewis M, et al. (1977) The spectrum of thyroid disease in a community: the Whickham survey. Clin Endocrinol (Oxf) 7(6): 481-493.
- Jonklaas J, Bianco AC, Bauer AJ, Burman KD, Cappola AR, et al. (2014) Guidelines for the treatment of hypothyroidism: prepared by the american thyroid association task force on thyroid hormone replacement. Thyroid 24(12): 1670-1751.
- Carr D, McLeod DT, Parry G, Thornes HM (1988) Fine adjustment of thyroxine replacement dosage: comparison of the thyrotrophin releasing hormone test using a sensitive thyrotrophin assay with measurement of free thyroid hormones and clinical assessment. Clin Endocrinol (Oxf) 28(3): 325-333.
- Centanni M (2013) Thyroxine treatment: absorption, malabsorption, and novel therapeutic approaches. Endocrine 43(1): 8-9.
- Elliott DP (2001) Effect of levothyroxine administration time on serum TSH in elderly patients. Ann Pharmac other 35(5): 529-532.
- Bolk N, Visser TJ, Kalsbeek A, van Domburg RT, Berghout A (2007) Effects of evening v/s morning thyroxine ingestion on serum thyroid hormone profiles in hypothyroid patients. Clin Endocrinol (Oxf) 66(1): 43-48.
- Bolk N, Visser TJ, Nijman J, Jongste IJ, Tijssen JG, et al. (2010) Effects of evening v/s morning levothyroxine intake: a randomized double-blind crossover trial. Arch Intern Med 170(22): 1996-2003.
- Bach-Huynh TG, Nayak B, Loh J, Soldin S, Jonklaas J (2009) Timing of levothyroxine administration affects serum thyrotropin concentration. J Clin Endocrinol Metab 94(10): 3905-3912.
- Rajput R, Chatterjee S, Rajput M (2011) Can Levothyroxine Be Taken as Evening Dose? Comparative Evaluation of Morning versus Evening Dose of Levothyroxine in Treatment of Hypothyroidism. J Thyroid Res 2011: 505239.
- Geer M, Potter DM, Ulrich H (2015) Alternative schedules of levothyroxine administration. Am J Health Syst Pharm 72(5): 373-377.
© 2018 Mahmut Apaydin, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






