- Submissions
Full Text
Global Journal of Endocrinological Metabolism
Periodontal Disease and Dental Treatment in Diabetic Patients
Dr. Llambés F*
Medically Compromised Patients Department, University of Valencia, Spain
*Corresponding author: Dr. Llambes F, Medically Compromised Patients Department, School of Dentistry, University of Valencia, Spain
Submission: October 02, 2017; Published: November 13, 2017

ISSN: 2637-8019Volume1 Issue3
Short Communication
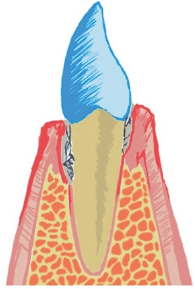
Periodontal disease is a destruction of the tissues that support the teeth initiated by dental plaque. Bacteria present in the mouth attach to the tooth surface and penetrate below the gum line destroying the periodontal ligament. In Figure 1 we can see calculus below the gum (mineralized plaque) which has active plaque on top, which is responsible of the damage. However tissue destruction around the tooth is produced by the immune response to plaque and not by the plaque itself. That's why periodontal disease does not affect all subjects with the same severity.
Figure 1: Periodontal disease with calculus below the gingival.
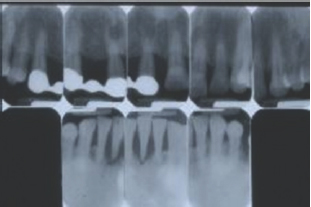
Diabetic patients have shown more severe periodontal disease than healthy control groups, especially when poor glycemic control is present Figure 2 shows a diabetic individual with severe periodontal disease, teeth are longer with increased mobility and migrations, roots are exposed and inflammatory signs can be observed in the gingival (edema, redness and bleeding). We also can see extreme bone destruction around teeth in X-rays from Figure 3 (bone should be 1,5mm below the enamel of the crown). One hypothesis to explain this damage in the periodontal tissues states that advanced glycosylation end products that appear in diabetic patients due to the hyperglycemia make the immune system hyperreactive to dental plaque, increasing destruction of periodontal support [1-3].
Figure 2: Patient 1: Severe periodont it is in a diabetic patient.

Figure 3: Patient 1: Periodontal destruction showed by periapical X-ray.
It also has been correlated periodontal disease severity with some systemic inflammatory markers such as C- reactive protein in diabetic patients . This is an interesting finding because it could show that some subjects have a more reactive immune system to oral plaque and diabetes inflammatory products, leading to more periodontal destruction in the mouth and more diabetic complications in the body.
Even though diabetic individuals have more severe periodontal disease, a successful periodontal treatment can be performed. Elimination of plaque and calculus attached to the tooth, appropriate oral hygiene and periodontal control every 6 to 12 months are the keys for success. Treatment results can be improved if we associate an antibiotic such as doxycycline (100mg per day for 15 days) at the same time we remove the dental calculus, but we have to keep in mind that more recurrence of periodontal disease will be observed in diabetic patients that have poor glycemic control. More information about the relationship between diabetes and periodontal disease can be found in [4].
Some cases of period on it is in diabetics are diagnosed very late. At this time, teeth have lost most of their support and must be extracted. Fortunately we can use nowadays predictable techniques to regenerate bone for placing dental implant to achieve a new dentition (Figure 4-6) [5,6].
Figure 4: Patient 2: Computerized tomography of a diabetic subject that will lose all the teeth due to periodontal disease. The reduced bone in the upper posterior areas can be observed.
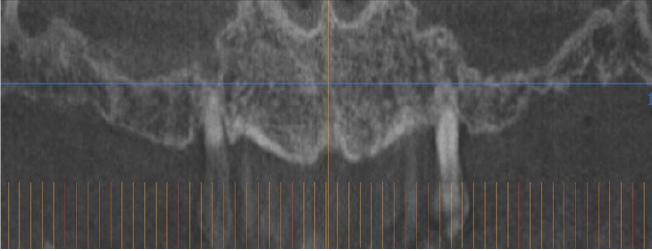
Figure 5: Patient 2: Bone regeneration achieved inside the maxillary sinus (new bone has a different radiopaque image than the original bone).
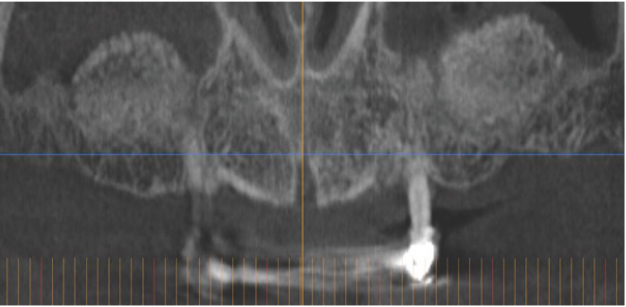
Figure 6: Patient 2: Panoramic X ray with implants supporting a fix upper and lower prosthesis.

References
- Papapanou PN (1996) Periodontal diseases: epidemiology. Ann Periodontol 1(1): 1-36.
- Lalla E, Lamster IB, Drury S, Fu C, Schmidt AM, et al. (2000) Hyperglycemia, glycoxidation and receptor for advanced glycation endproducts: potential mechanisms underlying diabetic complications, including diabetes-associated periodontitis. Periodontol 23: 50-62.
- Llambés F, Silvestre FJ, Hernández Mijares A, Guiha R, Bautista D, et al. (2012) Efect of periodontal disease and non surgical periodontal treatment on C-reactive protein. Evaluation of type 1 diabetic patients. Med Oral Patol Oral Cir Bucal 17(4): e562-e568.
- Llambés F, Silvestre FJ, Hernández Mijares A, Guiha R, CaffesseR (2005) Effect of non-surgical periodontal treatment with or without doxycycline on the periodontium of type 1 diabetic patients. J ClinPeriodontol 32(8): 915-920.
- Llambés F, Arias-Herrera S, Caffesse R (2015) Relationship between diabetes and periodontal infection. World J Diabetes 6(7): 927-935.
- Llambés F, Silvestre FJ, Caffesse R (2007) Vertical guided bone regeneration with bioabsorbable barriers. J Periodontol 78(10): 20362042.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






