- Submissions

Full Text
Gerontology & Geriatrics Studies
Chorea Hyperglycaemia Basal Ganglia Syndrome, a Neurological Complication of Diabetes: A Case Report
Moussavou Cédrick*, El Bakal Ayoub, Hamid Mohamed, Yassine El Adraoui, Slimani Sarah, Ibrahim Touré, Belghacham Hajar and Bourazza Ahmed
Mohammed V Military Teaching Hospital, Mohammed V University, Morocco
*Corresponding author:Moussavou Cédrick, Mohammed V military teaching hospital and Mohammed V University, Rabat, Morocco
Submission: June 17, 2022; Published: December 02, 2022

ISSN 2578-0093Volume8 Issue1
Abstract
Abnormal involuntary movements induced by hyperglycaemia are epic manifestations of diabetes. They are observed particularly in cases of poorly controlled diabetes. Chorea Hyperglycaemia Basal Ganglia syndrome (C-H-BG) recently referred to as Diabetic Striatopathy (DS) is a rare entity that can lead to misdiagnosis [1]. The prevalence of C-H-BG or DS has been reported to be 1 in 100,000 [2]. Although rare, C-H-BG is often described in non-ketotic hyperglycemia and hypoglycemia [3]. Only rarely has it also been described in ketotic hyperglycaemia. We report a case of diabetic chorea following diabetic ketoacidosis.
Keywords: Hypoglycaemia; Hyper density; Sitagliptin; Clonazepam; Metformin; Creatinine
Abbreviations:DS: Diabetic Striatopathy; C-H-BG: Chorea Hyperglycaemia Basal Ganglia Syndrome; BGS: Basal Ganglia Syndrome
Case Report
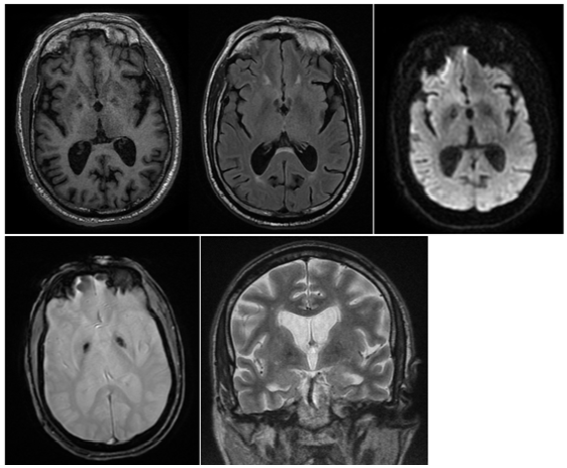
A 60-year-old man with chronic weaned smoking was being treated for hypertension. He had been followed for 20 years for type 2 diabetes, complicated by macroangiopathy (lower limb peripheral artery) and microangiopathy (diabetic retinopathy, diabetic nephropathy, and diabetic neuropathy). He was treated with Insulin (Lantus), Sitagliptin and Metformin. He was admitted to hospital with apyretic delirium. On physical examination, he was apyretic and confused. His blood pressure was 137/84mm Hg, his heart rate was 72 beats per minute. We noticed abrupt involuntary movements large and non-rhythmic, that started in the right upper limb, then there was a progressive extension to the right lower limb, afterwards to the left upper limb, neck, and face. These movements occurred on a background of hypotonia. This reflected a generalized chorea-ballism. Video V1 showing choreic and ballism movements that were observed during the hospitalization. The rest of the physical examination was normal. Laboratory tests revealed: hyperglycaemia of 5.64g/L; with high glycated haemoglobin levels (HbA1c) of 10.9%; serum osmolarity was 313.62mOsm; Her venous pH was pH=7.32; PCO2=42mmHg; urea=1g/L; creatinine=23mg/L; bicarbonate at 21mEq/L; sodium at 133mmol/L; potassium 4.90mmol/L; Chloride=100mmol/L; CRP at 17.20mg/L; procalcitonin at 0.36ng/ml. The blood count was normal (WBC=7.70×103/μL; haemoglobin 11.70g/dL). He had no hepatic dysfunction or electrolyte or thyroid disorders. Urine ketones were positive at 3+. He was diagnosed with diabetic ketoacidosis. Brain CT showed bilateral pallidal hyper density (Figure 1), characteristic of C-H-BG syndrome. And on brain MRI on day 8 of the course, bilateral pallidal hypointense signal was observed (Figure 1). The patient was treated simultaneously with insulin titration, hydration, and a course of haloperidol 2mg/ml 3 drops/08 hours. Five days later, glycaemic control was favourable, with complete resolution of the chorea-ballism (video V2). Video 1: Choreic and ballism movements. Video 2: Complete resolution of the chorea-ballism (Figure 2).
Figure 1:Axial brain CT scan: Hyper density in bilateral pallidum.
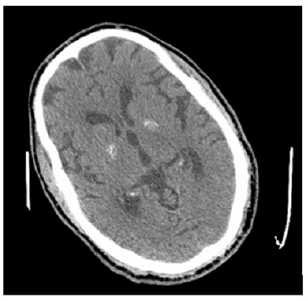
Figure 2:MRI brain demonstrated abnormal hypointense signal in the bilateral pallidum on T1, FLAIR, DWI, T2*, and T2-weighted.
Discussion
Diabetic chorea, also known as Chorea Hyperglycaemia Basal Ganglia Syndrome (C-H-BG) is mostly (81.7% of patients) associated with non-ketotic hyperglycaemia [4]. However, in our patient, the C-H-BG was ketotic. This supports the hypothesis of Chua et al which suggests that the occurrence of C-H-BG is not limited to non-ketotic patients [4]. Bilateral involvement was noted in 9.7% of patients in Chua [4] and 11.4% of patients in Oh et al. [5] respectively. Similarly, in Dubey’s study, chorea-ballism associated with ketotic hyperglycaemia was bilateral in 19.5% of cases [6]. The upper and lower limbs were predominantly affected, while a small proportion also had facial involvement [4]. Dubey et al, reported 83.1% of patients had stigmata of diabetic microangiopathy (retinopathy, neuropathy, and nephropathy) with a glycated haemoglobin (HbA1c) of 10.4±1.6, suggesting longterm uncontrolled diabetes. [6]. Our observation corroborates this hypothesis. The radiograph of C-H-BG patients is a basal ganglia lesion characterized by hyper density (on brain CT) or hypersignal on T1-weighted brain MRI. Bilateral basal ganglia lesions are present in patients with generalized chorea [4,5]. In most cases, the radiological lesions reported are unilateral. Chua et al. [4] reported bilateral involvement in 9.7% of patients with a predominance of left involvement according to the left/right involvement ratio of 1.2:1 [4], contrary to what was observed in our patient where we note a right predominance. In our patient, the basal ganglia hyper densities as well as the choreic movements were bilateral. Dwarak et al. [7] reported bilateral basal ganglia hypersignals [7]. The precise pathophysiological mechanism of chorea-ballism’s secondary to hyperglycaemia is unknown. It has been established that control of hyperglycaemia is the mainstay of treatment of CHBG, allowing to relieve, or even correct, the motor symptoms [8]. Thus, the treatment of chorea in CHBG syndrome is based on the normalization of glycemia [5,9]. In some cases, various combination therapies may be used: Glycaemic control and drugs, including haloperidol, tetrabenazine, risperidone, tiapride, chlorpromazine, diazepam, and clonazepam [10,4]. Oh et al. [5], reported that 74% of C-H-BG patients had complete resolution of chorea after a period ranging from one day to 10 months, with a median of six months. This is corroborated by the complete resolution within 5 days in our patient [5].
Conclusion
The singularity of our case is that it is one of the rare, described cases of chorea, hyperglycaemia, Basal Ganglia Syndrome (BGS) in association with ketoacidosis. The chorea is associated with a bilateral pallidal radiographic abnormality (CT and MRI). If diagnosed and treated early, chorea induced by ketoacidosis has a good prognosis.
Ethics
For the video recordings, the patient’s consent was taken.
References
- Lietz TE, Huff JS (1995) Hemiballismus as a presenting sign of hyperglycemia. Am J Emerg Med 13(6): 647-648.
- Ondo WG (2011) Hyperglycemic nonketotic states and other metabolic imbalances. Handb Clin Neurol 100: 287-291.
- Piccolo I, Sterzi R, Thiella G (1998 ) Chorea in hyperglycemia. Diabetes Care 21(10): 1777.
- Chua CB, Sun CK, Hsu CW, Tai YC, Liang CY, et al. (2020) Diabetic striatopathy: clinical presentations, controversy, pathogenesis, treatments, and outcomes. Sci Rep 10(1): 1594.
- Oh SH, Lee KY, Im JH, Lee MS (2002) Chorea associated with non-ketotic hyperglycemia and hyperintensity basal ganglia lesion on T1-weighted brain MRI study: a meta-analysis of 53 cases including four present cases. J Neurol Sci 200(1-2): 57-62.
- Dubey S, Chatterjee S, Ghosh R, Louis ED, Das S, et al. (2022) Acute onset movement disorders in diabetes mellitus: A clinical series of 59 patients. Eur J Neurol 29(8): 2241-2248.
- Dwarak S, Prabhakar K, Kakanale M, Aswathanarayana A, Sindhu BR (2019) Chorea, hyperglycemia, basal ganglia syndrome in diabetes-two rare case reports. Maedica (Bucur) 14(1): 59-62.
- Das L, Pal R, Dutta P, Bhansali A (2017) Diabetic striatopathy and ketoacidosis: report of two cases and review of literature. Diabetes Res Clin Pract 128: 1-5.
- Lai PH, Tien RD, Chang MH, Teng MM, Yang CF, et al. (1996) Chorea-ballismus with nonketotic hyperglycemia in primary diabetes mellitus. AJNR Am J Neuroradiol 17(6): 1057-1064.
- McCullen MK, Miller J, Jabbour S, Furlong K, Shirodakar M, et al. (2010) Expert opinion: Chorea in the setting of hyperglycemia: a case report and review of literature. Practical Neurology.
© 2022 Moussavou Cédrick. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






