- Submissions

Full Text
Gerontology & Geriatrics Studies
Manic and Depressive Expressions of Bipolar Disorders and Treatment
James Paul Pandarakalam*
Consultant Psychiatrist, UK
*Corresponding author:James Paul Pandarakalam, Consultant Psychiatrist, UK
Submission: February 01, 2022; Published: February 16, 2022

ISSN 2578-0093Volume7 Issue4
Summary
The artistic creativity and risk-taking behaviour of hypomania explains the evolutionary value of Bipolar Disorder (BD) and its survival over the evolutionary pressures, but BD is a destructive psychiatric condition with many challenges. Bipolar affective disorders are associated with significant mortality and morbidity. Diagnosis of BD is generally put on hold until the patients declare mania, but such a delay can be mitigated if clinicians develop the expertise to detect disguised bipolarity. Unlike schizophrenia research, BD research has been taking a very slow pace. BD has a multifactorial aetiology that includes genetic, biological, and psychological factors. Investigators hope to find new remedies that would enable sufferers to live a functional life like that of patients with Diabetes Mellitus and to achieve a benign course of the illness. BD in the elderly population carries its own risks and warrants special management. The easy availability of medical knowledge through cybernetic system prompts patients and families to challenge the clinicians to keep up to date and make clear-cut diagnosis.
Keywords: Depression; Hypomania; Mania; Mixed affective states; Rapid cycling; Mood stabilizers; Antipsychotics
Introduction
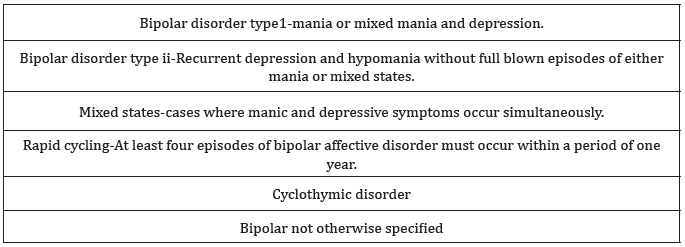
Bipolar disorders are characterized by a diverse pattern of symptoms, ranging from mild depression or hypomania (low highs) to severe or rapidly cycling forms of mania and depression with concurrent psychotic symptoms (Table 1). The incidence of bipolar 1 disorder is approximately 1 percent of the world population [1]. BD type1 is equated to the old terminology of manic-depressive psychosis. BD type ii is much more prevalent and a spectrum of BD that includes states of chronic mild hypomania has also been described [2]. When proper treatment plans are devised for specific people demonstrating the condition, the illness can be managed, and a benign course achieved. A few sufferers have demonstrated artistic creativity in the early phase of hypomania. Conversely, full-blown mania and depression are characterized by destructive tendencies-to put this idiomatically, though the “big bang” often associated with bipolar disorder is questionable, untreated cases of bipolar disorder may be said to embody a “big crunch”. It is estimated that there are 297000 people in UK suffering from this disorder and the annual cost attributable to BD is £2 billion at 1999/2000 prices.
Table 1: Bipolar disorders.
Etiological Search
BD has a multifactorial etiology. A strong genetic loading is identified for BD by family and twin studies. A prevalence rate of 15-20 percent has been demonstrated in first-degree relatives of patients with bipolar affective disorders. Twin studies have led to a concordance rate in monozygotic twins of 79 percent and in dizygotic twins of 19 percent. DNA markers have been identified through linkage studies and have been replicated in more than one study, particularly on chromosomes 18 and 22 [3]. BD has a heritability of 60-80% [4], but its etiology is highly polygenic [5,6]. The gene Ankyrin-3 (ANK3) has been consistently associated with BD in several genome-wide association studies [7]. Clear neurological changes are not well recognized in BD. An isolated case report of a patient who suffers from Paraneoplastic cerebellar degeneration secondary to which the patient, a young woman, developed BD has been reported [8].
In the 1960s the identification of the therapeutic value of lithium in the treatment of BD favored a strict biological view of this disorder, even though psychological factors may be the precipitant for this illness. Subsequently the positive therapeutic effects of anticonvulsant supported the hypothesis that brain processes apparently similar to kindling phenomena [9] occur in BD and such a view could accommodate the psychological precipitation of the illness, challenging a purely biological etiology of BD. This approach postulates that mania and depression are probably an automatic and repeated enactment of the brain’s initial response to a bygone stressful situation, but that the stressor may not be currently existent. Figuratively, this cyclical disorder is reminiscent of the Pandavas’ cyclical life in Hindu mythology; they moved between civic society and the hidden forest community; a pattern enforced on them in accordance with the penalty that they accepted for defeat at a game of dice with their cousins.
An autoimmune etiology of BD has been popularized by Immunopsychiatrists. The association of autoimmune disorders with schizophrenia is standard and well accepted. These relationships also existed for the broader category of non-affective psychosis. A small role for genetic link between pernicious anaemia in the family and raised risk for BD has been claimed by a few authors. Eaton et al. [10] suggests that a history of Guillain-Barré syndrome, Crohn’s disease, and autoimmune hepatitis in the individual was associated with raised risk of BD [10]. In my clinical practice, an association between Type 1 Diabetes Mellitus and BD has been observed. Recently, a Quantum Bioenergy Field (QBEF) in association with the material body has been brought to the equation of normal physiological functions. Thus, it has been hypothetically suggested that symptoms of BD may involve a swing between high-energy and low-energy states, and supposedly, disequilibrium of QBEFs may contribute to its symptom formation; the aetiology may be even an underlying medical condition [11]. The cognitive emptiness and emotional flatness of bipolar depression are also suggestive of QBEF involvement. Metaphorically, the build-up and release of energy is comparable to the automatic filling and emptying of a fluid tank disrupted due to some mechanical errors.
Bimodal Expressions
Mania occurs in two distinct forms, euphoric mania and dysphoric or mixed mania. Euphoric mania, in simple terms, is an energized pleasant mood. Dysphoric mania is also energized; however, it is characterized by certain symptoms of depression such as a negative mood. Sleep deprivation and tirelessness are important hallmarks of mania. The entire eye, including the lids, lashes, pupils and colour rings are extensively affected by mania. A person’s manic episode can be detected by looking for mania in the eyes, even before other manic symptoms become noticeable. Vision changes profoundly with euphoric mania-colours become very vivid and start to move around. With euphoric mania, there is an intense change in vision, as colours become very detailed and start to move around. In the manic state, the world is in Technicolor, and when severely depressed, it becomes black-and-white. Contrarily, in dysphoric mania vision is narrowed, and patients tend to squint and look angry around the eyes.
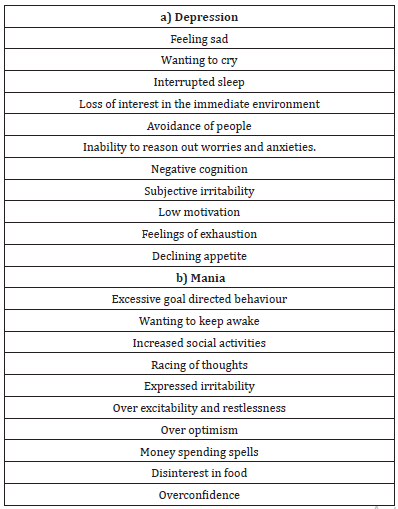
The following clues can be used to recognize mania in a person with bipolar disorder. Mania is devious and a manic patient wants to convince others that they are normal or better. Mania makes patients lie to themselves. Euphoric mania causes the liquid in the eyes to shimmer, making their eyes sparkle. People find this extremely attractive. Patients know how easy it is to get a relationship in the euphoric state and they focus these sparkling eyes on their unsuspecting prey who really get lost. Patients get darker eyes in dysphoric mania. These changes may be caused by adrenaline in the hypomanic state. With euphoric mania, the eyes usually widen, and they often get mean and narrow with dysphoric mania. In euphoric mania, the entire face brightens and actual eye-colour changes when manic. The first step in recognizing mania via physical changes is through the eyes. Movements of the shoulders (backward with euphoric mania and forward with dysphoric mania) are other physical changes in mania. Walking and hand movements change, and many physical behaviors speed up. Psychomotor excitability is a cardinal symptom of hypomania/mania (Table 2).
Bipolar depression raises specific diagnostic and therapeutic challenges. Only one-third of the patients receiving treatment with conventional mood stabilizers may experience adequate prophylaxis, most of the patients continue to be symptomatic. Two long-term follow up studies on BD 1 and ii disorders illustrated that depression is the dominating symptom in this illness: 146 patients suffering from type one 1 and 86 patients suffering from type 2 were followed up for a period of 12.8 years and 13.4 years, respectively [12,13]. Patients included in the bipolar type 1 were symptomatic during 47.3% of the follow-up weeks. Depression was the chief feature occurring during 31.9% of the follow-up weeks. The study noted 8.9% weeks for manic and hypomanic symptoms and 5.9% weeks for cycling and mixed symptoms. Patients included in the bipolar type 2 were symptomatic during 53.9% of follow-up weeks, depression predominating during 50.3% of the weeks. Hypomania and rapid cycling or mixed symptoms occurred during 1.3% and 2.3% of weeks, respectively. In clinical presentation, bipolar depression does not only vary from unipolar depression; the difference in optimum treatment is also significant. The condition is commonly misdiagnosed because of the similarities between its symptoms and those of major depression. Monopolar depression needs to be readily differentiated from bipolar depression because the inappropriate use of antidepressants may precipitate an affective switch. Bipolar depression should be considered when depression occurs without an identifiable psychogenic stressor [14]. The disease may be worsened if treatment is indefinite as a result of misdiagnosis.
The traditional view of BD is an abrupt onset of mania followed by depression with a euthymic phase between them, but longitudinal research and clinical studies prove otherwise, commonly an early onset of chronic mild depression and the first episode of BD is most often characterized by major depression [15]. Bipolar depression differs from other forms of depression because of the high risk both of completed suicide and psychotic features [16]. The manic symptoms may be colourful and depression is a less dramatic feature of the condition, but depression seems to hold the key to controlling and preventing the disorder. Bipolar depression covers a range of symptoms-including biological, cognitive, physical, and social features – and these domains should be carefully appraised. For most bipolar patients, depressive symptoms are significantly more debilitating than manic symptoms [17]. Major depression may to some extent be correlated with unipolar depression. The severity of the depression within the depressive episodes is variable, and this needs to be distinguished for treatment purposes.
In bipolar depressives, atypical depressive features are more recognizable, as is psychomotor retardation [18]. Patients also have a previous history of psychotic depression. Bipolar depression is associated with more mood lability and a relatively acute onset. When a young person presents with psychotic depression or psychomotor retardation, bipolar depression should be ruled out. Non-specific psychological symptoms and behavioral disturbances may be the precursor of BD in young people [19]. It is worth mentioning that patients presenting with depressive symptomatology should be thoroughly investigated, their past history of mood elevation as well as family history of affective disorders are important for accurate prognosis. Given the prevalence of and the disability associated with bipolar depression, the current arsenal of medication is inadequate. New research to help patients with this condition to reclaim their lives is overdue. The management of BD is dominated by too many uncertainties and the confusing guidelines for treatment worsen the situation. It may well be attributed to the dearth of rigorous research in this area. Depression in patients with this disorder is three folds as often as they are maniacal. With advancing age, depressive episodes outnumber the manic phase.
Prodromal Symptoms
Fire that is spread extensively is difficult to put out and should be stopped at the spark level. This is also the case with BD. Mania can fuel itself and depression can spiral down. Early intervention could prevent a full-blown relapse. Bipolar patients are able to report prodromal symptoms reliably (Table 2) and it is beneficial to teach patients to monitor their moods systematically and to promote healthy coping strategies [20]. Manic symptoms are seductive and in manic prodromal phase patients may have a tendency to give into the temptations and succumbing to them whereas in the depressive prodromal stage, patients may stay inactive hoping that symptoms will go away automatically [20]. Early warning signs of depression are more subtle than manic symptoms. Identifying these prodromal symptoms would help early intervention and prevent a massive relapse. Approximately 20% BD, patients suffer from OCD. Weakening of OCD symptoms has been noted and claimed in such patients as a heralding sign of the emerging elated period [21]. An earlier hypothesis suggests that OCD itself is a defense against psychosis, and figuratively, diminishing of OCD symptoms is like the bursting of the floodgates.
Table 2: Prodromes.
Differential Diagnosis
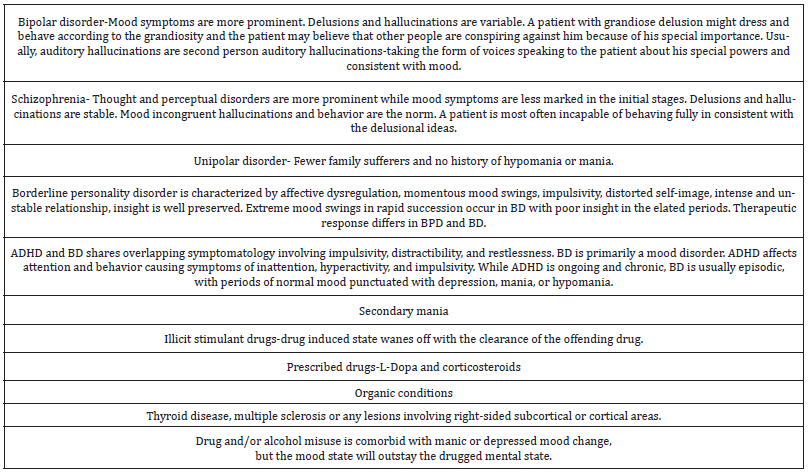
Diagnostic confusion between BD and schizophrenia may occur in the early stages because first rank symptoms of schizophrenia could be present as the illness unfolds initially; in 10-20% of manic patients Schneiderian first rank symptoms are evident. In schizoaffective disorder, mood symptoms and schizophrenic symptoms are both present and approximately in balance-neither type of symptom is sufficiently dominant to justify a diagnosis of either condition (Table 3). Difficulty in identifying BD may lead to delayed diagnosis and suboptimal treatment. Another significant factor is the episodic nature of the illness, an outcome of which is that the condition may be unrecognized, and therefore untreated, for years. Diagnostic uncertainty or mistaken diagnosis in the initial stages inevitably causes impediment in accurate recognition [22]. The diagnostic complexity of bipolar mania is further enhanced when a patient is seen for the first time when at the height of the illness. A subdued manic patient who has responded to sedative drugs will present a dilemma to the diagnostician because psychomotor excitability responds to medication earlier than hallucinations and delusions [23]. The pattern of mood cycles has individual specificity, but the pattern is predictable once the pattern is identified. The concept of broad-spectrum BD presents the therapist with the risk of medicalizing psychosocial problems and overprescribing mood stabilizers. Co-morbidities of BD like alcoholism and other psychoactive substance use disorders that are highly prevalent, contribute to the diagnostic conundrums of BD [24]. The finding of BD endophenotypes can improve early diagnosis, prevent errors in treatment and help elucidate the genetic susceptibility for this beastly disorder
Table 3: Differential diagnosis.
Late Life Onset
The prevalence of BD is underrated in the geriatric population and the illness holds the main features detected in the other cohorts, but it also has some specific characteristics in the older individuals. Rigorous research into BD in later life is lacking. The condition is often associated with organic aetiologies. One in six cases occurring for the first time in later life is thought to have its origins in multiple sclerosis, stroke, or steroid usage. When there is an organic aetiology, bipolar depression may not respond to antidepressants or mood stabilisers; such cases require elaborate physical investigation. Psychiatric and medical comorbidities tend to be more prevalent in the aged population. Higher rates of cognitive impairments than age- and education-matched groups present across all of the illness phases [25]. Higher rates of comorbidities and susceptibility to medication side effects make the treatment regime more problematic in the elderly. The clinical presentation of bipolar disorder in late life would be defined more frequently by depressive features and a predominantly depressive polarity and these results suggest that treatment strategies for elderly bipolar patients should focus on the prevention of depressive episodes [26].
Pregnancy and Postpartum Depression
Women with BD have a higher risk for pregnancy complications and congenital abnormalities than do women without BD. There are limited data to recommend discontinuing lithium, lamotrigine, or carbamazepine during pregnancy even though general consensus of opinion is to discontinue them [27]. Valproic acid is not recommended during pregnancy due to increased odds of neural tube defects associated with its use. Atypical antipsychotics are used more frequently during pregnancy, with mixed evidence regarding an association between these agents and congenital malformations or preterm birth [27]. Pregnancy and postpartum situations for patients suffering from bipolar depression are complex. Patients are routinely advised not to become pregnant while they are on prophylactic treatment, and to stop such medication if they become pregnant. Drugs are also withdrawn if the patient chooses to breastfeed her baby. The stress of childbearing and childbirth may cause a recurrence of illness. Bipolar women who are planning to get pregnant ought to be aware of the different types of stress they may have to face in the course of pregnancy and get prepared for them. Ability to adapt as a mother-parenteral self-identity is the first challenge. Pregnancy has great bearing with partner relationship. Parent infant attachment is another important challenge. Psychological and physiological state of mother is dynamic and needs adaptation. There are variations of presentation during every trimester and these changes during the different trimesters are to be considered separately.
During the first trimester, there may be emotional fluctuations between positive feelings such as excitement, happiness, and joy and rather negative ones such as disbelief, anticipation, worry, and tearfulness. This depends on a variety of factors, such as pregnancy ailments nausea, vomiting, reflux diseases, insomnia, planned or unplanned pregnancy, financial situations, family support, a perception of lifestyle restriction, and a sense of loss of independence. During the second trimester, the mood fluctuations may continue, and the negative feelings could sometimes lessen. Studies indicate that the mental health problems such as anxiety and depression occur less commonly in the second trimester in comparison to the first and third trimesters. In the third trimester, negative emotional feelings could come back more again. This could be due to increasing physical discomfort such as due to pelvic girdle pain, a backache, insomnia, tiredness, and exhaustion. A report of an ancient case of postpartum BD is found in the Old Testament. Hannah, the mother of Samuel, exhibits both a depressive and a manic phase. After a spell of depressive stupor during which “her lips were moving but her voice was not heard” (1 Samuel 1.13), she gives birth to her child and breaks into a manic episode. During this phase, she sings a song that constitutes an expression of extreme exaltation. Death and destruction to the oppressor, and supreme power and glory to the omnipotent creator, are exhorted in the song. Hyperbole is introduced to the seventh degree – as exemplified in the statement “she who was barren has borne seven”, though she had given birth to one child only [28]. The manifestation of bipolar depression presented here reminds us of its occurrence throughout history and its incidence at many stages of life. There is a need for initiatives that will improve the management of this condition and enhance the quality of life of those affected by it. The starting point is a renewed focus on academic research.
Suicidality
It is well established that pre suicidal risk is unpredictable in an individual [29]. Yet a clinician is in a position to assign a patient to a risk group-low risk, high chronic risk, high acute risk. In general, suicide is associated with acute bipolar depression but lower in-patients who receive long term treatment. An earlier statistical analysis of the incidence of suicides in patients with affective disorder inferred a lifetime risk of 15% [30]. After reviewing 13 additional studies Goodwin and Jamison concluded that 18.9% of depressed patients would die by suicide [31]. The risk of suicide in BD is about 30 times higher than in the general population. Suicidality is much higher among the bipolar depressives than in the maniacal phase-79.3% of the inpatients with BD posing suicidal risk whereas the suicidal risk was 2.3% among the maniacal patients. Coexistence of BD and personality disorder carries a much higher suicidal risk.
Mixed Affective States
Making a correct diagnosis of mood disorders can be an arduous task and this is particularly so when it comes to mixed states because patients will be focusing on their depressive and anxiety symptoms. The fleeting depression and mini highs make the clinical picture complicated. It is essential not to forget that the depression is only one phase of a broader bipolar mood disorder, and this has to be the illness to be treated by psychiatrists managing an appropriate polytherapy with mood-stabilizers and antidepressants [32]. A manic episode can be described to have mixed features (of depression) if there are three or more of subjective depression, worry, self-reproach/guilt, negative evaluation of self, hopelessness, suicidal ideation or behaviour, anhedonia, fatigue, or psychomotor retardation. A depressive episode can be said to show mixed features (of mania) if there are three or more of the following symptoms such as excitement, elevated mood, inflated self-esteem, pressure of speech, mind racing, increased energy, impulsivity, and lessened necessity for sleep. It is so vital to make a diagnosis of mixed manic-depressive states as it carries the highest morbidity of BD. The elated aspect of the added manic feature may heighten the risk of suicide.
Rapid Cycling
Suicidal risks, risks of accident and accidental death is high during the elated periods and the risks of impulsive and planned suicide becomes extremely high during low periods. More than four episodes per year are considered as rapid cycling. Cases with far frequent episodes are designated as ultra-rapid cycling and instances where mood swings occur within 24-hour period is recognized as ultra-ultra-rapid cycling or ultradian rapid cycling. BD is reported to be much commoner among female patients whose illness started at an earlier age [33]. While some authors argue it as a distinct subtype of BD, a few still argue that it is a transient complication of the long-term course of BD [34]. Depressive phase is anticipated to continue as the main clinical challenge.
Bipolar patients may run the risk of misdiagnosis and under diagnosis. The constructs of ultra-rapid and ultradian cycling have not been accurately corroborated. These terms could be misused to describe mood lability specifically rather than the full constellation of symptoms associated with a mood episode. It can also get confused with the variability to describe the variability that can occur within a mixed episode. DSM-5 makes no reference to ultra-rapid or ultradian cycling. Rapid cycling is the only such term that appears in the DSM, but sometimes the terms ultra-rapid and ultra-ultra-rapid (ultradian) cycling are used to illustrate more frequent mood episodes. Definitions may vary in individual circumstances, but on average ultra-rapid cycling is defined as a mania-depression cycle within a 48-72-hour period. Ultra-ultra-rapid (ultradian) cycling involves a full cycle occurring within a 24-hour period. The rarity of ultradian rapid cycling makes it riskier as many of the mental health staff are not familiar with this condition. Such a predicament may delay detection and intervention in times of a crisis. The dramatic presentation of type ii BD may even simulate dissociation state in rare cases (Table 4) or there could be a dissociation state in hypomania/mania. Dissociation states are more encountered in educationally backward cultures. Likewise, brief psychotic episodes could be bipolar manifestations [35].
Table 4: BD, and Dissociation state.

Comorbitities
Anxiety disorders comprise the commonest psychiatric co-morbidity of the bipolar spectrum [36] and anxiety has achieved the status of a separate specifier of BD in the DSM-V (APA 2013). As mentioned before, studies indicate that 20% of BD patients suffer from OCD. BD itself is incapacitating and OCD adds to their sufferings. There is some evidence to conclude that patients with BD are more prone to personality disorders than the normal population, but the incidence is lower when compared to unipolar affective disorders [37]. It is questionable whether coffee and alcohol are mood stabilisers or mood destabilisers but, unsafe in the hands of people suffering from this disorder. Both manic and depressed patients have a tendency to misuse alcohol, in the manic phase there is increased craving for alcohol while in the depressed phase they use it as self-medication. Likewise, bipolar patients are highly vulnerable to substance misuse. and it is a major comorbidity in B.D. patients. Bipolar patients with comorbid substance abuse may have a more severe course. Patients with substance abuse disorder get over diagnosed as B.D. as well as patients with B.D. get underdiagnosed as substance abusers. The “doubly troubled” patients need non-confrontational and non-threatening treatment approach.
Treatment Options
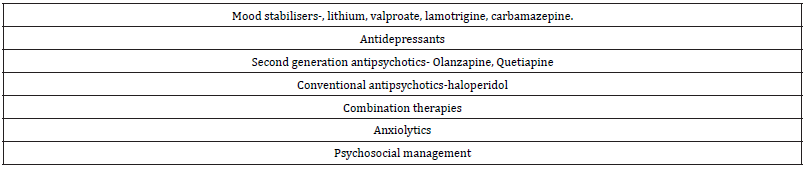
It may be interesting to note that the treatment guidelines for bipolar mania is similar worldwide, but the treatment guidelines for bipolar depression varies from country to country, sometimes substantially. An ideal treatment method should ameliorate acute depression and reduce abnormal mood elevation. The treatment strategies in acute depressive phase and long-term management should be considered separately and most often consist of the same medication with dose alteration and omitting the antidepressant. The aim of treatment should be remission rather than response and the former refers to reaching a stage where trouble symptoms no longer continue, and the latter only means a lowering of symptomatology persisting symptoms: response is three times easier to achieve than remission. Currently there are no agent licensed specifically, to treat bipolar depression but there are different treatment options consisting of monotherapy and combination therapies. Generally, polytherapy involving antidepressants, antimanic, mood stabilisers and anxiolytics are used in treating BD (Table 5).
Table 5: Treatments for BD.
Antidepressants
Even though there are several studies examining the efficacy of antidepressants in unipolar major depression, these studies did not include bipolar depression. There are only few placebo-controlled efficacy data for major depression arising in the course of BD and patients involved in such trials did not have marked symptoms. However, the general finding of antidepressant efficacy is applicable to bipolar depression. There is only a small quantity of evidence to decide between different agents in the treatment of bipolar depression. There are hardly any specific treatment recommendations for refractory depression occurring in the course of bipolar illness. In the past there has been an over utilization of antidepressants. The latent period to observe a favourable effect in response to antidepressant treatment in bipolar depression is similar to that of unipolar depression. There are several cautions to be born in mind while prescribing antidepressants. Anti-depressants can cause a manic switch and most guidelines for treating bipolar depression recommend discontinuing antidepressants within the first 3-6 months after remission [38-40]. If there is a single history of manic switch due to antidepressant treatment and a clear history of suicidal risk or homicidal risk in the manic phase, antidepressant will not be the right choice of treatment in that particular patient. Bipolar type ii where hypomania has not caused any untoward incident could be tried on antidepressant medication [41]. Antidepressants should be an adjunctive therapy to a mood stabilizer and antidepressant monotherapy is not recommended.
Uncertainties about antidepressants
Clinicians are apprehensive whether antidepressants may shorten the euthymic period. Tricyclics are associated with a treatment-emergent affective switch than other types of treatment. It is recognized that early discontinuation of antidepressants is desirable because of the uncertainty about long term use of antidepressants. Paradoxical manic episodes have been reported during the sudden withdrawal of antidepressants [42]. A clinician is thrown into the situation of being between the devil and the deep sea. An American study suggests that the risk of depressive relapse in patients with bipolar depression was significantly associated with discontinuing antidepressants soon after remission and also comments that the risk of manic switch was substantially less than the risk of depressive relapse [2]. Guideline for treatment with antidepressants suggesting discontinuation six months after remission was tested in this American study. The American study involved 84 patients with bipolar depression in remission following a combination therapy of antidepressant and mood stabiliser. About half of the study group discontinued their anti-depressant within six months and the rest remained on the combination for more than one year. Early discontinuation was associated with greater risk of relapse of depression and relapse rate was four times more likely overall with early discontinuation compared with continuing antidepressants for at least twelve months. They also observed that shorter duration of antidepressant therapy was also associated with an increase relapse of manic symptoms after a shorter time, with the greatest risk within the first six months Mood stabilisers.
Across the Atlantic, mood stabilising agents are the first line treatment for bipolar depression before considering antidepressants. Currently the popular ones are lithium, valproate, lamotrigine, and carbamazepine. There is no consensus definition of an ideal mood stabiliser. The view that an ideal mood stabiliser is a drug that would decrease the frequency or severity of any type of episode in BD without worsening the frequency or severity of other episodes is the most liberal attitude [43,44]. A stringent definition would be that an ideal mood stabiliser should have four distinct capacities- it should be useful in the treatment of acute manic and acute depressive symptoms as well as it should be capable of preventing manic and depressive symptoms [45]. Unfortunately, such a mood stabiliser is not proven to exist.
Lithium carbonate is essentially an antimanic agent with modest antidepressant effect: it has been the gold standard for treatment of BD for half a century. It is still the main stay of treatment in U.K even though there are well observed short term and long-term side effects attached to lithium treatment. The therapeutic range of lithium is narrow and plasma level monitoring is required to ensure that a patient remains within the recommended therapeutic plasma levels to avoid toxicity. One third of patients are lithium non responders and the number of patients discontinuing from lithium therapy are also quite high [46]. Lithium has been associated with suicide prevention. Overdose with lithium carries more mortality than other mood stabilisers. It is the hypothesis based on kindling phenomenon and the observation that anticonvulsant has a mood stabilising effect in epileptic patients, that introduced them to bipolar pharmacopoeia [47], but there is no clear evidence to consider that depression and epilepsy have a shared aetiology. Valproate is a single branched chain fatty acid. Open studies of valproate monotherapy have favoured a prophylactic effect against mania but not depression. Valproate semisodium is prescribed as a mood stabiliser in bipolar disorder and it is a mixture of two similar ingredients - valproic acid and sodium valproate. Sodium valproate (especially if started as a fixed dose intravenous infusion of 1200mg/day for the first 3-5 days) is a highly efficacious, cost-effective treatment approach for hard-to-treat acute mania [48].
Lamotrigine is a phenyltriazine-derived anticonvulsant and has robust antidepressant activity. The mechanism of action of lamotrigine is different from other anticonvulsant and mood stabilisers. The efficacy of lamotrigine in the treatment of bipolar depression has been demonstrated in a randomised, double blind clinical trial comparing two doses of lamotrigine, fifty and two hundred doses with placebo. A clinical response was noted for 48% and 56% of patients treated with low dose and high dose lamotrigine, respectively, in comparison with 29% of patients treated with placebo [49]. Other studies also have yielded favourable results [50,51]. Lamotrigine should be titrated slowly as rapid titration enhances the risk of developing skin rashes. Lamotrigine also have caused delirium, confusion, depression, and psychosis [52]. Because early manifestations of hypersensitivity may occur in the absence of rash, patients with these symptoms should be evaluated immediately. Prior to initiation of therapy, patients should be warned that rash, fever, lymphadenopathy may be symptomatic of a serious adverse reaction. Lamotrigine is more effective against depression than mania in the long-term treatment and is the drug of choice where depression is the major burden of the illness, but special care needs to be taken against the adverse side effects. Calabrese et al has presented the outcomes for the rapid cycling patients maintained on placebo or lamotrigine and it seems lamotrigine is a useful drug for the condition even though treatment efficacy outcome criteria for rapid cycling patients are not well established [53].
The Carbamazepine is a dibenzapine derivative. A number of open and small-scale controlled studies of carbamazepine in depression indicates a possible antidepressant effect, but the studies lack clear evidence to prove its antidepressant property [54]. Carbamazepine has been associated with higher incidence of suicide attempts and completed suicides [55]. The use of Carbamazepine and Valproate in the treatment of acute bipolar depression is not evidence based [24].
Second generation antipsychotics
Traditional antipsychotics came to be introduced into the treatment regime of bipolar depression, not because they have antidepressant properties, but to take advantage of their anxiolytic and hypnotic properties. As they are available in the depot form, typical antipsychotics are used to ensure medication adherence even though with the advent of atypical antipsychotics the use of depot preparation has decreased. Anxiety is an incapacitating symptom of bipolar depression. The recent media intolerance towards benzodiazepines contributed to the overuse of antipsychotics in treating anxiety symptomatology in psychiatric patients in general. 47%-90% of patients are prescribed antipsychotics alone or in combination with mood stabilisers [56]. Conventional anti psychotics were thought to be pro-depressants causing switch from mania to depression than treatment with lithium and valproate. With the exception of a 6-month perphenazine study, there are no other randomized study of typical antipsychotics that support the belief that this class of medications worsen bipolar depression. The use of haloperidol in the acute phase of mania is still a common practice and is highly effective. In fact, a few drops of timely administration of haloperidol could prevent escalation of manic episode and has speedier effect. The atypical antipsychotics appear to have a better antidepressant profile than the traditional ones [57,58]. This claim has been verified in large, double-blind, placebo-controlled clinical trials. The therapeutic response of lithium usually occurs only in the second week of treatment and is slower than the response to atypical anti-psychotic drugs such as quetiapine. The antidepressant property of atypical may be related to the fact that they combine5-HT2A inhibition and down-regulation, as well as D2 antagonism [59]. The novel antipsychotics are approved for acute mania but their efficacy in acute depression and prophylaxis of depression is under investigated.
Olanzapine has shown a smaller effect size, while olanzapine-fluoxetine combination has shown a moderate effect in patients with bipolar type 1 depression [60]. In a recent American study, Quetiapine has shown a large therapeutic effect size in a group of patients including those with bipolar 1 or ii depression [61]. The study found that Quetiapine monotherapy was effective and well tolerated thus proving that the drug has anti manic and antidepressant properties in the treatment of BD. Their study involved five hundred and forty-two outpatients with bipolar 1 or 11 disorder who had major depressive symptomatology and were randomly assigned to 8 weeks of oral quetiapine (600 or 300mg/day) or placebo. Quetiapine at 600 and 300mg/day significantly improved nine of 10 and 8 of 10 Montgomery-Asberg depression rating scale items, respectively, compared with placebo, including the core symptoms of depression. They also noticed that treatment emergent mania was low and similar for the quetiapine and placebo groups (3.25 and 3.9% respectively). Quetiapine has anxiolytic and hypnotic properties, and this could be an added advantage. Large prospective studies are warranted to test the validity of these findings. Only time will tell whether Quetiapine merits the label as a “Bimodal activity- bipolar antipsychotic”. Risperidone, amisulpiride and aripiprazole are also used on the basis of individual requirements. The antidepressant property of other atypical antipsychotics including Lurasidone remains to be ascertained. Clozapine is used as a sheet anchor for treatment resistant BD, but there are no blinded studies of its use in BD [62].
Use of adjunctive therapies
Regrettably, two-thirds of outpatients treated even in academic centres remain moderately symptomatic and disabled by depression. They all experience residual symptoms more frequently and treatment generally involve combination therapies. Common prescribing practices include the use of several mood stabilisers in combination with atypical antipsychotics, second-generation antidepressants, and anxiolytics. It is true that the efficacy of drugs is lost over time in monotherapy. Combination therapy is recommended by mood specialists initially or in the event of monotherapy failure. Clinicians need to balance the potential benefits of any adjunctive therapy against the risk of side effects and interactions. Moreover, the added drug should be introduced gradually.
The effectiveness of a rational polypharmacy approach is supported by some research data [63], but they also increase the side effects. Substantial treatment data exist regarding the combination of lithium and carbamazepine, but the latter has a history of suicide. The antimanic and superior anti-depressant effects of lithium and lamotrigine, respectively, can be taken advantage of, if these drugs are given in combination; a promising combination treatment paradigm that warrants further investigation [64]. Based on available observational findings, combining lamotrigine with other mood stabilising drugs or an atypical antipsychotic to attain better mood stability makes intuitive sense. Nevertheless, the effectiveness of these combination strategies has not been compared with monotherapy. Theoretically, it a valuable idea to combine lamotrigine with lithium or valproate or an atypical antipsychotic, but more prospective studies are warranted. Pharmacokineticlly, valproate doubles lamotrigine levels. Oral contraceptive efficacy may be affected by Lamotrigine.
Neurotoxicity can result from possible pharmacodynamic interactions between lamotrigine and carbamazepine [65]. Similarly combining lamotrigine and quetiapine may be a valuable idea to treat severe bipolar depression. Logically speaking, since both drugs have antidepressant properties, a manic switch could result from their combination. There should be considerations for future trials testing whether the antimanic effect of quetiapine would counterbalance the risk of a manic switch due to the combined antidepressant effect of these two agents, and this requires a closer scrutiny [66]. Lamotrigine could potentially cancel the effect of contraceptive pills and oral contraceptives have been shown to reduce blood levels of lamotrigine. Adding semi-sodium valproate could double the blood levels of lamotrigine and can be effective in treatment-resistant BD. Rapid cycling BD carries a high comorbidity risk and a combination of mood stabilisers may become an inevitability; achieving bimodal stability is a herculean task.
There is criticism against readily using heavy-duty antipsychotics to treat bipolar type ii depression when antidepressants and mood stabilisers could be given a proper trial. The scientific literature does not offer any clear guidelines to choose these agents to achieve and sustain remission. Recently, there has been an attempt to formalise the current treatment combinations in a better conceptual framework for mood stabilisation. According to this framework, “below the base line” refers to depressive symptoms and “above the baseline” includes mania, mixed states and hypomania. An individual’s responsiveness and tolerability are reliable methods of establishing the best combination regime. How all these combinations will fare in the long-term prophylaxis remains to be seen.
Electroconvulsive therapy
Electroconvulsive Therapy (ECT) has often been used in the past where more resistant depression is encountered more frequently. NICE guidance on ECT and depression clearly indicate that ECT should be held in reserve, rather than is an early treatment option. With the currently available treatments with SSRIs and taking into consideration the risk of switching into hypomania or mania, this is a fair position to adopt, but where ECT has worked in the past and where a patient is actively suicidal, it still remains a lifesaving option. ECT is also useful in treating bipolar depression during pregnancy and refractory cases of depression. The public fear that ECT is even administered against the will of patient is groundless and the results of this specific treatment methods are favourable [67].
Psychosocial management
Despite the dazzling progress in pharmacopeia, BD is marked by recurrent episodes, and these have become the norm. Relapse rates reaching 40%, 60%, and 73% in 1 year, 2 years, and 5 or more years, respectively have been suggested by longitudinal studies [68,69]. Although mood stabilisers have been used generously, poor results still characterize the outcome of bipolar depression [70]. Adherence to medication is estimated to be poor in one-half to two-thirds of patients within the first 12 months of treatment [71]. Such findings prompt clinicians to search for additional modalities of intervention for BD. There is the need to treat the whole person that would include the physical and social needs. It is also equally important to educate patients and carers about the disorder and its treatment options. Ongoing psychotherapy is essential to ensure compliance with medication and to help to resolve the effects of the disorder on family, employment and working environment. It is important to give positive self-esteem to the patient, as bipolar relapses are an assault on the patient’s social dignity and self-image. Construction of life charts of mood symptoms and life events may help patients optimally. Patients’ involvement in treatment programmes is the key predictor of positive outcomes. A negative therapeutic alliance can also occur innocently from the part of the mental health staff as well as from the part of patients, which can be attributed to the very nature of the illness.
Of the various psychosocial interventions used in BD, the three largest published studies employed either CBT [72], Family therapy [73] or Group Psychoeducation [74]. Psychosocial interventions also include teaching bipolar patients to cope with prodromal symptoms to prevent full-blown episodes [75,76].
Discussion
Unmet clinical needs persist in all phases of the bipolar disorder. Depression and mania are probably two sides of the same coin but require different treatment approaches. Agents with “bimodal” activity, in the sense, ameliorating acute depression and reducing abnormal mood elevation are desirable to treat bipolar depression. Even though lamotrigine’s antimanic effect is modest, it appears to have robust anti-depressant properties in bipolar depression and is a useful drug to combine with other agents for long term relapse prevention. Because of the risk of adverse reactions, it may be reserved for more refractory cases and in patients presenting with intolerance to traditional mood stabilisers [54]. Quetiapine’s antidepressant value needs to be ascertained further. A steady stream of new data is required to further elucidate the role of currently available treatment options. It is even anticipated that because of the observed favorable effects of the newer antipsychotics on BD, the therapeutic and diagnostic boundaries between this disorder and schizophrenia could be blurred in the years to come and necessitate a new classification of mood stabilizing agents in comparison with anti-psychotics. A dearth of authentic research in the management of bipolar depression has resulted in multiple uncertainties. Given the time period bipolar patients spend in the depressive phase, new modes and novel approaches to treatment are immensely important. Stem cell research may hold promise of a cure.
The recognition of the core features of bipolar depression, the threshold symptoms for treatment, the optimal treatment choices for monotherapy or combination therapy are important issues that warrant further investigations. As the optimal duration of maintaining antidepressant therapy has not been established empirically and, until better evidence-based guidelines are available, antidepressant therapy should be tailored on an individual basis. NICE is currently in the process of producing guidelines for BD. In the meantime, there are several guidelines available. Thanks to psychopharmacology, there are more drugs options now than a few decades ago. The choice of treatment should be made on the needs of the individual patient. Evidence for the efficacy and safety of novel therapies such as stimulants, phototherapy, omega-fatty acids, Transcranial magnetic stimulation, and sleep deprivation for bipolar depression remains unconvincing and is totally without experimental support. The clinician and the patient collaborating and carefully considering all available treatment options may ultimately lead to the correct choice of a treatment plan.
References
- Merikangas K, Yu K (2002) Genetic epidemiology of bipolar disorder. Clin Neurosc Res 2(3-4): 127-141.
- Angst F, Stassen HH, Clayton PJ, Angst J (2002) Mortality of patients with mood disorders follow up over 34-38 years. J Affective disorders 68(2-3): 167-181.
- Badner JA, Gershon ES (2002) Meta-analysis of whole-genome linkage scans of bipolar disorder and schizophrenia. Mol Psychiatry 7(4): 405-411.
- Johansson V, Halkola RK, Cannon TD, Hultman CM, Hedman AM (2019) A population-based heritability estimate of bipolar disorder-in a Swedish twin sample. Psychiatry Res 278: 180-187.
- Craddock N, Sklar P (2013) Genetics of bipolar disorder. Lancet 381(9878): 1654-1662.
- Haggarty SJ, Karmacharya R, Perlis RH (2020) Advances toward precision medicine for bipolar disorder: mechanisms & molecules. Molecular Psychiatry 26(1): 168-185.
- Holmgren A, Hansson L, Kjeldal KB, Impellizzeri AAR, Gilfillan GD, et al. (2022) Mapping the expression of an ANK3 isoform associated with bipolar disorder in the human brain. Transl Psychiatry 12: 45.
- Catherine Slattery, Mark Agius & Rashid Zaman (2010) Bipolar disorder associated with paraneoplastic cerebellar degeneration: A case report. Psychiatria Danubina 22(Suppl 1): 137-138.
- Post RM, Ketter TA, Denicoff K, Pazzaglia PJ, Leverich GS, et al. (1996) The place of anticonvulsant therapy in bipolar illness. Psychopharmacology 128(2): 115-129.
- Eaton WW, Pedersen MG, Nielsen PR, Mortensen PB (2010) Autoimmune diseases, bipolar disorder, and non-affective psychosis. Bipolar Disord 12(6): 638-646.
- Pandarakalam JP (2020) Interactions of quantum bioenergy fields. Neuro Quantology 18(2):157-172.
- Judd LL, Akiskal HS, Schletter PJ, Endicott J, Maseret J, et al. (2002) The long-term natural history of the weekly symptomatic status of bipolar I disorder. Archives of General Psychiatry 59(6): 530-537.
- Judd LL, Akiskal HS, Schletter PJ, Coryell W, Endicottet J, et al. (2002) A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. Archives of General Psychiatry 60(3): 261-269.
- Pandarakalam JP (2007) Clinical challenges of bipolar depression. British Journal of Hospital Medicine 68(10): 530-531.
- Pandarakalam JP (2007) Depressive expression of bipolar disorder. Irish Psychiatrist 8(6): 247-253.
- Hirschfild RMA, lewis L, Vornik LA (2003) Perceptions and impact of bipolar disorder, hoe far have we really come? results of the national and depression and manic-depressive association, survey of Individuals with Bipolar Disorder. J Clin Psychiatry 64(2): 161-174.
- Akiskal HS, Walker P, Puzantian VR (1983) Bipolar outcomes in the course of depressive illness: phenomenological, familial, and pharmacological predictors. J Affective disorders 5(2): 115-128.
- Calabrase JR, Hirschfild RMA (2004) Impact of depressive symptoms compared with manic symptoms in bipolar disorder: Results of a US community-based survey. J Clin Psychiatry 65(11): 1499-1504.
- Mitchell PB, Wilhelm K, Parker G, Austin MP, Rutgers P, et al. (2001) The Clinical features of bipolar depression: a comparison with matched major depressive disorder patients. J Clinical Psychiatry 62(3): 212-216.
- Lam D, Wong G, Sham P (2001) Prodromes, coping strategies and course of illness in bipolar affective disorder-A naturalistic study. Psychological Medicine 31(8): 1397-1402.
- Sanil R (2018) Obsessive Compulsive Disorder(OCD)-A primer on neurobiology, diagnosis and treatment. Psych scene hub.
- Goodwin GM (2003) Evidence-based guidelines for treating bipolar disorder: recommendations from the British Association for Psychopharmacology. Journal of Psychopharmacology 17(2): 149-173.
- Lish J, Meenan SD, Whybrow PC, Price RA, Hirschfield RM (1994) The national depressive and manic-depressive association survey of bipolar members. J Affective Disorders 31(4): 281-294.
- Pandarakalam JP (2008) Diagnostic conundrums of bipolar disorder. Progress in Neurology and Psychiatry 12(6): 6-11.
- Shobassy A (2021) Elderly bipolar disorder. Curr Psychiatry Rep 23(2): 5.
- Nivoli AM, Murru A, Pacchiarotti I, Valenti M, Rosa AR, et al. (2014) Bipolar disorder in the elderly: a cohort study comparing older and younger patients. Acta Psychiatr Scand 130(5): 364-373.
- Scrandis DA (2017) Bipolar disorder in pregnancy: A review of pregnancy outcomes. J Midwifery Womens Health 62(6): 673-683.
- James Alexander (1962) Postpartum psychiatric problems. Hamilton, California, USA, p. 163.
- Mackinnon DR, Farberow NL (1976) An assessment of utility of suicide prediction. Suicide Life Threat 6(2): 86-91.
- Pokorny AD (1993) Suicide prediction revisited. Suicide Life Threat Behaviour 23(1): 1-10.
- Guze SB, Robins E (1970) Suicide and primary affective disorders. Br J Psychiatry 117(539): 437-438.
- Goodwin GM, Jamison KRT (1990) Manic-depressive illness. Oxford University Press, New York, USA.
- Tavormina G (2014) Treating the bipolar spectrum mixed states: a new rating scale to diagnose them. Psychiatr Danub 26(Suppl 1): 6-9.
- Montgomery SA, Schatzberg AF, Guelfi JD, Kasper S, Nemeroff C, et al. (2000) Pharmacotherapy of depression and mixed states in bipolar disorder. J Affective Disorder 59(Suppl 1): S39-S56.
- Marneroes A, Pillmann P (2004) Acute and transient psychoses. Cambridge: Cambridge University Press, UK.
- Karam EG, Salamoum MM, Yeretzian JS (2010) The role of anxious and hyperthymic temperaments in mental dis orders: a national epidemiologic study. World Psychiatry 9(2): 103-110.
- Brieger P, Ehrt U, Maarneros A (2003) Frequency of comorbid personality disorders in bipolar and unipolar affective disorders. Compr Psychitry 44(1): 28-34.
- Frances A, Khan D, Carpenter S, Dorothy J, Donovan S (1998) The expert consensus guidelines for treating depression in bipolar disorder. J Clinical Psychiatry 59(suppl 4): 573-579.
- Yatham L, Kusumakar V, Parikh S, Haslam D, Matte R, et al. (1997) Bipolar depression: treatment options. Can J Psychiatry 42(suppl 2): S87-S91.
- Sachs GS (1996) Treatment-resistant bipolar depression. Psychiatr Cln North Am 19(2): 215-236.
- Kusumakar V (2002) Antpsychotics and antidepressants in the long-term treatment of bipolar disorder. J Clinical Psychiatry 63(Suppl 1): 23-28.
- Goldstein TR, Frye MA, Denicoff KD, Jackson ES, Leverich GS, et al. (1999) Antidepressant discontinuation related mania: Critical prospective observation and theoretical implications in bipolar disorder. J Clinical Psychiatry 60(8): 563-567.
- Bowden CL, Mitchell P, Suppes T (1999) Lamotrigine for the treatment of bipolar disorder. Eur Neuropsychopharmacology 9(suppl 4): S113-S117.
- Ketter TA, Calabrese JR (2002) Stabilization of mood from below versus above baseline in bipolar disorder: a new nomenclature. J Clin Psychiatry 63(2): 146-151.
- Mark BS, Landis M (2004) What is a mood stabiliser? An evidence-based response. Am J Psychiatry 161(1): 3-18.
- Post RM (1990) Non-lithium treatment for bipolar disorder. J Clin Psychiatry 51: 9-16.
- Sussman N (1997) Gabapentin and lamotrigine: Alternative agents for the treatment of bipolar disorder. Primary Psychiatry, pp. 25-42.
- Luchezar GH, Petra M, Maria S, Milena P, Georgi H (2013) Bipolar disorder-from endophenotypes to treatment. Psychiatry Danubina 25(3): 284-291
- Calabrese JR, Rapport DJ (1999) Mood stabilisers and the evolution of maintenance study designs in bipolar 1 disorder. J Clin Psychiatry 60(suppl 5): 5-13.
- Bowden CL (1999) New concepts in mood stabilisation: Evidence for the Effectiveness of Valproate and Lamotrigine. Neuropsychopharmacology 19(3): 194-199.
- Frye MA, Ketter TA, Kimbrell TA, Dunn RT, Speer AM, et al. (2000) A placebo-controlled study of lamotrigine and gabapentin monotherapy in refractory mood disorders. J Clinical Psychopharmacology 20(6): 607-614.
- Ferrier IN (1998) Lamotrigine and Gabapentine. Alternative in the treatment of bipolar disorder. Neuropsyhobiology 38(3): 192-197.
- Calabrese JR, Suppes T, Bowden CL, Sachs GS, Swann AC, et al. (2000) A double blind, placebo-controlled, prophylaxis study of lamotrigine in rapid cycling bipolar disorder. Lamictal 614 Study Group. J Clinical Psychopharmacology 61(11): 841-850.
- Richard P, Nicol F, Heather A (1999) Anticonvulsants as mood stabilisers. Advances in Psychiatric Treatment 5(2): 96-103.
- Flechtner KT, Oerlinghausen BM, Seiberet W, Walther A, Greil W (1996) Effect of prophylactic treatment on suicide risk in patients with major affective disorders. Data from a randomized perspective trial. Pharmacopsychiatry 29(3): 103-107.
- Mallakh El, Ghaemi N (2006) Bipolar depression: A comprehensive guide. American Psychiatric Publishing, Washington, USA.
- Bowden CL (2005) Atypical antipsychotic augmentation of mood stabiliser therapy in bipolar disorder. J Clinical Psychiatry 66(suppl3): 12-19.
- Dunner DL (2005) Atypical antipsychotics: Efficacy across bipolar disorder subpopulations. J Clinical Psychiatry 66(Supp 3): 20-27.
- Yatham LN, Goldstein JM, Vieta E (2005) Atypical antipsychotics in depression: potential mechanism of action. J Clin Psychiatry 66(suppl5): 40-48.
- Tohen M, Vieta E, Ketter TA, Sachs G, Bowden C (2003) Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar 1 depression. Archives General Psychiatry 60(11): 1079-1088.
- Calabrese JR, Keck PEJR, Macfadden W, Minkwitz M, Ketter TA, et al. (2005) A randomised, double-blind, placebo-controlled trial of quetiapine in the treatment of bipolar 1 or ii depression. Am J Psychiatry 162(7): 1351-1360.
- Andreas M, Frederick G (2005) Bipolar disorders. Cambridge University Press, Cambridge, UK.
- Freeman MP, Stoll AL (1998) Mood stabiliser combinations: a review of safety and efficacy. Am J Psychiatry 155(1): 12-21.
- Post RM (2006) What is an ideal mood stabiliser? Clinical approaches in bipolar disorders 5: 14-20.
- Dubovsky SL, Buzan RD (1997) Novel alternatives and supplements to lithium and anticonvulsants for bipolar affective disorder. J Clin Psychiatry 58(5): 224-242.
- Pandarakalam JP (2007) Search for Bi-model activity in BD. Progress in Neurology and Psychiatry 11(5).
- Wheeldon TJ, Robertson C, Eagles JM, Reid IC (1999) The views and outcomes of consenting and non-consenting patients receiving ECT. Psychol Med 29(1): 221-223.
- Gitlin MJ, Swendsen J, Heller TL, Hammen C (1995) Relapse and impairment in bipolar disorder. Am J Psychiatry 152(11): 1635-1640.
- O Connell RA, Mayo JA, Flatlow L, Cuthbertson B, Brien BEO (1991) Outcome of bipolar disorder on long-term treatment with lithium. Br J Psychiatry 159: 123-129.
- Keck PE, McElroy SL, Strakowski SM, West SA, Sax KW, et al. (1998) 12-Month outcome of patients with bipolar disorder following hospitalization for a manic or mixed episode. Am J Psychiatry 155(5): 646-652.
- Keck PE, McElroy SL, Strakowski SM, Stanton SP, Kizer DL, et al. (1996) Factors associated with pharmacologic noncompliance in patients with mania. J Clin Psychiatry 57(7): 292-297.
- Lam DH, Watkins ER, Hayward P, Bright J, Wright K, et al. (2003) A randomized controlled study of cognitive therapy for relapse prevention for bipolar affective disorder: outcome of the first year. Archives of General Psychiatry 60(2): 145-152.
- Miklowitz DJ, George EL, Richards JA, Simoneau TL, Suddath RL (2003) A randomized study of family-focused psychoeducation and pharmacotherapy in the outpatient management of bipolar disorder. Arch Gen Psychiatry 60(9): 904-912.
- Colom F, Vieta E, Aran AM, Reinares M, Goikolea J M, et al. (2003) A randomized trial on the efficacy of group psychoeducation in the prophylaxis of recurrences in bipolar patients whose disease is in remission. Archives of General Psychiatry 60(4): 402-407.
- Perry A, Turner N, Morriss R, McCarthy E, Limb K (1998) Randomised controlled trial of efficacy of teaching patients with bipolar disorder to identify early symptoms of relapse and obtain treatment. British Medical Journal 318(7177): 149-153.
- Scott J, Garland A, Moorhead S (2001) A pilot study of cognitive therapy in bipolar disorders. Psychological Medicine 31(3): 459-467.
© 2022 James Paul Pandarakalam. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






