- Submissions

Full Text
Gerontology & Geriatrics Studies
Cancer and Virtual Reality VR, the Great Challenge of the Century
Sakhri Selma Épse Boulhart*
Department of medical oncology service, Algeria
*Corresponding author: Sakhri Selma Épse Boulhart, Department of medical oncology service, Algeria
Submission: December 01, 2021; Published: January 21, 2022
ISSN 2578-0093Volume7 Issue4
Introduction
The number of new cases of cancer is constantly increasing around the world. The lengthening of life expectancy and therefore the aging of the population largely explain this increase in the number of cancers, in particular (prostate cancer in men, breast cancer in women, colorectal or gastric cancers). The diagnosis, the associated treatments as well as the more or less long-term sequelae represent a multitude of stressful situations. It has thus been shown that more than 10% of patients treated for cancer present the clinical symptoms of an anxiety disorder [1] and this prevalence reaches nearly 17.6%, in patients living with cancer for more than two years [2]. Virtual reality is a therapeutic aid, but it also has its place in the training of doctors in oncology and in cancer diagnosis. Medical oncology as a whole and virtual reality have a promising future.
Virtual reality for patients
Virtual reality has found its place with patients as a therapeutic aid. For a large number of pathologies, such as cancer, it is used because it is a revolutionary technology but above all gentle and without side effects [3]. VR refers to the interactions between an individual and a computer-generated environment stimulating multiple sensory modalities, including visual, or auditory experiences, The user's perception of reality is facilitated by the use of headsets (HMD, in glasses or helmets), (Figure 1). Translated from French to English - www.onlinedoctranslator.com
Figure 1: VR virtual reality headset. PLOS ONE | https://doi.org/10.1371/journal.pone.0219115 August 14, 2019.

To fight the pain
VR is the most useful and used in this area. In developed countries, many oncology departments use virtual reality to help their patients fight against pain related to the disease or following a biopsy. Almost half of hospital patients experience pain, a quarter of which is considered "un-bearable" [4]. The treatment of pain has traditionally been based on pharmacological management, including opioids, which can give inconsistent and suboptimal results. Therapeutic Virtual Reality (VR) has become an effective and non-pharmacological treatment modality for pain [4,5]. VR users wear a head-mounted display with a proximity screen that creates a feeling of being transported to realistic three-dimensional worlds (Figures 1 & 2).
Figure 2: Virtual reality for pain relief in hospitals Huffpost Canada 2021
A proposed mechanistic theory of VR suggests that by stimulating the visual cortex while engaging other senses, VR acts as a distraction to limit the user's processing of nociceptive stimuli [6]. The ubiquity of high-performance mobile computing has now reduced both the size and cost of virtual reality devices, enabling its use in everyday clinical environments (Figures 3 & 4). To date, VR has been used in many clinical settings in oncology, to help treat anxiety disorders, control pain, support physical rehabilitation, and distract patients during chemotherapy, [4,6] of Likewise, VR reduces pain and provides positive distraction during procedures, such as intravenous line placements [6].
Figure 3:the virtual reality headset decreases the anxiety of the intensive care patient Healthy/mind 05/10/2021.9.

Figure 4: Virtual reality and augmented reality-based visualization of scientific experimental imaging data, toolsfor surgery and anatomy, and collaborative interfaces for education and telehealth [7].
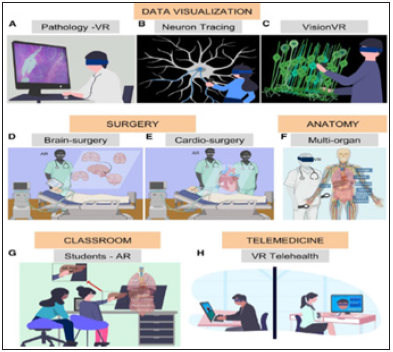
HuffPost Canada 2021
To better manage a hospitalization
VR is indeed an ideal tool to help adult patients and children to fight against stress but also trouble for chemotherapy sessions, it is a technology that will help them keep morale during these sessions. Several controlled VR trials in hospitals have been published in the last 10 years
For cancer patients in palliative care
Virtual reality is indicated for anxious patients: There are many anxiety-generating situations in palliative care (announcement of disease progression, care, chemotherapy sessions, radiotherapy, etc.) Often linked to anxiety attacks, the associated pains wake up or are increased. The use of headphones could therefore soothe these patients by diverting their attention, and thus re-duce the pain crisis (Figure 5).
Figure 5:Case studies using virtual reality and augmented reality [7].
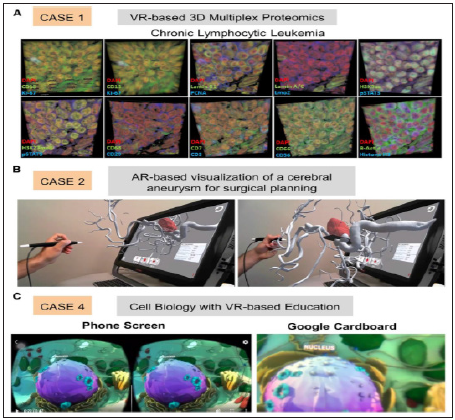
The virtual reality headset can help prevent pain
Linked to certain treatments (installation of a peripheral venous route, Huber needle, indwelling catheter, carrying out blood gases, etc.) and during the repair of complex dressings (dilapidated, very painful tumor wounds, sources of anxiety, etc.)
This device can be used in addition to the usual therapies
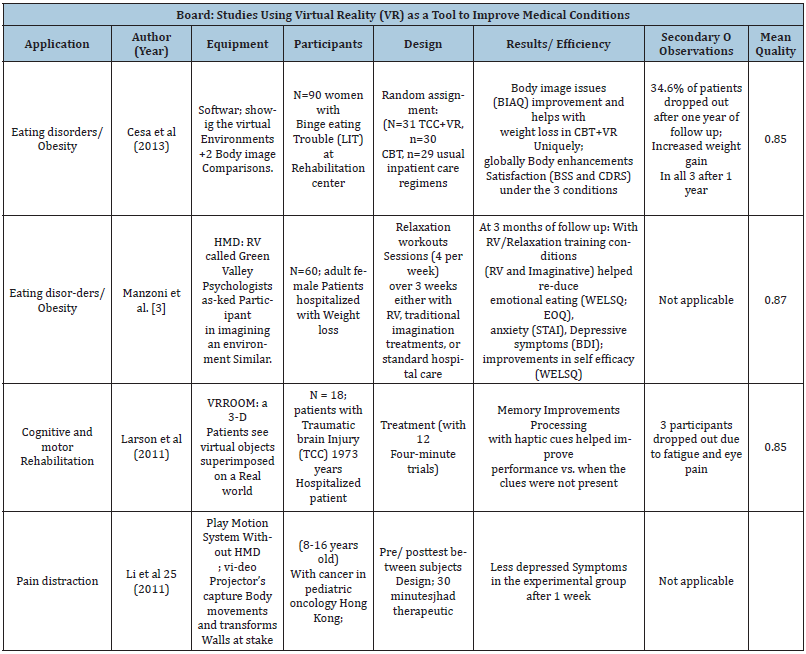
Like anxiolytics, neuroleptics or analgesics. It may also be of interest for patients who are resistant to taking medication (Table 1).
Table 1:
To train doctors
For medicine, its use in the field of health has focused on technical and educational applications (eg, preparation for surgery through simulations of surgical acts, medical evaluations), but also in therapeutic management - known as therapy by VR exposure - of certain pathologies such as cancer, anxiety disorders, psychosis, and certain forms of depression) [7,8].
For virtual training of surgeons and biomedical devices
Surgeons require specific skills requiring extreme practice and dedicated training, but this process can be difficult for medical trainees. Virtual reality offers students the opportunity to perform a low-risk procedure before performing surgery on an individual to resolve this problem. Students develop skills such as on-site thinking, problem-solving in a hands-on environment, and performing tasks in a stressful environment. Virtual reality-based training has unique advantages. VR makes it easier to work with various deep organs that may be physically obstructed by others and, therefore, difficult to observe during conventional surgical training. VR can be used as a training approach to transfer procedural knowledge in the bio-pharmaceutical industry, replacing traditional reading of long manuals [8].
Experiential biomedical education tools for teaching
Virtual reality enhances the learning experience of students by teaching new concepts of molecular biology in cancerology [7-9]. For a generation living a digital lifestyle, attention span has dramatically decreased thanks to media technologies [2-7]. VR as an educational tool offers feasible digital solutions to this problem as students focus on a virtual space where distractions are greatly reduced. One approach to using virtual reality in classrooms is to provide students with headsets synchronized with a central device to experience the same content. It can also be decentralized, where medical lessons take place in a virtual classroom with students wearing VR headsets and logging in from different locations.
Conclusion
Virtual Reality (VR) is revolutionizing the world around us, the use of VR in oncology is today a practice that is increasingly considered by healthcare teams, it is highly interactive, flexible, tailored to the individual, and applicable to people of different ages, genders, and health. As technology improves and costs are reduced, virtual reality will undoubtedly shape the future of cancer care.
References
- (2005) Medling uses of virtual reality in healthcare: it's almost done. Biomed Instrum Technol 39: 16-18.
- Riener R, Harders M (2012) Virtual reality in medicine. Springer, London, UK, pp: 1-2.
- Helfand M, Freeman M (2009) Assessment and management of acute pain in hospitalized adult patients: a systematic review. Pain Medicine 10(7): 1183-1199.
- Turk DC, Wilson HD, Cahana A (2011) Treatment of chronic non-cancer pain. Lancet 377(9784): 2226-2235.
- Shah A, Hayes CJ, Martin BC (2017) Factors influencing long-term opioid use among opioid-naïve patients: a review of initial prescribing characteristics and etiologies of pain. Journal of Pain 18(11): 1374-1383.
- Dascal J, Reid M, IsHak WW, Spiegel B, Recacho J, et al. (2017) Virtual reality and medical inpatients: a systematic review of randomized controlled trials. Innov Clin Neurosci 14(1-2): 14-21.
- Bin S, Masood S, Jung Y (2020) Virtual and augmented reality in medicine. In: Feng DD (Ed.), Biomedical Information Technology. (2nd edn), Academic press, USA, pp: 673-686.
- Khor WS, Baker B, Amin K, Chan A, Patel K, et al. (2016) Augmented and virtual reality in surgery-the digital surgical environment: applications, limits and legal pitfalls. Anne Trad Med 4(23): 454.
- Chirico A, Lucidi F, Laurentiis M, Milanese C, Napoli A, et al. (2016) Virtual reality in health system: beyond entertainment. A mini review on the efficacity of VR during cancer treatment. J Cell Physiol 231(2): 275-287.
© 2022 Sakhri Selma Épse Boulhart. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






