- Submissions

Full Text
Gerontology & Geriatrics studies
Exploring the Relationship between the Platelet Indices and Psychosocial Morbidity in Elderly Patients at a Rural Medical College Hospital
Sunil Kumar*, Abhijit Agrawal, Jahanvi Bhagwati and Sachin Agrawal
Jawahar Lal Nehru Medical College, Datta Meghe Institute of Medical Sciences (DU), Wardha, Maharashtra, India
*Corresponding author: ISunil Kumar, MD, PGDGM (Geriatric medicine), Professor and Head, Department of Medicine, Jawahar Lal Nehru Medical College, Meghe Institute of Medical Sciences (DU), Wardha, Maharashtra, India
Submission: March 05, 2018;Published: May 07, 2018

ISSN : 2578-0093Volume3 Issue2
Abstract
Background: The platelet indices like mean platelet volume (MPV), platelet distribution width (PDW), and plateletcrit (PCT) are a laboratory marker associated with platelet function and activity. We have tried to correlate and compare all these indices in elderly patients as far as psychosocial morbidity like cognition, frailty and depression are concerned.
Methods: This was a prospective observational study and it comprised 1000 consecutive elderly patients admitted for routine check-up in medicine department. Blood samples were taken to measure platelet indices like MPV, PDW and PCT. Cognition, frailty and depression were assessed by the Mini mental state examination, frail non disabled questionnaire and Geriatric Depression scale respectively.
Result: Patients with normal and high platelet count had a depression score of more than 5. [(p=0.0001, r=0.705) 2=811.21, p=0.0031,S]. In the group of low platelet count, 50.58% patients were robust, 49.42% patients were frail (r=0.792, p=0.0001). Among normal platelet count group, 92.75% were frail (r=0.337, p=0.0001). In high platelet count group, 13.40% were robust, 71.30% frail and 15.30% were disable (r=0.781, x2=652.91; p<0.0001, S). In high platelet count group 81.01% had MMSE score ≤23, (r=-0.440, x2=754.72, p=0.0001, S). 79.25% patients having high PCT had MMSE score ≤23, (r=-0.528, x2=737.28, p=0.0001, S).
Conclusion: Platelet indices could be considered meaningful laboratory markers for the risk of psychosocial morbidity in elderly people.
Keywords: Elderly; Psychosocial; Morbidity; Platelet indices
Introduction
Ageing is a normal, progressive and irreversible process which affects every individual, family, community and society. Government of India under National Policy on Older Persons has defined ‘senior citizen’ or ‘elderly’ as a person who is of age 60 years or above in 1999. In our country total population of elderly is 10 crore, forming 10% of total population and it is estimated to reach up to 15crore by 2020 [1]. Among them at least 50% have chronic diseases thus posing a greater responsibility on the health services where there is a greater strain on available health infrastructure and financial constraints [2]. Aging is a process of deterioration in the functional capacity of an individual that results from structural changes, with advancement of age leading to an increased risk of functional dependence, hospitalization, and mortality [3-5].
Therefore, many recent studies have investigated the usefulness of various parameters of automated blood cell counters as biomarkers for adverse clinical outcomes in the elderly. Among them is total leucocytes and some subpopulations of leucocytes which is associated with frailty, red blood cell distribution width seems to be a good indicator of morbidity, and mean platelet volume as markers for cardiovascular disease and its risk factors like hypertension and diabetes [6-12]. The platelet indices like mean platelet volume (MPV), platelet distribution width (PDW), and plateletcrit (PCT) values exhibited significant variability. There is evidence that Depression is associated with platelet activation, it also became apparent that the selective serotonin reuptake inhibitor (SSRIs) in general and sertraline in particular affect platelet function. SSRIs block reuptake of serotonin not only in nerve cells but also in platelets as well [13,14].
Common psychosocial problems include impaired memory and intelligence, anxiety, depression, frailty, dependency and dissatisfaction with family members, earning and occupation. There is limited knowledge of the usefulness of platelet indices as markers for psychosocial morbidity like depression, frailty, and cognition in the elderly. Research is needed to identify risk factors at a stage of age-related decline that would be amenable to preventive interventions. To address this issue, we have tried to analyse the association of the following platelet indices as Platelet count (PLT), platelet distribution width (PDW), MPV, and platelet crit with psychosocial morbidity as a potential biomarkers.
Material and Method
This prospective observational study was conducted in rural medical hospital at Wardha city, the state of Maharashtra from August 2016 to July 2017. All consecutive patients above the age of 60 years admitted in our hospital were enrolled for the study, after taking approval from the institutional ethics committee. In our hospital there is Adhar scheme which provides free of cost screening and treatment for the patients having average daily admission of 15 to 20 patients, being most of them elderly. We have enrolled 1200 elderly patients under this scheme who has come for routine checkup. Patients having malignant disease, infection, h/o blood transfusion, myeloproliferative disorder, h/o recent major surgery, h/o intake of anti-platelet drugs, h/o chemotherapy/radiotherapy and critically ill were excluded from the study. Total 200 patients were excluded from the study and 1000 were enrolled (Figure 1).
Figure 1: Scatter diagram showing linear correlation between platelet count and depression score.

Review was done regarding subject’s medical and pharmacological history, a physical examination, and a physical activity questionnaire. The disease status of the patient was based on the explicit diagnosis in the patient’s medical history. Patient’s physical activity and daily life were evaluated on the basis of their frailty index. The diagnosis of dementia and cognitive impairment was based on MMSE and the criteria of the diagnostic and statistical manual of the mental disorder. Each participant’s relatives were provided with information about the purpose and objective of the study and signed informed consent. The Geriatric Depression scale was used to assess the probable depression in our study group. A score of ≥5 on geriatric depression scale was suggestive of probable depression.
The frailty score (FIND-frail non disabled questionnaire) was used for diagnosing the frailty. A patient with score a+b=1 was labelled “ROBUST”, a patient with score c+d+e=1 was labelled “FRAIL” and patient with a score a+b+c+d+e=0 was labelled as “DISABLED”. MMSE (mini mental state examination) questionnaire was used for diagnosing cognitive impairment. A score of ≤23 was suggestive of cognitive impairment.
Blood collection
Blood samples were obtained by venupuncture for biochemical analysis. Following platelet indices had been measured using automated hematology analyzer in the central laboratory of the hospital-platelet count, mean platelet volume and platelet distribution width and platelet crit.
Definitions:
A. Platelet count: Total number of platelets (1.5lac/cu mm to 5.0lac/cu mm).
B. Plateletcrit: It is a measure of total platelet mass (0.150 to 0.500%).
C. Mean platelet volume: It is the average size of platelets (6.0 to 11.0/cu micrometer).
D. Platelet distribution width: It is the variability in the size of the smallest and the largest platelets (11.0 to 18.0%).
Statistical analysis
Statistical analysis was done by using descriptive and inferential statistics using Chisquare test, Pearsons’ correlation coefficient and software used in the analysis were SPSS 20.0 version, Graph Pad Prism 6.0 version and p<0.05 is considered as level of significance.
Result and Observation
In this study we included 1000 patients of whom 601(60.1%) were males and 399(39.9%) were females, mean age was 66.02±5.76years. The mean platelet count was 303210±21296lac/ cu mm, the mean platelet crit 0.29±0.17%, mean platelet volume was 9.25±5.70 per μm3, and the mean platelet distribution width 14.18±5.63%. There were 165 males who were chronic smokers and 107 males who were chronic alcoholics.
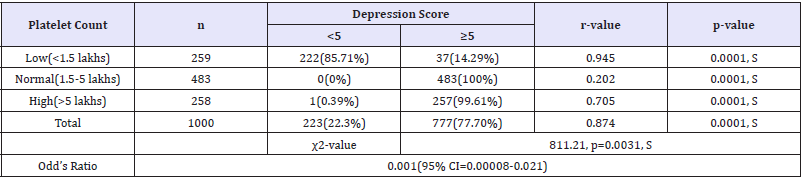
In our study of 1000 patients, 259 patients had platelet count less than 1.5lac/cu mm of which 222(85.71%) patients had a depression score of less than 5 and 37(14.29%) patients had a depression score of more than 5(p=0.0001, r=0.945). 483 patients with normal platelet count had a depression score more than 5, (p=0.0001, r=0.202). Out of 258 patients 257(99.61%) patients had a depression score of more than 5, which was statistically significant [(p=0.0001, r=0.705)2=811.21, p=0.0031, S]. The correlation of platelet count with Depression score is shown in Figure 1 and Table 1.
Table 1: Correlation of platelet count with depression score.
In lower platelet count group, 131(50.58%) patients were in robust category according to frailty score , 128(49.42%) frail and 0% were disable, having positive correlation between platelet count and frailty score (r=0.792 and p=0.0001). In patients having normal platelet 3(0.62%) were robust, 448(92.75%) were frail and 32(6.63%) were disable, (r=0.337, p=0.0001). Among higher platelet count group, 134(13.40%) patients were robust, 713 (71.30%) were frail and 153(15.30%) were disable, (r=0.781, 2=652.91; p<0.0001, S). The Correlation of platelet count with Frailty score is shown in Figure 2 and Table 2.
Figure 2: Scatter diagram showing linear correlation between platelet count and frailty score.
Table 2: Correlation of platelet count with Frailty score.
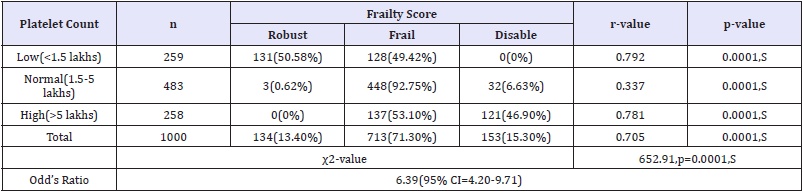
Table 3: Correlation of platelet count with MMSE score.
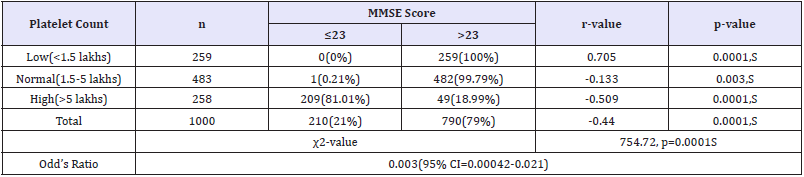
In our study in 259 patients with low platelet counts, none had MMSE score ≤23, (r=0.705, p=0.0001). Among patients with normal platelet count only 1(0.21%) patient had MMSE score ≤23 and 482(99.79%) patients had MMSE score >23, (r=-0.133). In patients with high platelet count 209(81.01%) had MMSE score ≤23 while 49(18.99%) patients had MMSE score >23, (r=-0.509, p=0.0001). Altogether platelet count was negatively correlated with MMSE score (r=-0.440) and it was statistically significant (2=754.72, p=0.0001S) (Table 3).
Among 294 patients with low platelet crit, 222(75.51%) patients had depression score <5 and 72(24.49%) patients had depression score ≥5, (r=0.884, p=0.0001). All patients with normal platelet crit had depression score ≥5, (r=0.061, p=0.200). 265 patients had high platelet crit, of these 1(0.38%) patient had depression score <5 and 264(99.62%) patients had depression score ≥5, (r=0.696, p=0.0001). Altogether platelet crit showed positive correlation with depression score [(r=0.831, 2=680.48; p<0.0001, S)], shown in Figure 3 and Table 4.
Figure 3: Scatter diagram showing linear correlation between platelet crit and depression score.
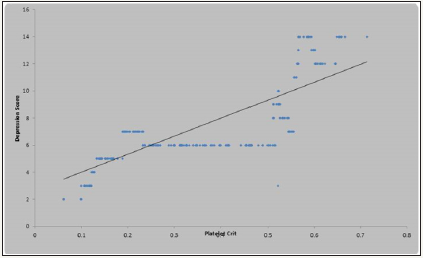
Table 4: Correlation of platelet crit with depression score.
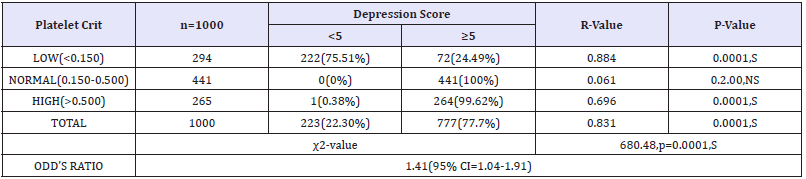
Figure 4: Scatter diagram showing linear correlation between platelet crit and frailty.

Table 5: Correlation of platelet crit with frailty score

Out of 294 patients who had low platelet crit, 131(44.56%) were robust, 163(55.44%) patients were frail and non were disable, (r=0.651, p=0.0001). Patients with normal platelet crit (441), 3(0.68%) patients were robust, 412(93.42%) patients were frail and 26(5.90%) patients were disable, (r=0.279, p=0.0001). Patients with high platelet crit (265), non were robust, 138(52.08%) patients were frail and 127(47.92%) patients were disable, [(r=0.710, p= 0.0001) (2=610.95; p<0.0001 S-Significant)]. The Correlation of platelet crit with Frailty score is shown in Figure 4 and Table 5.
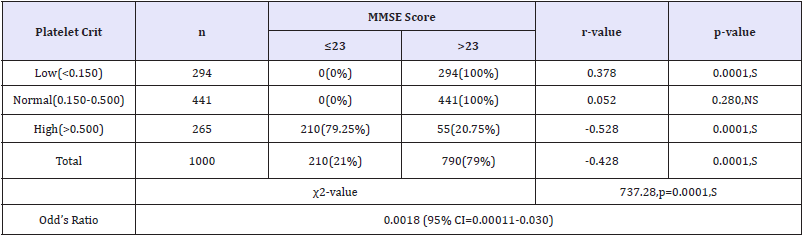
In our study 294 patients had platelet crit below 0.150, of them none had MMSE score ≤23, (r=0.378, 0.0001). In normal platelet crit group, none-had MMSE score ≤23, (r=0.052, p=0.280). 265 patients had high platelet crit (>0.150), among them 210(79.25%) had MMSE score ≤23 and 55(20.75%) had MMSE score >23, (r=- 0.528, p=0.0001), [2=737.28, p=0.0001, S]. The Correlation of platelet crit with MMSE score is shown in Figure 5 and Table 6.
Figure 5: Scatter diagram showing linear correlation between platelet crit and MMSE score.
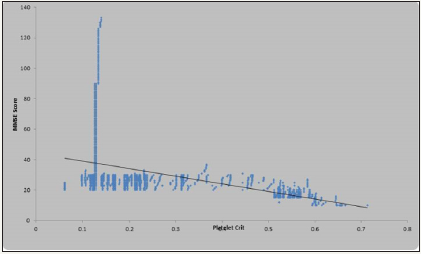
Table 6: Correlation of platelet crit with MMSE score.
In 259 patients with PDW <11%, 222(85.71%) had depression score <5 and 37(14.29%) had depression score ≥5, (r=0.945, p=0.0001). 481 patients had normal PDW (11 to 18%), of them all had depression score ≥5, (r=0.219, p=0.0001). In high PDW (18%) group, out of 260 1(0.38%) patient had depression score <5 and 259(99.62%) patients had depression score ≥5, [(r=0.743, p=0.0001) (2=811.21; p<0.0001 S]. The Correlation of platelet distribution width with Depression score is shown in Figure 6 and Table 7.
Figure 6: Scatter diagram showing linear correlation between platelet distribution width and depression score.
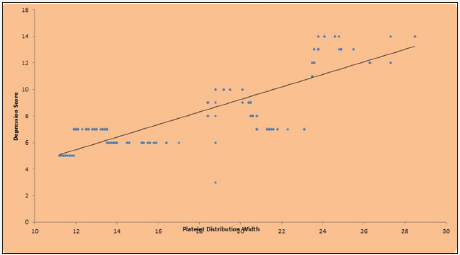
Table 7: Correlation of platelet distribution width with depression score.
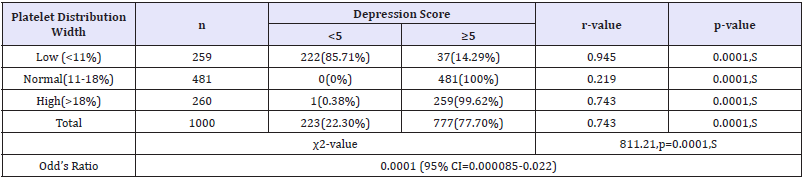
Figure 7: Scatter diagram showing linear correlation between platelet distribution width and frailty score.

Table 8: Correlation of platelet distribution width with frailty score.

According to frailty score 131(50.58%) were robust, 128(49.42%) were frail and none were disable in low PDW (<11%) group, (r=0.780, p=0.0001). Among 481 patients with normal PDW (11 to 18%) , 3(0.62%) patients were robust, 447(92.93%) were frail and 31(6.44%) were disable, (r=0.283, p=0.0001). 260 patients had high PDW(>18%), non among them were robust, 138(53.08%) patients were frail and 122(46.92%) patients were disable, (r=0.849, p=0.0001), [(2=655.88; p<0.0001S]. The Correlation of platelet distribution width with Frailty score is shown in Figure 7 and Table 8.
Figure 8: Scatter diagram showing linear correlation between platelet distribution width and MMSE score.
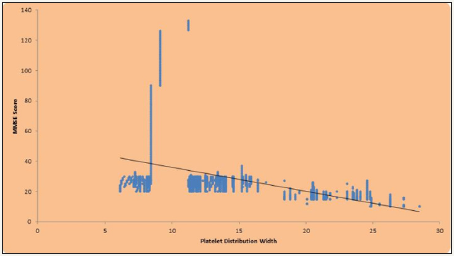
Table 9: Correlation of platelet distribution width with MMSE score.
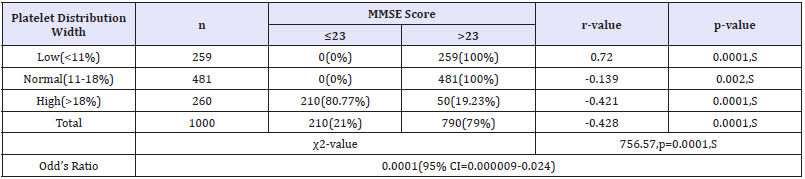
In low PDW group (<11%) all had MMSE score >23, (r=0.720, p=0.0001). 481 patients with normal PDW (11 to 18 %), all had MMSE score > 23, (r=-0.139, p=0.002). In high PDW group (260), 210(80.77%) patient had MMSE score ≤23 and 50(19.23%) patients had MMSE score >23, (r=-0.421, P=0.0001). Altogether 210(21%) patients showed MMSE score ≤23 and 790(79%) patient had MMSE score >23, [(r=-0.428, 2=756.57; p=0.0001)] Figure 8 and Table 9.
Figure 9: Scatter diagram showing linear correlation between mean platelet volume and Depression score.
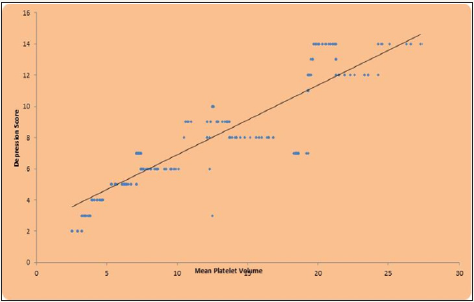
Table 10: Correlation of mean platelet volume width with depression score.
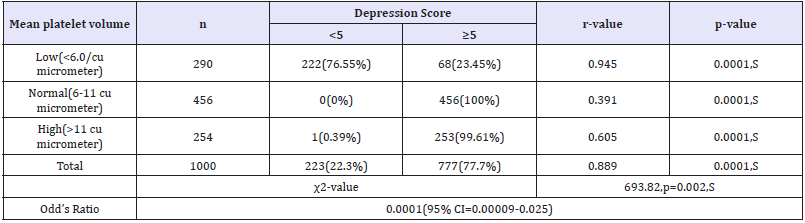
Out of 290 patients with low MPV (<6.0/cu μm), 222(76.55%) had depression score <5 and 68(23.45%) patients had depression score ≥5, (r=0.945, p=0.0001). All 456 patients with MPV (6.0 to 11.0/cu μm) had depression score≥5, (r=0.391, p=0.0001). 254 patients had high MPV (>11/cu μm), among them 253(99.61%) patients had depression score ≥5, (r=0.605, p=0.0001). Out of 1000 patients 223(22.3%) patients had depression score < 5 and 777(77.7%) patients had depression score ≥5, [(r=0.889, p=0.002, (2=693.82; p<0.0001, S]. The correlation of mean platelet volume with depression score is shown in Figure 9 and Table 10.
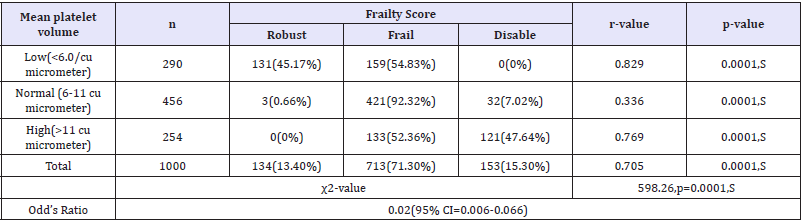
In 290 patients with low MPV (< 6.0/cu μm), 131(45.17%) were robust, 159(54.83%) were frail and none were disable, (r= 0.829, 0.0001). Among 456 patients with normal MPV (6 to 11/cu μm), 3(0.66%) were robust, 421(92.32%) were frail and 32(7.02%) were disable, (r=0.336, p=0.0001). Among 254 patients having high MPV (>11/cu μm), none were robust, 133(52.36%) were frail and 121(47.64%) were disable, (r=0.769, p=0.0001). Of 1000 patients 134(13.40%) were robust, 712(71.30%) frail and 153(15.30%) were disable, [(r=0.705, p=0.0001) (2=598.26; p<0.0001 S] (Figure 10) (Table 11).
Figure 10: Scatter diagram showing linear correlation between mean platelet volume and frailty score.
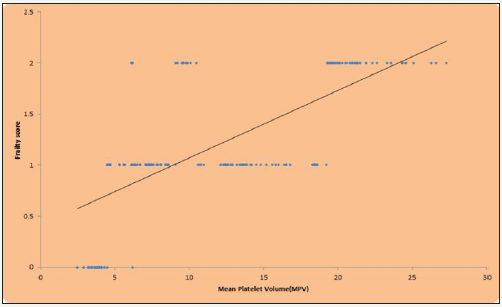
Table 11: Correlation of mean platelet volume width with frailty score.
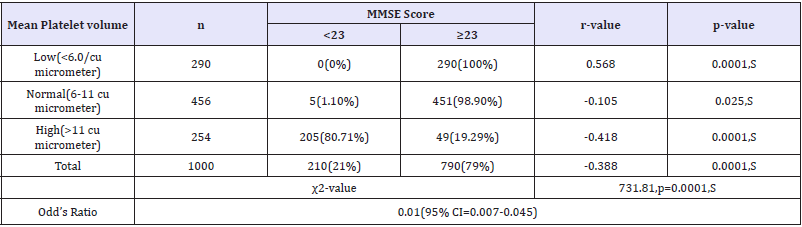
In all patients (290) with low MPV (<6.0/cu μm), MMSE score was >23, (r=0.568, p=0.0001). 451(98.90%) patients with normal MPV had MMSE score >23, (r=-0.105, p=0.025). Among 254 patients with high MPV, 205(80.71%) had MMSE score ≤23 and 49(19.29%) had MMSE score >23, (r=-0.418, p=0.0001).
Discussion
We have found significant association of the Platelet indices like Platelet count (PLT), platelet distribution width (PDW), MPV, and plateletelcrit (PCT) with psychosocial morbidity like depression, frailty and cognition in elderly subjects. In this study almost all patients with normal (100%) and high (99.6%) platelet count had a depression score of more than 5. [(p=0.0001, r=0.705) 2=811.21,p=0.0031,S]. In a study by Morel et al. [15] similar results was found as the patients with higher platelet count showed more depression, (they used the Montgomery As berg depression rating scale), while in our study geriatric depression scale were taken [15]. The mean age in Morel et al was 42.94±9.99 years. A possible explanation in this context is that depression overlaps with anxiety and panic attack which could lead to sympathetic overdrive; a platelet would respond to adrenalin or noradrenalin released after such stress [15]. In normal platelet count cause of depression is unexplained.
In the group of low platelet count, 50.58% patients were in robust category according to frailty score, 49.42% patients were frail and none were disable, having positive correlation between platelet count and frailty score (r=0.792, p=0.0001). Among normal platelet count group, 92.75% were frail having positive correlation between platelet count and frailty score (r=0.337, p=0.0001). In high platelet count group, 13.40% were robust, 71.30% frail and 15.30% were disable. There was a positive correlation between platelet count and frailty score (r=0.781, 2=652.91; p<0.0001 S).In contrast to our study, Amira A Mahmoud et al. [16] showed non-significant correlation with platelet count and frailty in the age group of 19-70 years (mean age 48.09±18. 3). Phenotypes of frailty used in their study were Cardiovascular health study, and Centre for Epidemiological Studies-Depression. In our study we used FIND questionnaire. In their study 34 (24.2%) patients were robust with mean platelet count of 154.9±42, 22 (15.8%) were prefrail with mean platelet count of 145.7±71.7 and 84(60%) were frail with mean platelet count of 177.4±70.4, which was not significant (p=0.21). In our study patients with low platelet counts, none had MMSE score ≤23, while in high platelet count group 81.01% had MMSE score ≤23,(r=-0.440, 2=754.72, p=0.0001, S). No previous study was available for comparison between low platelet count and MMSE score (Table 12).
Table 12: Correlation of mean platelet volume width with MMSE score.
When compared with PCT, almost all patients with normal and high PCT had depression score ≥5. Altogether PCT showed positive correlation with depression score (r=0.831) and it was statistically significant (p=0.0001) [2=680.48; p<0.0001]. No previous studies showed relation of PCT with depression. In our study patients who had low PCT, 131(44.56%) were robust, 163(55.44%) were frail and none were disable. Patients with normal PCT almost all 93.42% were frail and Patients with high PCT, none were robust, 138(52.08%) were frail and 127(47.92%) were disable, (2=610.95; p<0.0001). There was no previous study correlating PCT with frailty. In our study there were 79.25% patients having high PCT had MMSE score ≤23, (r=-0.528, 2=737.28, p=0.0001, S). No separate data for PCT and MMSE score were available. In our study 37/259(14.29%) patients with low PDW had depression score ≥5, (r=0.945,p=0.0001). While almost all patients with normal and high PDW had depression score ≥5, (r=0.743, 2=811.21; p<0.0001 S). No study was available to compare PDW with depression.
In our study patients with low PDW, 131/259 (50.58%) were robust, 128/259 (49.42%) were frail and none were disable. There was a positive correlation between PDW and frailty score (r=0.780) and it was statistically significant (p=0.0001). With normal PDW 447/481(92.93%) patients were frail and 31/481 (6.44%) were disable, (r=0.283, p=0.0001). In high PDW group, 138/260 (53.08%) patients were frail and 122/260 (46.92%) were disable, (2=655.88;p<0.0001 S). There was no study of frailty with PDW. In our study when correlated with PDW, 210/260 (80.77%) patients with high PDW had MMSE score ≤23 and 50/260 (19.23%) had MMSE score >23. Similar correlation was also found by Wang et al. [17] and Liang QC et al. [18] where they got a positive correlation between Mini-Mental State Examination (MMSE) and MPV and PDW, after adjusting confounding factors (r =0.532 for MPV and r=0.425 for PDW, p<0.001 for both).
In our study patients having low MPV, 68(23.45%) patients had depression score ≥5 and almost all had depression score ≥5, in normal and high MPV group. Out of 1000 patients 223(22.3%) patients had depression score <5 and 777(77.7%) patients had depression score ≥5, MPV was positively correlated with depression score (r=0.889) and it was statistically significant (p=0.002) (2=693.82; p<0.0001 S-Significant). Similar results were seen in a study by Ataoglu et al. [19]. In this study out of 1000 patients 134(13.40%) patients were robust, 712(71.30%) patients were frail and 153(15.30%) patients were disable, there was a positive correlation between MPV and frailty score (r=0.705) and it was statistically significant (p=0.0001) (2=598.26;p<0.0001 S-Significant). There was no data of frailty with MPV. In our study out of 1000 patients 210(21%) patients had MMSE score ≤23 and 790(79%) patients had MMSE score >23. (r=0.388, 2=731.81; p=0.0001 S). Similar to our study Wang et al. [17] and Liang QC et al. [18] also compared MPV and PDW with MMSE score, and they showed significant correlation.
Conclusion
Elderly population are more prone to various psychological, physical and cognitive impairment hence our study provides evidence that platelet indices can be used as a potential biomarker to ascertain probable depression, frailty and cognitive function in elderly population. However more research are required on this topic to generalise in community.
Ethics Committee Approval
This study was approved by the ethical committee under the terms of the favourable approval by the Data Meghe institute of medical sciences (deemed to be university)[IEC reference number- DMIMS (DU)/IEC/2015-16/1489).
References
- Central S Office (2011) Situation analysis of the elderly in India.
- Yeolekar ME (2005) Elderly in India-needs and issues. J Assoc Physician India 53: 843-844.
- Kumar V (2012) Geriatric medicine. In: Munjal YP (Ed.), API Textbook of Medicine, (9th edn), Jaypee Brothers Medical Publishers (P) Ltd., New Delhi, India, pp. 2038-2042.
- Ahmed N, Mandel R, Fain MJ (2007) Frailty: an emerging geriatric syndrome. Am J Med 120(9): 748-753.
- Sunil K (2017) Frailty index-assessment tools in elderly: feasibility in India. Annals of Geriatric Education and Medical Sciences 4(2): 45-49.
- Leng SX, Hung W, Cappola AR, Yu Q, Xue QL, et al. (2009) White blood cell counts, Insulin like growth factor-1 levels, and frailty in communitydwelling older women. J Gerontol A BiolSci Med Sci 64(4): 499-502.
- Patel KV, Semba RD, Ferrucci L, Newman AB, Fried LP, et al. (2010) Red cell distribution width and mortality in older adults: a meta-analysis. J Gerontol A BiolSci Med Sci 65(3): 258-265.
- Endler G, Klimesch A, Sunder-Plassmann H, Schillinger M, Exner M, et al. (2002) Mean platelet volume is an independent risk factor for myocardial infarction but not for coronary artery disease. Br J Haematol 117(2): 399-404.
- Chu SG, Becker RC, Berger PB, Bhatt DL, Eikelboom JW, et al. (2010) Mean platelet volume as a predictor of cardiovascular risk: a systematic review and meta-analysis. J Thromb Haemost 8(1): 148-156.
- Leal-Santos FA, Silva SB, Crepaldi NP, Nery AF, Martin TO, et al. (2013) Altered platelet indices as potential markers of severe and complicated malaria caused by Plasmodium vivax: a cross-sectional descriptive study. Malar J 12(1): 462.
- Pathansali R, Smith NM, Bath PMW (2001) Prothrombotic megakaryocyte and platelet changes in hypertension are reversed following treatment: a pilot study. Platelets 12(3):144-149.
- Greisenegger S, Endler G, Hsieh K, Tentschert S, Mannhalter C, et al. (2004) Is elevated mean platelet volume associated with a worse outcome in patients with acute ischemic cerebrovascular events? Stroke 35(7): 1688-1691.
- Parakh K, Sakhuja A, Bhat U, Ziegelstein RC (2008) Platelet function in patients with depression. South Med J 101: 612-617.
- Markovitz JH, Shuster JL, Chitwood WS, May RS, Tolbert LC (2000) Platelet activation in depression and effects of sertraline treatment: An open-label study. Am J Psychiatry 157(6): 1006-1008.
- Morel-Kopp MC, Mclean L, Chen Q, Tofler GH, Tennant C, et al. (2009) The association of depression with platelet activation: evidence for a treatment effect. J Thromb Haemost 7(4): 573-581.
- Mahmoud AA, Fouad M, Deraz H (201) Prevalence and Correlates of Frailty among Patients on Maintenance Hemodialysis. Gen Med 3: 156.
- Wang R, Jin D, Li Y, Liang Q (2013) Decreased mean platelet volume and platelet distribution width are associated with mild cognitive impairment and Alzheimer’s disease. J Psychiatr Res 47(5): 644-649.
- Liang QC, Jin D, Li Y, Wang RT (2014) Mean platelet volume and platelet distribution width in vascular dementia and Alzheimer’s disease. Platelets 25(6): 433-438.
- Ataoglu A, Canan F (2009) Mean platelet volume in patients with major depression: effect of escitalopram treatment. J Clin Psychopharmacol 29(4): 368-371.
© 2018 Sunil Kumar. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






