- Submissions

Full Text
Experimental Techniques in Urology & Nephrology
Paraganglioma of the Urinary Bladder - A Rare Tumor
Rathee VS*
Department of Surgery and Urology, India
*Corresponding author: Rathee VS, Department of Surgery and Urology, PGIMS, Rohtak, India
Submission: February 12, 2020;Published: March 04, 2020

ISSN 2578-0395Volume3 Issue1
Introduction
Approximately 10% of the tumors from chromaffin cells occur at extra adrenal sites [1]. Extra adrenal pheochromocytomas are known as paragangliomas. Primary paraganglioma of the urinary bladder is rare making up less than 0.05% of all bladder neoplasms [2]. It has been postulated that bladder paragangliomas arise from Embryonic rests of chromaffin cells within the bladder wall. They are commonly situated at the dome or the trigone of the bladder [2,3]. The most common symptoms are paroxysmal hypertension headache, sweating and palpitation [4]. The other symptoms commonly reported is haematuria (50-60%) [5], though this is not specific for paraganglioma.
Material and Methods
We report a 32 years female presented with total painless gross haematuria for 2 months duration. Physical examination was normal. Cystoscopy showed a solid tumor (2x2cm) on the posterior wall of the bladder (Figure 1).
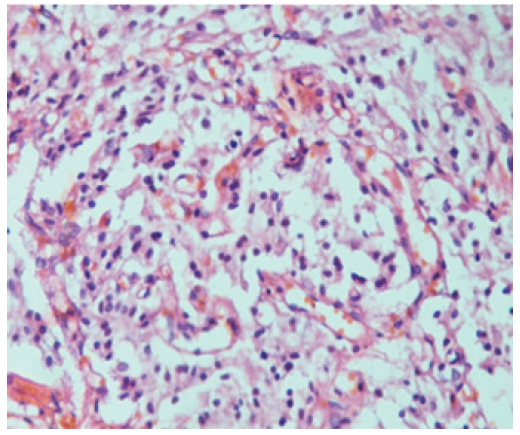
Figure 1: Photomicrograph showing zellballen arrangement of tumor cells with abundant clear cytoplasm, characteristic of paraganglioma (H&E stain, 400x).
Result
I. TURBT (Transurethral resection of bladder tumor) was done Operative findings were as follows: 2x2 cm solid tumor on the posterior wall of the urinary bladder. RUOnormal, LUO not visualized. Complete resection of the tumor done.
II. Histopathological report of the biopsy specimen showed neuroendocrine cells with some typical zellballen appearance (Figure 1).
III. Staining was strongly positive for chromogamin and S-100. Post- operative period was uneventful.
Conclusion
I. Paraganglioma of the urinary bladder is a rare tumor. Approximately 10% of the bladder paragangliomas are malignant with one or more local invasion, regional lymph node metastasis or distant spread.
II. Clues to early diagnosis may perhaps include a characteristic Cystoscopic appearance though this has not been specifically, Investigated in the literature to date.
III. Due to low prevalence of these tumors this is something that will likely rely on further assessment of case reports in the future to establish.
References
- Das S, Bulusu NV, Lowe P (1983) Primary vesical pheochromocytoma. Urology 21(1): 20-25.
- Dahm P, Gschwend JE (2003) Malignant non-urothelial neoplasms of the urinary bladder: A review. European Urology 44(6): 672-681.
- Ansari MS, Goel A, Goel S, Durairajan LN, Seth A (2001) Malignant paraganglioma of the urinary bladder- A case report. International Urology and Nephrology 33: 343-345.
- Onishi T, Sakata Y, Yonemura S, Sugimura Y (2003) Pheochromocytoma of the urinary bladder without typical symptoms. Int J Urol 10(7): 398-400.
- Frydenberg M, Ferguson R, Langdon P, Rogers J, McCarthy S (1991) Malignant pheochromocytoma of the bladder active or inactive. Br J Urol 67(5): 548-549.
© 2020 Rathee VS. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






