- Submissions

Full Text
Experimental Techniques in Urology & Nephrology
Ureterocalicostomy for Upper Ureteric Injury: Measure to Salvage the Renal Unit
Aman Gupta1, Vidur Bhalla2 and Vivek Kumar Garg3*
1Senior Resident, Department of Urology, GMCH, India
2Associate Professor, Department of Urology, GMCH, India
3Demonstrator, Department of Biochemistry, GMCH, India
*Corresponding author: Vivek Kumar Garg, Demonstrator, Department of Biochemistry, GMCH, Chandigarh, India
Submission: January 23, 2020;Published: February 10, 2020

ISSN 2578-0395Volume3 Issue1
Abstract
Ureterocalicostomy is a procedure for recurrent pelvic ureteric junction obstruction (PUJO), inaccessible renal pelvis and renal anomalies associated with PUJO. It requires meticulous dissection of peri pelvic region. A wide spatulated, tension free, mucosa to mucosa anastomosis, internal stenting and lower pole amputation are the key features for a successful outcome of Ureterocalicostomy. We had a patient of upper ureteric injury sustained during laparoscopic converted open adrenalectomy surgery. He also had undergone multiple previous right hypochondrium surgeries that resulted in severe peri pelvic and perinephric fibrosis. Ureterocalicostomy was successfully performed in the patient. We hereby emphasize the possibility of Ureterocalicostomy as a procedure of choice in a case of iatrogenic ureteric injury and inaccessible pelvis due to severe peri pelvic adhesions.
Keywords: Ureterocalicostomy; PUJ obstruction; Upper ureteric injury
Introduction
Ureterocalicostomy is a salvage procedure usually performed in patients of recurrent pelvic ureteric junction obstruction (PUJO) associated with inaccessible renal pelvis due to peri pelvic fibrosis around upper ureter. Ureterocalicostomy is also considered a primary procedure of choice in some patients of PUJ obstruction associated with renal anomalies. Here, we present a case of iatrogenic ureteric injury with loss of upper ureteric segment sustained during a difficult laparoscopic converted open adrenalectomy treated with Ureterocalicostomy.
Case report
A forty-four-year-old male presented to our department in September 2018, three weeks after undergoing laparoscopic converted open right adrenalectomy for incidentaloma. This patient had significant history of multiple previous right hypochondrial interventions. He had sustained blunt trauma abdomen with liver injury due to roadside accident in 1997 which was managed conservatively. Thereafter, in November 2014 he underwent Endoscopic retrograde cholangiopancreatography (ERCP) for biliary sludge. During that procedure of ERCP, dormie basket got stuck in the CBD requiring a conversion to open cholecystectomy and CBD exploration with T- tube drainage. In 2005, patient developed common bile duct stricture and underwent multiple CBD stents placed which were kept in situ for 5-6 years and then removed. Patient was in regular follow up for his hepatobiliary problem.
In 2014 patient was detected with right adrenal incidentaloma which was kept under observation. Due to increasing size of the incidentaloma (9x9.3x9.4), he was planned for adrenal surgery on 27/8/18. Laparoscopic adrenalectomy was planned and started but because of dense adhesions noted intraoperatively surgery was converted into open procedure through right subcostal incision. Patient was discharged on post-operative day 6. Histopathology report of the specimen was myelolipoma of adrenal gland. After three weeks, patient reported back to the primary surgeon with fever. Ultrasound showed a collection of 11.8x8.9 cm along lower pole of right kidney. Percutaneous pigtail drainage with 10f was done. Its drained pus initially for 3days and then clear urine. The drainage continued for many days. CECT scan identified a small rent in posterior part of right renal pelvis with associated urinoma formation in right para renal space, extending up to right parabolic gutter. Right DJ stenting was done.
Figure 1: Combined RGP and nephrostogram showing a gap of approximately 2.5cm between renal pelvis and upper ureter.
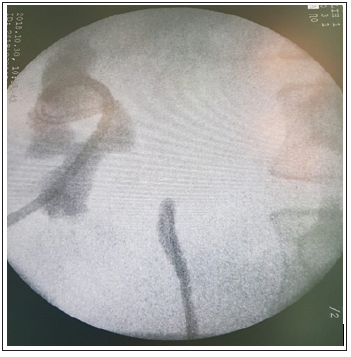
Figure 2: Intraoperative picture showing complete transection of the ureter at the upper end.

At this stage patient was referred to our department. Xray abdomen KUB showed malpositioned DJ stent. Thus, DJ stent was removed. RGP was also performed which showed complete ureteric obstruction at upper level. Ultrasound guided right PCN was done. Later a combined RGP and nephrostogram was performed which showed a gap of approximately 2.5cm between renal pelvis and upper border of ureter (Figure 1). Patient was planned for exploration with options of pyeloplasty and Ureterocalicostomy. Consent for nephrectomy was also taken anticipating dense adhesions because of his previous procedures. Patient was explored on 2/11/18 through previous scar excising right subcostal incision. Ascending colon was mobilized, and ureter was identified, traced and dissected up to the blind end of upper ureter (Figure 2). On medial aspect dense adhesions were present between kidney, pelvis and IVC and renal pelvis was found out to be completely frozen. Vascular control for kidney was also not possible as hilum could not reach.
There were tough adhesions between kidney, liver and with other surrounding structures making kidney mobilization difficult. Pus pocket posterior to kidney was drained. With blunt and sharp dissections lower pole of the kidney was mobilized. PCN was removed and through that tract a bougie was passed into the lower calyx for identification and over its lower pole of the kidney was amputated. Parenchyma of the lower pole was quite thick and vascular, so hemostasis achieved. Ureter was spatulated and was anastomosed with the calyx over DJ stent. Anastomosis was watertight and tension free (Figure 3). Post-operative events were not significant and pcn was removed on POD 13. Drain was removed on POD17. Patient was discharged with stable vitals, wound healthy, self-voiding and orally accepting well. Patient was kept on follow up and DJ stent was changed at fourth month.
Figure 3: Anastomosis of transected lower pole of the kidney with ureter.

Discussion
Neuwist K [1] first described Ureterocalicostomy in 1947 and it was technically modified by Hawthorne et al. [2]. Ureterocalicostomy has been accepted as a salvage procedure for recurrent PUJO and also as a primary surgery for complex ureteropelvic junction strictures as reported by Kochakaran et al. [3]. It is to be considered in patients where standard pyeloplasty cannot be used [4-8] i.e.
1. PUJ obstruction with renal anomalies of fusion/rotation/ ascent. 2. Intrarenal pelvis or short ureter 3. Previous failed pyeloplasty. 4. Extensive post-operative fibrosis. 5. Reconstruction associated with trauma. 1. Contraindication for Ureterocalicostomy includes: 1. Poorly functioning kidney with MAG3 clearance <20%. 2. Infundibular stenosis. 3. Large proximal ureteric stenosis with no possibility of tension free anastomosis. 4. Denuded medial ureter.
Key feature for successful ureterocalicostomy includes:
1. Complete pre-operative evaluation including retrograde pyelography, nephrostogram, intravenous pyelogram or Ct urography. 2. It is important to completely amputate lower kidney pole to avoid anastomotic stricture [9]. 3. Wide tension free [10] anastomosis. 4. Good vascularization of periureteral tissue. 5. Lower 2-3mm calyx should be free of cortex for precise mucosa to mucosa anastomosis [11]. 6. Wrapping of anastomosis with omental pedicled graft [12].
In our case, a 2.5cm segment of upper ureter was missing due to missed intragenic injury during previous surgery. Also, intraoperatively in the present surgery, there were dense peri pelvic adhesions which made the case even more complicated and difficult. In such circumstances Ureterocalicostomy proved to be the best surgical option as it bypassed extensive peri pelvic scarring and inflammation and provided dependent drainage while compensating for insufficient ureteric length.
Conclusion
Ureterocalicostomy, when done, gives good result even in postoperative cases and is a measure to salvage the kidney.
References
- Neuwirt K (1947) Implantation of ureter into lower calyx of renal pelvis. Urol Cutaneous Rev 52(6): 351.
- Hawthorne NJ, Zincke H, Kelalis PP (1976) Ureterocalycostomy: An alternative to nephrectomy. J Urol 115(5): 583-586.
- Kochakaran W, Viseshsindh V, Muangman V (2002) Ureterocalycostomy for reconstruction of complicated UPJ obstruction. J Med Assoc Thai 85(3): 351-355.
- Levitt SB, Nalizadeh I, Javaid M, Ban M, Kegan S et al. (1981) Primary calycoureterostomy for pelviureteral junction obstruction: Indications and results. J Urol 126(3): 382-386.
- Wesolowski S (1971) Corrective operative procedure after unsuccessful pelviureteric plastic surgery. Br J Urol 43: 679-86.
- Jarowenko MV, Flechner SM (1985) Recipient ureterocalycostomy in a renal allograft: Case report of a transplant salvage. J Urol 134(5): 844-855.
- Dewan PA, Clark S, Condron S, Henning P (1999) Point of technique: Ureterocalicostomy in the management of pelviureteral junction obstruction in horse-shoe kidney. Br J Urol 84(3): 366-368.
- Selli C, Rizzo M, Movani F, Dedola G, Amorosi A (1992) Ureterocalicostomy in treatment of pyeloplasty failures. Urol Int 48(3): 274-277.
- Jameson SG, McKinney JS, Rushton JF (1957) Ureterocalycostomy a new surgical procedure for correction of ureteropelvic stricture associated with intrarenal pelvis. J Urol 77(2): 135-43.
- Popescu C (1964) The surgical management of postoperative ureteral fistula. Surg Gynec Obstet 119: 1079-1084.
- Mollard P, Braun P (1980) Primary ureterocalycostomy for severe hydronephrosis in children. J Pediatr Surg 15(1): 87-91.
- Turner WR, Wynne EJ, Handley M (1967) The use of omental pedicle graft in the repair and reconstruction of urinary tract. Br J Surg 54(10): 849-853.
© 2020 Vivek Kumar Garg. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






