- Submissions

Full Text
Experimental Techniques in Urology & Nephrology
Huge Isolated Retrovesical Hydatid Cyst Affecting a Little Girl
Azzawi M Hadi*
Department of surgery, Tikrit medical college, Iraq
*Corresponding author: Azzawi M Hadi, Department of surgery, Tikrit medical college, Iraq
Submission: April 23, 2018;Published: July 03, 2018

ISSN 2578-0395Volume2 Issue2
Abstract:
A 8 year old girl presented with pain abdomen & frequency. Ultrasound & CT scan of abdomen showed hydatid cyst Retrovesical area. Surgery was performed and pathology of the excised mass confirmed the diagnosis. The rarity of the case of primary retrovesical hydatid cyst in such early age and such a huge size was the urging cause to present it.
Keywords: Hydatid cyst; Retrovesical; Echinococcus granulosus
Case Description
A 8-year old girl presented with 4 months abdominal pain which was mild but continues, partially responding to analgesics, she also had frequency and nucturia. not associated with dysuria, nor hematuria. she had no remarkable systemic manifestations, nor a significant evidence in the past medical, and surgical history. she completed her vaccination schedule in time. she born and lives in rural area.
Figure 1:CT scan findings, 7x6cm retrovesical cyst
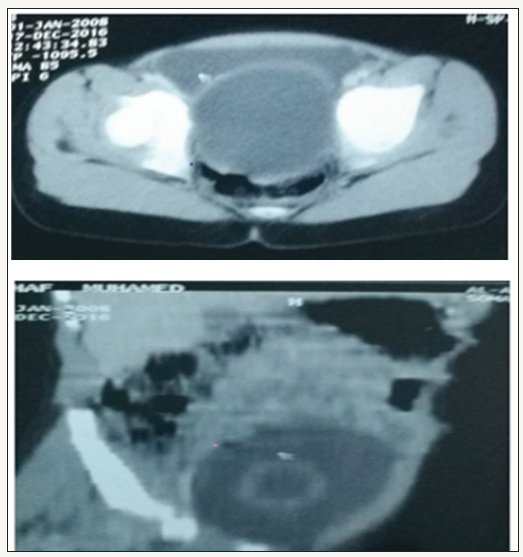
On examination she was very well, and no finding can be detected other than mild lower abdominal tenderness, with palpable soft mass. urinalysis was normal, as well her blood and biochemical indexes. Abdominal ultrasound requested, the report said that she had normal liver abdominal organs, with a cystic mass posterior to the bladder of 7x6cm, which contain echo free fluid, gives a deferential diagnosis of mesenteric cyst, big ovarian cyst, congenital diverticulum. Axial CT scan confirmed these findings as shown in (Figure 1).
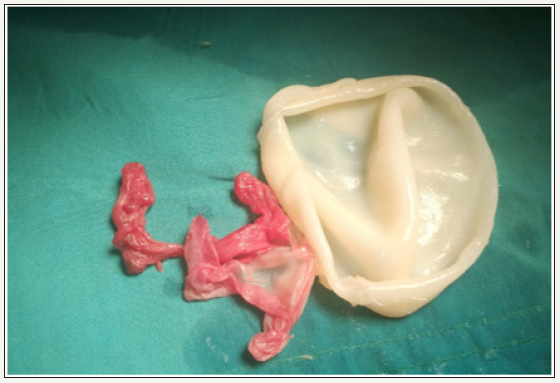
Surgical exploration done by lower abdominal pfannenstiel incision, the mass was in midline, and was located in posterior to the bladder, pushing the posterior bladder wall anteriorly. All other abdominal organs were normal as well the chest views of the CT were normal. Surgery was performed to excise the mass. the cyst contents aspirated, which was clear fluid. and there was an endocyst of hydatid cyst that have been proved by the microscopic examination which revealed a laminated membrane, (Figure 2). Post operatively she had a smooth recovery, and sent home on albendazole tab 200mg daily in two divided doses for 3 months. The girl followed for one year by abdominal ultrasound, that shows no evidence of recurrence.
Figure 2:Part of the pericyst and Endocyst
Discussion
Echinococcus granulosus the parasite that causes hydatid disease is endemic in many areas of the world. Hydatid cysts can develop in almost any part of the body [1]. In most cases, the first and most important locations for this parasite are the liver and the lungs. Hydatid disease of the urinary tract is uncommon, accounting for only 2-3% of all hydatid cases [2]. If hydatid cysts located at some the unusual sites, it may cause a diagnostic uncertainty. Peritoneal cavity hydatid cysts or pelvic hydatid cysts are usually result from rupture of a primary liver focus that occur spontaneously or during surgical management [1]. Although the most common site of echinococcal involvement is the liver, yet cystic echinococcus infestation can occur in any part of the body and should be considered in the differential diagnosis of any cystic masses [3]. Isolated retrovesical hydatid cyst, however, is very rare site with a few cases reported in literature only [4-6]. Unusually retrovesical hydatid cyst can be a cause for retention of urine [7,8]. It can presented as an extraperitoneal cyst, as well in the retrovesical area [9].
The diagnosis is based on clinical findings, imaging techniques and serology. Ultrasound is useful as a first line investigation in evaluation of cysts in the abdomen. Computed tomography and MRI are indicated in disseminated disease, lesions located out of the abdomen, sub-diaphragmatic sites, and pre-operative evaluation [10,11]. Abdominal ultrasound & native CT scan regarded helpful in diagnosis of abdominal hydatid disease and prove the suspicion of the clinical presentation. Although there was a unilocular cyst in our case, the multilocular appearance of the cyst supported by the density of the cyst contents indicated that the cyst was alive & viable [12,13]. Sagittal fast spin-echo T2-weighted MR image clearly identifies small cystic lesions representing daughter cysts [14]. The Dévè’s classical theory states that fissuring or rupture of a primary hepatic, splenic or mesenteric cyst may seed its contents to the abdominal cavity, leading to a new lesions, while the primary cyst may heal and disappear, leaving behind a scar that may not detected by any diagnostic tools [9,11,15]. Haematogenous or lymphatic dissemination is another theory tried to explain the absence of the primary visceral lesion, and the absent evidence of peritoneal seeding [9,11,15]. Other hypothesis said that the larva may remained in the rectal ampulla and migrated through the haemorrhoidal vessels to reach a perirectal or retrovesical location [16].
Surgical treatment of Symptomatic large hydatid cysts by cystopericystectomy still the gold standard procedure [17]. Preoperative and postoperative use of albendazole have been found to decreases the viability of cysts at the time of surgery and significantly reduces the chances of cyst recurrence. Thus, albendazole is regarded as an effective adjuvant therapy in the management of hepatic hydatid cyst [18]. The cyst’s growth rate is of about 10mm per year [19], but it is surprising that the cyst in this case reaches such a size at this age.
Conclusion
Hydatid cyst should be regarded as one of the differential diagnoses in patients with an isolated retrovesical cysts discovered during routine assessment for other conditions, such as patients presented with nonspecific symptoms of lower urinary tract, because prophylactic measures need to be considered in the operation to take spillage prevention in consideration.
References
- Shailesh S, Prem D, Tarun J, Ashish S, Sanjay S, et al. (2010) Isolated retrovesical hydatid cyst. BJUIw.
- Gogus O, Beduk Y, Topukcu Z (1991) Renal hydatid disease. Brit J Urol 68: 466-469.
- Engin G, Acunar B, Rozanes I, Acunar G (2000) Hydatid disease with unusual localization. Eur Radiol 10(12): 1904-1912.
- Rajesh S, Rupali B, Tariq A, Mandeep S (2004) Hydatid Cyst in Rectovesical Pouch, JK Science 6(2): 101-102.
- Khouaja MK, Ben Sorba N, Haddad N, Mosbah AT (2004) Retrovesical hydatid cyst: diagnosis and treatment in 8 cases. Prog Urol 14(4): 489- 492.
- Horchani A, Nouira Y, Chtourou M, Kacem M, Safta ZB (2001) Retrovesical Hydatid Disease: A Clinical Study of 27 Cases. Eur Urol 40(6): 655-660.
- Dogra PN, Taneja R (1995) Retrovesical hydatid cyst: an unusual cause for retention of urine. Ind J Urol 11(2): 82-83.
- Emira L, Karabuluta A, Balcia U, Germiyanoğlua C, Erola D (2000) An unusual cause of urinary retention: a primary retrovesical echinococcal cyst. Urology 56(5): 856.
- Angulo JC, Escribano J, Diego A, Sanchez-Chapado M (1998) Isolated retrovesical and extrarenal retroperitoneal hydatidosis: clinical study of 10 cases and literature review .J Urol 159(1): 76-82.
- WHO Informal Working Group (2003) International classification of ultrasound images in cystic echinococcosis for application in clinical and field epidemiological settings. Acta Trop 85(2): 253-261.
- Perigela HC, Reddy MK, Prasad BV, Narahari J (2013) Giant pelvic hydatid cyst. J Dr NTR Univ Health Sci 2(3): 218-221.
- Gossior KJ, Kontoyiannio DS, Dascalogiannaki M, Gourtsoyiannis NC (1997) Uncommon locations of hydatid disease: CT appearances. Eur Radiol 7(8): 1303-1308.
- Kotoulas G, Gouliamos A, Kalovidoures A, Vlahos L, Papavasiliou C (1990) Computed Tomographic localization of Pelvic hydatid disease. Eur Radiol 11(1): 38-41.
- Halefoglu M, Yasar A (2007) Huge Retrovesical Hydatid Cyst with Pelvic Localization as the Primary Site: A Case Report. Acta Radiol 48(8): 918- 920.
- Sarkar S, Sanyal P, Das M, Kumar S, Panja S (2016) Acute urinary retention due to primary pelvic hydatid cyst: a rare case report and literature review. J Clin Diagn Res 10(4): PD06-PD08.
- Alders N, Wojciechowski M (2017) An Isolated Retrovesical Hydatid Cyst in a Child: A Rare Case Presentation. Arch Parasitol 1: 103.
- Balik IAA, Celebi F, Basglu M, Oren D, Yildirgan I, et al. (2001) Intraabdominal extrahepatic echinococcus. Surg Today 31(10): 818-824.
- Shams-Ul-Bari, Arif SA, Malik AA, Khaja AR, Dass TA (2011) Role of Albendazole in the Management of Hydatid Cyst Liver. Saudi J Gastroenterol 17(5): 343-347.
- Emir L, Germiyanoglu C, Lokumcu A, Erol D (2001) Retrovesical echinococcal cyst causing renal failure an nocturnal enuresis in a child. Journal of Pediatric Surgery 36(7): 14.
© 2018 Azzawi M Hadi. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






