- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
Is Endoscopic Tympanoplasty a Better Alternative for Small Central Perforations? A Tertiary Care Experience
Renu Rajguru*
Department of ENT, INHS Ashwini, Mumbai, Maharashtra, India
*Corresponding author: Renu Rajguru, Department of ENT, INHS Ashwini, Mumbai, Maharashtra, India
Submission: August 24, 2022;Published: September 23, 2022

ISSN 2637-7780 Volume3 Issue2
Abstract
Introduction: Traditional approaches to tympanoplasty involve the use of a microscope. However, with
the advent of endoscopes and HD cameras, Endoscopic tympanoplasty has appeared as an alternate
to Microscopic tympanoplasty. Our study was aimed at assessing the success rates of endoscopic
tympanoplasty in small dry central perforations of pars tensa.
Materials and methods: A total of 49 patients were enrolled in this study who underwent endoscopic
myringoplasty and the surgical outcome was analysed in terms of graft uptake and post-op Air Bone gap
closure for a duration of six months.
Results: Among the study population, 45 participants (91.84%) had an intact neotympanum at the end
of 06 months, 2 participants (4.08%) had residual perforation and 2 (4.08%) recurrent perforations due
to URTI. The mean pre-op air-bone gap was 23.63dB±3.9dB in the study population with a minimum of
16dB and maximum of 31dB (95% CI 22.43 to 24.83), whereas the mean post-op air-bone gap was 13.84
dB±2.79 dB, minimum being 8 dB and maximum being 20 dB (95% CI 12.98 to 14.69). The difference
between the pre op and post op air bone gap was statistically significant (P value <0.001).
Conclusion: We conclude that endoscopic myringoplasty is an acceptable alternative to conventional
microscopic myringoplasty in terms of surgical outcomes and graft uptake, shorter operating time, better
visualisation, better cosmesis and reduced postoperative pain.
Keywords:Endoscopic tympanoplasty; Microscopic tympanoplasty; Surgical outcomes
Introduction
Chronic Otitis Media (COM) is an inflammatory disorder of middle ear cleft effecting 65- 330 million people worldwide, leading to hearing impairment in about 50% of the effected population [1]. COM is the result of an initial episode of acute otitis media, negative middle ear pressure or otitis media with effusion. Depending on the disease activity COM is classified as healed, mucosal or squamous type. It is an important cause of hearing loss, particularly in the developing world. Management options for COM mucosal type are topical antibiotic drops, surgery, a hearing aid or no treatment, depending on the symptomatology and the patient’s choice. In patients with a history of intermittent activity, surgery to close the perforation is indicated to minimize future activity and reduce patient’s hearing disability [2].
Tympanoplasty refers to any surgery involving reconstruction of the tympanic membrane and/or the ossicular chain after eradicating disease from the middle ear. Myringoplasty is a tympanoplasty without ossicular reconstruction [3].
Traditional approaches to tympanoplasty involve the use of a microscope as the binocular nature of vision and availability of both hands for surgery makes the microscopic technique a widely preferred one technique. However, microscope gives a magnified image in a straight line. Hence, while performing microscopic tympanoplasty, it is difficult to visualize certain areas like retrotympanum, attic and hypotympanum [4]. Also in the presence of anterior or posterior canal wall overhang, sometimes even the edges of perforation may not be visualised completely and the surgeon has to frequently adjust either the microscope or the patient’s head [5]. This leads to discomfort to the patient and increase in the duration of the surgery. With the advent of endoscopy and better cameras, Endoscopic tympanoplasty has appeared as an alternative to Microscopic tympanoplasty and is gaining popularity in recent years. It is less invasive with a wider field of vision and shorter operating time [6].
Materials & Methods
We conducted a descriptive study over a period of 2 years, from December 2018 to December 2020 at ENT department of our tertiary care academic medical hospital to assess the success rates of endoscopic tympanoplasty in small dry central perforations of pars tensa with an objectives to evaluate the efficacy of endoscopic myringoplasty by analysing the take up rate of temporalis fascia graft and postoperative audiometric results.
Methodology
A sample size of 49 patients attending the ENT OPD with tympanic membrane perforation consenting to undergo endoscopic tympanoplasty were considered as study population. Patients included in the study were cases of COM mucosal type with dry small central perforations of pars tensa, in the age group 18 years to 60 years. Patients with chronic Eustachian tube dysfunction, those with perforations of less than 3 months duration, smokers, patients with comorbidities like tuberculosis, Syphilis or HIV positive status, those on immunosuppressives or with compromised immunity, diabetics and those on ototoxic drugs were excluded from this study. Patients with underlying otosclerosis, suspected ossicular discontinuity, narrow or abnormal external ear canal, those having COM with any complications or those with COM Squamous type were also excluded from our study.
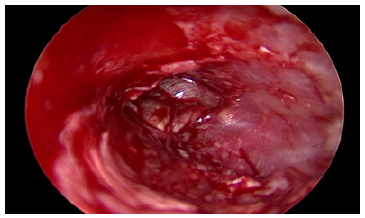
All cases were operated under local anesthesia with Lignocaine 4% in 1/80000 adrenaline. Injections were done in 4 points inside the canal at the bony- cartilaginous junction. A wide angle Storz Otoendoscope “0” degree (2.7mm diameter) connected to storz camera and a LED light source of 300 W were used. The camera was connected to a monitor with a video recording system. After cleaning and draping, the external auditory canal was cleaned with saline, and the endoscope was introduced through the canal to examine the perforation and insinuated in the middle ear to visualize its cavity as well as ossicles (Figure 1). Margins and the undersurface of the perforation were then freshened (Figure 2). Temporalis fascia graft was harvested by a separate incision in the supra-aural region after infiltration with the local anesthesia. Tympanomeatal flap was elevated by taking 12 o’clock to 6 o’clock incision till the annulus and the middle ear mucosa so visualized was incised to enter the middle ear (Figure 3). The handle of malleus was bared and the graft was placed by underlay technique (Figure 4). Tympanomeatal flap was reposited and gel foam pieces were placed in the middle ear and external auditory canal.
Figure 1: Endoscopic view of small central perforation.
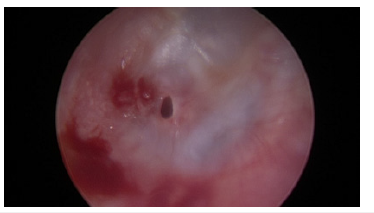
Figure 2:Edges of perforation freshened.
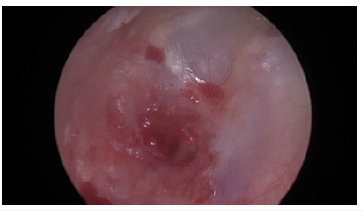
Figure 3: Middle ear mucosa seen after elevating tympanomeatal flap.
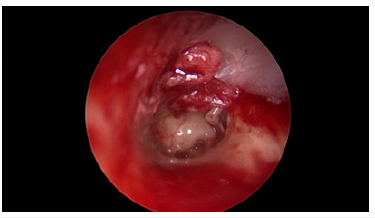
Figure 4: Graft in situ.
The patients were then reviewed weekly for the first three weeks and monthly subsequently for six months. A repeat Pure Tone Audiometry was performed at the end of six months. The patients’ pre and post-operative audiograms were compared and analysed.
Statistical analysis
IBM SPSS version 22 was used for statistical analysis. Categorical variables at different time periods of follow-up compared using the McNemar test. The change in the quantitative parameters, before and after the intervention was assessed by paired t-test. Descriptive analysis was carried out by mean and standard deviation for quantitative variables, frequency and proportion for categorical variables.
Results
A total of 49 patients were included in the final analysis. The mean age of the patients was 38.04 years+11.85 years with the youngest being 18 years and the oldest patient of the cohort was 57 years of age. The cohort had an almost equal gender distribution with 25 male and 24 female patients. Only small central perforations were included in the study, we had 2 antero-superior perforations, 18 postero-inferior perforations, 15 central perforations and 14 antero-inferior perforations.
The average time taken for a surgery was around 1.25hrs with a standard deviation of 0.14hrs.
Among the study population, 45 participants (91.84%) had an intact neotympanum at the end of 06 months, 2 participants (4.08%) had residual perforation and 2 (4.08%) recurrent perforations due to URTI. The recurrent perforations were managed with TCA cauterisation and silastic sheet application.
The mean pre-op air-bone gap was 23.63dB±3.9dB in the study population with a minimum of 16dB and maximum of 31dB (95% CI 22.43 to 24.83), whereas the mean post-op air-bone gap was 13.84 dB±2.79dB, minimum being 8dB and maximum being 20dB (95% CI 12.98 to 14.69). The difference between the pre op and post op air bone gap was statistically significant (P value <0.001).
Discussion
Since the introduction of tymapnoplasty in the 1950s, a variety of surgical techniques have been developed, though the conventional microscopic technique through a post aural incision is the most popular one [7]. The problems with this technique are primarily related to the postaural scar and vision in a straight field which many a times requires canal wall drilling. Postaural incision leads to increased tissue handling and tissue dissection, thus causing an increased incidence of pain, paraesthesia or hypoaestheisa around the incision and pinna.
However, with the advent of the endoscopes and better visualisation, endoscopic tympanoplasty is fast becoming an attractive option. The endoscopic technique is a minimally invasive surgery that offers unique set of advantages like quicker operating time, easily manoeuvrable field of view with good visualisation, better cosmesis; as well as availability of angled visualisation and less tissue dissection. However, space constraints, use of one hand to manoeuvre the endoscope and constant fogging/smearing of the tip lead to a steeper learning curve for endoscopic tympanoplasty [6].
Operational success in cases of tympanoplasty are usually described on the basis of graft uptake and Air-Bone gap (AB gap) closure. Graft success rates as elicited by various studies for endoscopic groups varies from 79% to a 100%. In our study we achieved a success rate of 91.84%. Furthermore, Lade et al. [8]; Harguop et al. [9]; Tseng et al. [10]; Kuo et al. [11]; Jyothi et al. [5]; Guler et al. [4]; and Mokbel et al. [7] in their respective studies found that graft uptake for endoscopic tympanoplasty gives comparable or even better results when measured against microscopic tympanoplasty [4,5,7-11].
The AB gap gain was used as the other standard measure to ascertain the surgical outcome of endoscopic tympanoplasty in our study. We had used temporalis fascia as the graft material. We found the mean pre op air bone gap was 23.63±3.9 whereas post op air bone gap was 13.84±2.79 and this was statistically significant (P value <0.001). Our results are corroborated by other studies which also claim a favourable and significant difference in the AB gap closure in endoscopic tympanoplasty. Thus, eliciting the fact that endoscopic tympanoplasty leads to a significant closure of AB gap as compared to pre-operative levels [3-14]. The use of the endoscope comes with its own sets of advantages and challenges; however, the skill set is adaptable; plus, with the advent of endoscopic suites; the set-up is readily available at most ENT centres to which an oto-endoscope can be easily added. The post op cosmesis is much better since the post-auricular scar is avoided. Thus, endoscopic tympanoplasty aids in increasing patient satisfaction [15,16].
Endoscopic tympanoplasty also doubles up as an excellent teaching tool for Middle ear anatomy. The use of angled microscopes allows one to easily demonstrate and access the anatomy of the socalled hidden areas of the ear like the sinus tympani, hypotympanum and retrotympanum at the same time giving a close-up view of the middle ear with excellent details [17].
At the end of our study, we were able to ascertain that Endoscopic tympanoplasty offers good success rates and leads to a significant hearing improvement and thus forms a lucrative option to microscopic tympanoplasty
Conclusion
Our study concluded that endoscopic myringoplasty offers better visualisation of key areas of middle ear, the rate of graft success is high with good improvement in air-bone gap, allows more natural and direct access to the middle ear, better cosmesis and reduced pain.
References
- World Health Organization (WHO) (2004) Chronic suppurative otitis media: burden of illness and management options. Geneva, Switzerland.
- Health A (2004) Chronic suppurative otitis media burden of illness and management options.
- Kumar M, Kanaujia SK, Singh A (2015) A comparative study of endoscopic myringoplasty vs conventional myringoplasty. Otorhinolaryngology Clinics 7(3): 132-137.
- Guler İ, Özcan M (2019) A comparison of endoscopic and microscopic techniques for the repair of tympanic membrane perforations. ENT Updates 9: 166-171.
- Jyothi AC, Shrikrishna BH, Kulkarni NH, Kumar A (2017) Endoscopic myringoplasty versus microscopic myringoplasty in tubotympanic CSOM: A comparative study of 120 cases. Indian Journal of Otolaryngology and Head and Neck Surgery 69(3): 357-362.
- Garcia L de B, Moussalem GF, Andrade JSC de, Mangussi-Gomes J, Cruz OLM, et al. (2016) Transcanal endoscopic myringoplasty: A case series in a university center. Brazilian Journal of Otorhinolaryngology 82(3): 321-325.
- Mokbel KM, Moneir W, Elsisi H, Alsobky A (2015) Endoscopic transcanal cartilage myringoplasty for repair of subtotal tympanic membrane perforation: A method to avoid postauricular incision. J Otolaryngol Rhinol 1.
- Lade H, Choudhary SR, Vashishth A (2014) Endoscopic vs microscopic myringoplasty: a different perspective. European Archives of Oto-Rhino-Laryngology 271(7): 1897-1902.
- Harugop AS, Mudhol RS, Godhi RA (2008) A comparative study of endoscope assisted myringoplasty and micrsoscope assisted myringoplasty. Indian Journal of Otolaryngology and Head & Neck Surgery 60(4): 298-302.
- Tseng CC, Lai MT, Wu CC, Yuan SP, Ding YF (2017) Comparison of the efficacy of endoscopic tympanoplasty and microscopic tympanoplasty: A systematic review and meta-analysis. Laryngoscope 127(8): 1890-1896.
- Kuo C hung, Wu H Mei (2017) Comparison of endoscopic and microscopic tympanoplasty. European Archives of Oto-Rhino-Laryngology 274(7): 2727-2732.
- Mohanty S, Manimaran V, Umamaheswaran P, Jeyabalakrishnan S, Chelladurai S (2018) Endoscopic cartilage versus temporalis fascia grafting for anterior quadrant tympanic perforations - A prospective study in a tertiary care hospital. Auris Nasus Larynx 45(5): 936-942.
- Lou ZC (2020) Endoscopic myringoplasty: Comparison of double layer cartilage-perichondrium graft and single fascia grafting. Journal of Otolaryngology - Head and Neck Surgery 49(1).
- Chozhan P, Sankara Subramanian M, Kannathal D, Malarvizhi R (2018) Comparative study between endoscopic cartilage myringoplasty and endoscopic temporalis fascia myringoplasty. International Journal of Otorhinolaryngology and Head and Neck Surgery 5(1): 24.
- Taneja V, Milner TD, Iyer A (2020) Endoscopic ear surgery: Does it have an impact on quality of life? Our experience of 152 cases. Clinical Otolaryngology 45(1): 126-129.
- Kanona H (2015) Endoscopic ear surgery: A case series and first United Kingdom experience. World Journal of Clinical Cases 3(3): 310.
- Anschuetz L, Siggemann T, Dür C, Dreifuss C, Caversaccio M, et al. (2021) Teaching middle ear anatomy and basic ear surgery skills: A qualitative study comparing endoscopic and microscopic techniques. Otolaryngology-Head and Neck Surgery 165(1): 174-178.
© 2022 Renu Rajguru. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






