- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
Left External Jugular Phlebectasia: Rare Presentation in Adults; Sign of a Deep, Dangerous Lesion?
Rachana Agrawal*
Consultant ENT surgeon, Bharatiya Arogyanidhi Hospital, India
*Corresponding author: Rachana Agrawal, Consultant ENT surgeon, Bharatiya Arogyanidhi Hospital, Maharashtra, India
Submission: August 15, 2018;Published: September 28, 2018

ISSN 2637-7780 Volume2 Issue5
Abstract
Jugular phlebectasia is a rare condition, seen in children, on the right side. It is more commonly seen in the internal jugular vein as compared to the external jugular vein. In this case report, we present an adult female with a left sided external jugular venous phlebectasia. It usually presents as a neck swelling which increases in size on coughing, straining, Valsalva manoeuvre. Complications may include hoarseness of voice, Horner’s syndrome, phlebitis, thrombosis, intracranial extension and congestive cardiac failure. The treatment is usually conservative. Due to the rarity of this condition, it is often misdiagnosed. With this case report we would like to increase the awareness of this condition. If diagnosed correctly when present, will avoid unnecessary investigations and appropriate management can be undertaken swiftly. Though rare in adults, jugular phlebectasia should be considered as a possibility in all cases of left venous dilatation without associated co-morbidities.
Keywords: External jugular phlebectasia; Internal jugular phlebectasia; Venous dilatation; Jugular aneurysm
Abbreviations: EJV: External Jugular Phlebectasia; IJV: Internal Jugular Phlebectasia; USG: Ultrasonography
Introduction
Jugular phlebectasia is rare condition presenting as an isolated fusiform dilatation of the jugular vein [1]. It is most commonly seen in the internal jugular vein, followed by the external jugular, anterior jugular and then the superficial communicating veins [2]. It usually presents on the right side [3] and in children as an intermittent neck swelling which increases in size on coughing, straining, sneezing and Valsalva manoeuvre. External jugular phlebectasia is rarely seen, rarer still in adults and frequently misdiagnosed or managed inappropriately. It differs from varices, due to the lack of tortuosity and from aneurysms which are segmental, saccular and secondarily acquired. Differential diagnosis of this condition may include laryngocele, branchial cyst, or superior mediastinal cysts [2]. The treatment is controversial however conservative treatment is preferred in asymptomatic masses and regular follow up is recommended. Surgery is advised in the presence of complications or for cosmetic reasons. In our report we present a case of external jugular phlebectasia in an adult, on the left side (Figure 1). Due to the rarity of this condition, its unique presentation on the left side, especially in adults, a high index of suspicion is required to recognise it and differentiate it from other swellings or a cardiovascular condition. We also highlight the importance of avoiding over-investigations and invasive investigations which could be catastrophic.
Figure 1:Enlarged left jugular vein.

Case Report
A 42-year-old woman came with a complaint of a swelling on the left side of her neck noticed since one month. This elongated swelling was insidious in onset and appeared only while coughing, laughing, or talking for a long duration. She did not complain of fever, difficulty in breathing or swallowing, change in voice, and cough or chest pain (Figure 2). There was no history of trauma or surgery. On examination, there was a fusiform elongated swelling, on the left side of her neck, anterior to the sternocleidomastoid muscle, along the course of the external jugular vein. It appeared only on coughing, laughing, talking for a long time or doing the Valsalva manoeuvre. The swelling was soft, compressible, non-tender, non-pulsatile and non-transilluminator. No palpable thrill, no audible bruit was heard over the swelling. The neck lymph nodes were not palpable. Oropharyngeal and systemic including cardiovascular examination was normal. Laryngoscopy was normal. USG of neck showed a dilatation of the left external jugular vein with a prominence of the left internal jugular vein which increased with Valsalva manoeuvre. The Doppler study showed turbulence in both the veins without any thrombosis. The patient was counselled regarding the nature of the condition and conservative management with regular follow up was advised. She was advised to seek immediate medical counsel if the symptoms increased or new symptoms such as hoarseness, difficulty in breathing or swallowing occurred.
Figure 2:Increased prominence of the EJV on laughing.

Discussion
Phlebectasia is a rare condition where there is an outward dilatation of the entire vein without any tortuosity, differentiating it from a varix. It usually presents on the right side and in children. In our case report, the patient is a 45-year-old female, presenting with the condition on the left side. Jugular phlebectasia usually presents as a soft compressible swelling in the neck, in the paediatric age group. It may affect any neck vein, though most commonly it affects, in decreasing order, the internal jugular, external jugular, anterior jugular and superficial communicating veins [2]. It is seen twice more commonly in boys as compared to girls, and more often on the right side [4]. It was first reported by Zukschwerdt [5] and subsequently by Gerwig [1].
Many theories have been proposed to explain why the right side involvement is higher, such as those proposed by Dhillon [6] where he states that the right internal jugular vein is larger than the left in most of the people, the right brachiocephalic vein is in direct continuity with the superior vena cava, and there are no valves in right brachiocephalic vein as compared with the left. La Monte hypothesized the internal jugular phlebectasia (IJP) occurs more commonly on the right side as the right innominate vein lies in contact with the right apical pleura, any increased intrathoracic pressure would increase the pressure on the internal jugular vein [3].
Isolated left sided internal jugular phlebectasia was seen in only 7 out of 51 children with IJP by Li Jianhong [7]. Nasser Al- Tamami reported in a case report and review of literature; the left sided was involved in only 2 out of 26 cases and only 2 cases out of 26 were seen in adults [8]. The etiology is unclear, and may occur due to anatomical abnormality, mechanical compression, trauma, congenital structural defects [4]. Complications include; hoarseness of voice, Horner’s syndrome, phlebitis, thrombosis, intracranial extension and congestive cardiac failure [9]. Ultrasonography or Colour Doppler flow imaging ultrasound, along with a Valsalva manoeuver is the investigation of choice to confirm the diagnosis because of its clarity, safety and low cost [7]. A USG can help differentiate it from other causes of neck swellings including laryngocele or branchial cysts. Other diagnostic tests that have been recommended in literature include direct needle aspiration, venography, arteriography and computed tomography [10]. Treatment is usually not indicated in asymptomatic patients as it a benign self-limiting condition. Surgery is recommended if complications occur or for cosmetic reasons. External jugular Phlebectasia has rarely been reported, and it is rarer still in adults.
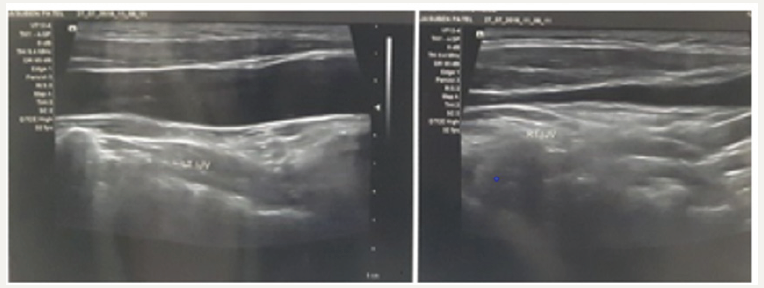
In adults, left sided jugular phlebectasia was described by Tohru Tanigawa, from Japan, in a 74-year-old elderly female [11]. Right sided lesions in adults, which are more common, were reported by Ozdemir [12], who reported a case of right EJP with duplication of the internal jugular vein in 2004, Pandey [13] reported a surgically managed case in a 24-year-old male in 2008 and in 2014, Matsunaga k [14], who noticed an incidental finding of a right sided EJP in an 81-year-old man undergoing surgery for hernia. In this case report we try to highlight the diagnosis of an external jugular venous phlebectasia on the left side, in an adult. The internal jugular vein is also dilated which was only detected by the ultrasonography report. This may lead to complications like hoarseness and difficulty in swallowing, if enlarged. Thus, the diagnosis of jugular phlebectasia should be considered, though rare, in all cases of left venous dilatation. Unnecessary investigations for cardiovascular diseases also may be avoided if diagnosed early. A good clinical examination and a USG and a Doppler can diagnose this condition accurately and help differentiate it from other neck swellings (Figure 3). A raised jugular venous pressure may also appear as the similar presentation; however, it is more on the right side, associated with cardiac failure and pulsations may be seen only on supine position at a 45-degree angle. With this case report we would like to increase the awareness of this condition if diagnosed correctly when present, will avoid unnecessary investigations and appropriate management can be undertaken swiftly.
Figure 3:USG showing increased prominence of the internal jugular vein.
References
- Gerwig WH (1952) Internal jugular phlebectasia. Ann Surg 135(1): 130-133.
- Abdulla AS, Aldabagh MH (2008) Congenital phlebectasia of the internal jugular vein. Dohuk Med J 4(2): 155-160.
- Monte SJ, Walker EA, Moran WB (1976) Internal jugular phlebectasia. A clinicoroentgenographic diagnosis. Arch Otolaryngol 102(11): 706-708.
- Vicente HL (2001) Jugular phlebectasia. Pediatric surgery update 18: 2.
- Zukschwerdt L (1929) Rare localization of a venectasia. Dtsch Z Chir 216: 283-285.
- Dhillon MK, Leong YP (1991) Jugular venous aneurysm-a rare cause of neck swelling. Singapore Med J 32(2): 177-178.
- Jianhong L, Xuewu J, Tingze HU (2006) Surgical treatment of jugular vein phlebectasia in children. The American Journal of Surgery 192(3): 286-290.
- Amami AlN, Macki K (2015) Internal jugular phlebectasia: a case report and literature review. J Otolaryngol ENT Res 2(6): 00045.
- Swami H, Nambiar S (2009) Focal ectasia of internal jugular vein. Medical Journal, Armed Forces India 65(3): 282-283.
- Sander S, Elicevik M, Ural M, Vural O (1999) Jugular phlebectasia in children: is it rare or ignored? J Pediatr Surg 34(12): 1829- 1832.
- Tanigawa T, Shiga RAS, Murohara T (2014) Left jugular phlebectasia in an elderly patient. circulation 130(16): 1416- 1417.
- Ozdemir S, Coskun H, Balban M (2004) Phlebectasia of the external jugular vein associated with duplication of the internal jugular vein. Clin Anat; 17(6): 522-525.
- Pandey M, Kumar P, Khanna A (2008) Phlebectasia of the external jugular vein. The Internet Journal of Surgery 19(1).
- Matsunaga K, Kishi K (2014) Phlebectasia of the external jugular vein with thrombosis: Report of a case. Surg Today 44(6): 1180- 1184.
© 2018 Rachana Agrawal. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






