- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
Drug Induced Sleep Endoscopy, Our Experience
Mastrapasqua RF1*, Scarano E1, Fiorita A2, Mastrapasqua RF1, Marchese MR1, Marrone S1, Loperfido A1, Rizzotto G2,Paludetti G1
1 Department of Head and Neck Surgery, Catholic University of Sacred Hearth, Italy
2 Department of Neuroscience, Catholic University of Sacred Hearth, Italy
*Corresponding author: Mastrapasqua RF, Department of Head and Neck Surgery, Otorhinolaryngology, Catholic University of Sacred Hearth, Roma, Italy
Submission: June 12, 2018;Published: August 14, 2018
ISSN: 2637-7780Volume2 Issue2
Introduction
Drug Induced Sleep Endoscopy (DISE) is an important hub in diagnostic pathway of patients affected by Obstructive Sleep Apnea Syndrome (OSA) providing useful information that can be useful for all the different professionals involved in this patient’s management involving surgical or medical [1,2] decisions such as determining the exact anatomical structure involved in obstruction. During the procedure can be performed different test that can predict efficacy of different treatments such as mandibular advancements, hypoglossal stimulation and Mandibular advancement device fitting test that can further improve therapy addressing and surgical planning [3]. Knowing the anatomical site involved and the obstruction mechanism can lead to minimize the effort and combining multiple therapeutic approaches to maximize results and minimize side effects. Now there is no standard consensus on which classification to adopt and regional consensus as European Position Paper on DISE [4] are still not universally applied, therefore there are no Italian data on the most common obstruction pattern on a large population sample.
Methods
In this retrospective study we evaluated 286 consecutive DISE reports from January 2015 to June 2018 from the Sleep department in Policlinico Gemelli Hospital. All patients underwent our clinics standard diagnostic pathway: otolaryngology pre-operative evaluation comprehensive of fibre optic nasopharyngoscopy with Muller’s maneuver and Sleep medicine evaluation by objective items as home respiratory polygraphy (Somntè Recording Unit©, Somntè Compumedics Australia), BMI, neck circumference and a neurological exam, and Subjective evaluation. Subjective evaluation was obtained by means of Italian translation of strongly validated questionnaires, named Sino-Nasal Outcome Test (SNOT- 20), sleepiness through Epworth Sleepiness Scale (ESS) and Berlin questionnaire [5]. During the same surgery session, all patients underwent DISE and inferior turbinates decongestion, Anaesthesiologist, Neuroelectrophysiology Technician and Otorhinolaryngologic were attending the procedures.
Patients, already prepared for polygraphic intraoperative recording, received drug sedation. For drug sedation we used increasing dose of Propofol (3mg/kg/h) until continuous BiSpectral Index (BIS) monitoring by Aspect A-2000 BIS monitor© (Apect Medical Systems, Natick, MA), was between 45-65. During snoring, we use flexible nasopharyngoscopy trough the nasal cavity evaluating the pattern and degree of obstruction (nasopharynx, oropharynx hypopharynx and larynx) and continuously monitoring the sleep through polygraph (Somntè Compumedics System©, Somntè Compumedics Australia). We also performed a bimanual pull up mandibular advancement maneuver, advancing at 75% maximum confort advancements (4 to 5mm), evaluating masseter muscle activation and visualizing the effect on airway obstruction. The anatomical site and the magnitude of the obstruction are classified following a modified version of the classification proposed by Vicini [6]. At the end of DISE procedure all patients underwent Inferior turbinates decongestion to improve CPAP compliance [7- 9]
Table 1:Modified vicini classification.
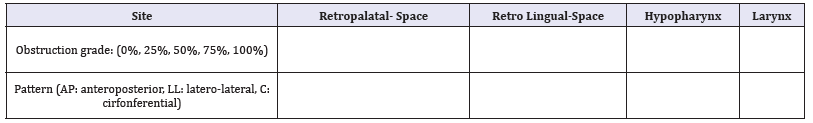
The classification was compiled as shown in Table 1, it was also specified in case of laryngeal obstruction the mechanism of obstruction as trap-door closing of epiglottis, vocal folds spasm or edema. All procedures were made by the same operators and all the reports were rewieved by the same investigators
Results
The most common obstruction site is retropalatal space, most frequently completely: 100% in 83.4% cases (236/286), 75% in 11% (31/286), 50% in 3.5% cases (10/286) 25% in 0.7% (2/286) e 0% in 1.4% (4/286). The most common obstruction pattern of this site was concentrically (72.4% cases, 202/279) then anteroposterior (25.1%, 70/279) and lateral (2.5% 7/279). The following was retro-lingual space 100% in 24.3% cases (68/286), 75% in 23.9% (67/286), 50% in 24.6% cases (69/286) 25% in 15% (42/286) e 0% in 12.1% (34/286). The two most frequent patterns are antero-posterior 40.7% (100/246) and circumferential 40.2% (99/246), lateral pattern is less common 19.1% (47/ 246).
Hypopharynx was less involved: 100% in 1.4% cases (4/286), 75% in 3.1% (9/286), 50% in 1.4% cases (4/286) 25% in 1% (3/286) e 0% in 93.0% (266/286). The obstruction is mostly circumferential 60% (12/20), then lateral 35% (7/20), less common antero-posterior 5% (1/20). Larynx was involved at 100% in 5.9% cases (17/286), 75% in 1.7% (5/286), 50% in 1.7% cases (5/286) 25% in 1.7% (5/286) e 0% in 88.8% (254/286), the majority is anteroposterior 71.9% with a trap-door movement of the epiglottis (23/32), some are lateral for the closure of vocal folds 21.9% (7/32) or circumferential 6.3% (2/32).
Combined obstruction is frequent retropalatal and retro-lingual 87.5% of patient with retropalatal obstruction (244/279) while only 7.2% (10/279) had involved also Hypopharynx, and 11.5% (32/279) Larynx. Of the 32 patients whose Larynx was involved 53.1% (17/32) had an Hypopharyngeal association.
Conclusion
Due to lack of consensus about DISE classification and the absence of large literature samples it is difficult to confront our data with literature. It is remarkable that cranial obstructions are far more frequent than caudal obstructions and frequently more complete, also the most frequent obstruction is a circumferential retropalatal obstruction and that can be a strong point in proposing mandibular advancement, Laryngeal and Hypopharyngeal are associated in 53% cases. Knowing the site of obstruction can lead to a better therapeutic planning in OSA patients aiming the best and less invasive surgical procedure thus combining surgery with other approaches such as Mandibular Advancement devices, Positional therapy or electrostimulation.
References
- Huntley, Chou D, Doghramji K, Boon M (2017) Preoperative drug induced sleep endoscopy improves the surgical approach to treatment of obstructive sleep apnea. Ann Otol Rhinol Laryngol 126(6): 478-482.
- De Corso E, Bastanza G, Della Marca G, Grippaudo C, Rizzotto G, et al. (2015) Drug-induced sleep endoscopy as a selection tool for mandibular advancement therapy by oral device in patients with mild to moderate obstructive sleep apnoea. Acta Otorhinolaryngol Ital 35(6): 426-432.
- Bosi M, De Vito A, Vicini C, Poletti V (2013) The predictive value of Muller’s maneuvre for CPAP titration in OSAHS patients. Eur Arch Otorhinolaryngol 270: 2345–2351.
- De Vito A, Carrasco Llatas M, Vanni A, Bosi M, Braghiroli A, et al. (2014) European position paper on drug-induced sedation endoscopy (DISE). Sleep Breath 18(3): 453-465.
- Lawrence JE, Kristo D, Strollo PJ, Friedman N, Malhotra A, et al. (2009) Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 5(3): 263-276.
- Vicini C, De Vito A, Benazzo M, Frassineti S, Campanini A, et al. (2012) The nose oropharynx hypopharynx and larynx (NOHL) classification: a new system of diagnostic standardized examination for OSAHS patients. Eur Arch Otorhinolaryngol 269(4): 1297–1300.
- Fiorita A, Scarano E, Mastrapasqua R, Picciotti PM, Loperfido A, et al. (2018) Moderate OSAS and turbinate decongestion: Surgical Efficacy in improving the quality of life and compliance of CPAP using Epworth Score and SNOT-20 score. Acta Otorhinolaryngolocial Ital 38(3): 214-221.
- Hsueh YL, Ying L, Ning HC, Lee LA, Fang TJ, et al. (2008) Improvement in quality of life after nasal surgery alone for patients with obstructive sleep apnea and nasal obstruction. Arch Otolaryngol Head Neck Surg 134(4): 429-433.
- Kim ST, Choi JH, Jeon HG, Cha HE, Kim DY, et al. (2004) Polysomnographic effects of nasal surgery for snoring and obstructive sleep apnea. Acta Otolaryngol 124(3): 297-300.
© 2018 Mastrapasqua RF. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






