- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
The Comparative Study of Underlay and Overlay Tympanoplasty Without Chain Reconstruction Effect on the Improvement of Hearing Loss and Tympanic Landmarks Among Patients with Otitis Media Who Referred to Alzahra and Ayatollah Kashani Hospitals During 2016-2017
Shahpour Kouhpaei*
Isfahan University of Medical Sciences, Iran
*Corresponding author: Shahpour Kouhpaei, Isfahan University of Medical Sciences, Isfahan, Iran
Submission: March 13, 2018;Published: August 01, 2018

ISSN 2637-7780 Volume2 Issue1
Abstract
Background: Perforated tympanic membrane and middle ear infection are among common complications treated by tympanoplasty. This study was aimed to compare the effects of underlay and overlay tympanoplasty on the improvement of hearing and tympanic membrane landmarks and post operative complications as well.
Methods: In a clinical trial study 62 patients with perforated tympanic membrane were selected and randomly divided in the two groups of 31. The first group was operated by overlay and the second group was operated by underlay tympanoplasty. All patients were followed in 3 and 6 months after surgery and improvement of the hearing, tympanic membrane land marks and post operative complications were compared between the two groups.
Findings: Three and six months after surgery, tympanic landmarks in both groups improved but there was no significant difference between the two groups but improvement of hearing threshold in frequencies of 1000 and 4000 was better in the overlay graft. The overall improvement in the overlay graft was 83.8% and in the underlay graft was 64.5% and no statistically significant difference was observed between the two groups (p=0.21).
Discussion: Our study showed improvement of hearing, success rate of operation, recurrence, and post operative complications were not different between overlay and underlay tympanoplasty methods. But the improvement of hearing in some frequencies was better in overlay method, although overlay tympanoplasty is more difficult. But if sufficient precision is given in this method itwill be safe and provides more favorable hearing results.
Keywords: Tympanoplasty; Overlay and underlay graft; Hearing Improvement
Introduction
Global statistics reflect an increasing rate of prevalence and side effects resulted from the middle ear infection. The perforated tympanic membrane, middle ear ossicle necrosis and ultimately hearing loss are among the most important ones [1]. Tympanoplasty is one of the most common surgical procedures in the field of ear diseases. In this process, the previous perforated tympanic membrane is recovered through a variety of grafts including allograft, homograft and Autograft. Most surgeons use autologous grafts such as Temporal is muscle fascia, tragus cartilage, vein walls, and etc. to recover the hole [1,2] Tympanoplasty is divided into 5 types based on bone reconstruction [3-6]. The purpose of the tympanoplasty is to make a mechanism for voice conduction and closing perforation. It improves two important hearing-related functions, which include increasing the ratio of the tympanic area to the oval window playing the most important role in voice enhancement, and preventing the sound from reaching the round window simultaneously [7].
Different methods and techniques are used for surgery. Some surgeons use the back of the ear incision and some the AURAL one.Despite the various methods and techniques and numerous studies that have been done so far,the effects of tympanoplasty on hearing improvement is still contraversial and different degrees of recovery are mentioned for this method [8-11]. Therefore, due to different results and high prevalence of complications including tympanic perforation which makes the timpanoplasty surgery essential most often, this study aims to determine the effects of Type I Tympanoplasty (without chain reformation) on hearing improvement in patients with a history of middle ear otitis.
Materials and Methods
This study is a clinical trial one conducted in 2015 and 2016 in al-Zahra and Ayatollah Kashani medical centers in Isfahan. The target population includes the age range of 18-60 year old patients suffering from Tympanic perforation who were candidates for Tympanoplasty Type 1surgery. (Without Chain reformation)The criteria for participation include patients aging from 18 to 60 years old and suffering from tympanic perforation due to trauma or chronic otitis media, no previous surgery on the ear, the absence of other ear diseases such as NIHL, otosclerosis, congenital hearing loss, and systemic diseases. Also, the patient’s refusal to continue for various reasons and no more referrals were considered as exclusion criteria.
The sample size required for the study was calculated using the formula for estimating the sample size for comparing the means and considering the 95% confidence level, the test power of 80%, the standard deviation of the hearing threshold level, which is estimated at 1/1 and the least significant difference between the two groups, which was 0.8, in 30 patients in each group. A total of 62 patients were studied in two groups of 31. The study was conducted after approving the proposal and obtaining a permit from the University’s Medical Ethics Committee, and 62 patients were selected for type 1 Tympanoplasty. Before surgery, all patients did the audiometry test and their hearing level was determined at different frequencies. Patients’ audiogram was performed for both ears. Other essential information including demographic characteristics, history of the disease, and duration of the current illness were asked and recorded in their forms.
Patients were randomly distributed to two groups of 31 patients. The first group did overlay (without chain correction) and 31 other patients all did underlay graft of Tympanoplasty Type I. All of the patients were under audiometric study before, 3 and 6 months later, and their hearing threshold was measured before and after the operation and compared between the two groups. Also, complications such as tinnitus, recurrence and perforated tympanic membrane were studied in two groups. All surgeries and audiometry tests were performed by a qualified audiologist and a surgeon at the al-Zahra and Kashani medical centers in Isfahan. Data were collected and stored in the computer and then analyzed by SPSS version 24 and T-test, T-paired, Chi-square, Mann-Whitney and ANOVA along with repeated observations.
Results
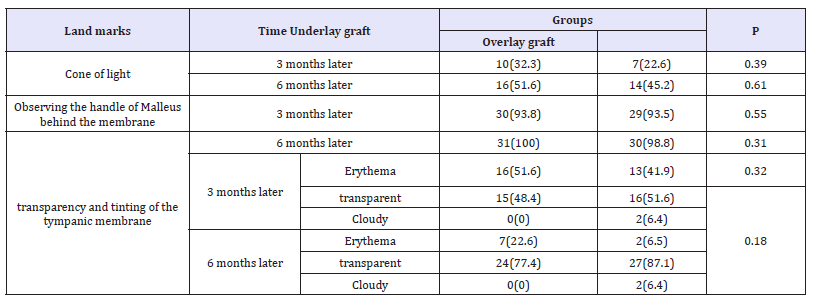
In this study, 62 patients with the average age of 43.6±9 years were studied including 24 males and 38 females. The demographic data of patients did not show any significant difference between the two groups regarding the mean age and duration of illness and the frequency of sex, cause of referral and the side involved. In (Table 1), the results of the three landmarks involving (observing the cone of light), 2 (observing the handle of Malleus from the tympanic membrane) and 3 (tympanic transparency and tinting) in the 3rd and 6th months of the operation in the two groups under overlay and underlay graft are shown. According to this table, the condition of these landmarks was not significantly different in the two groups, 3 months and 6 months later.
Table 1:Frequency distribution of Landmarks 1, 2 and 3 at 3 and 6 months of operation in two groups.
In Table 2, the mean and standard deviation of auditory thresholds before, after 3 and 6 months of the operation are shown in two groups. There was no significant difference in hearing threshold between the two groups in terms of results at any time intervals. Although changes were the same in the two groups,the auditory threshold in the overlay grafting group was significantly different from the other one at frequencies of 500, 1000 and 4000. The analysis of the AB gap before, 3 months and 6 months after operation showed that this variable was not significantly different between the two groups at any time intervals and there was no significant difference in the trend of changes during the study and it significantly decreased in both groups (Table 2).
Table 2:Mean and standard deviation of auditory threshold before and after operation in two groups.
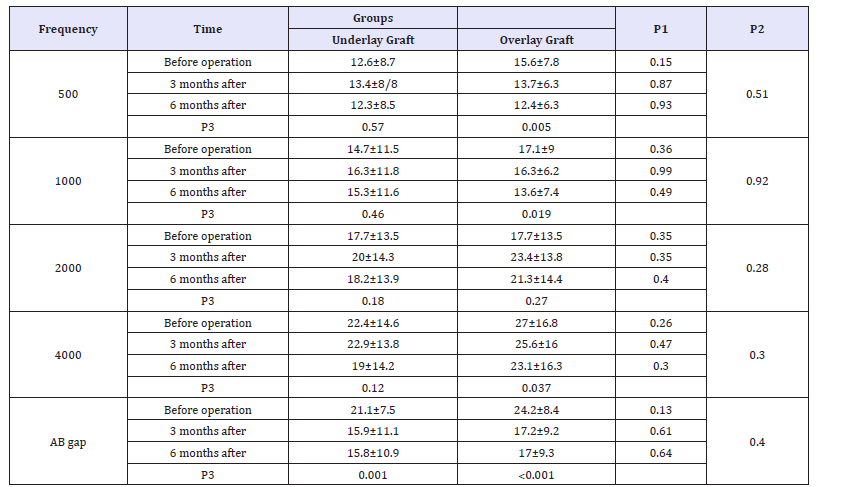
P1=Significant level of hearing threshold difference between the two groups at each time point by T-test
P2=Significance level of hearing loss threshold changes between two groups according to ANOVA test with repetition of observations
P3=Significant level of change in auditory thresholds within each group in terms of ANOVA test with repeated observation
Figure 1:Frequency of recovery 3 months and 6 months after surgery in two groups.

In (Figure 1), the percentage of hearing improvement status in 3 months and 6 months after surgery is shown in two groups of grafts. According to the figure, the overall improvement in the overlay graft group was 83.8% and it was 64.5% in the opposite one, (an improvement of 80.6% in the underlay graft group and 64.5% in the overlay graft group were relative). There was no significant difference between the two groups according to the Mann-Whitney test (p=0.21). The frequency of tinnitus in the underlay graft group was 48.4%, 45.2% and 38.7%, respectively, and in the other one was, 58.1%, 51.6% And 45.2%, before and 3 and 6 months later and the presence of tinnitus was not significantly different between the two groups at any time.
During the study period, the disease recurred in 5 patients including 3 from the underlay graft and 2 from the overlay graft group (9.7% vs. 6.5%), but the difference between the two groups was not significant (p =0.64).For postoperative complications, 20 patients from each group suffered from post-operative complications, including hearing impairment, ear itching, tinnitus ear pain and otorrhea. The frequency of these complications in the underlay graft group was 22.6%, 35.5%, 25.8%, 16.1% and 2.3% respectively, and in another one was, 29%, 41.9%, 25.8%, 9.7% and 3.2% respectively. There was no significant difference between the two groups (P=0.84).
Discussion
Tympanic perforation is a common complication in patients referred to ENT clinics, which is mainly due to the middle ear infection or trauma. The tympanic membrane rupture and middle ear bones loss lead to hearing problems and even severe deafness if left untreated. In the tympanic graft, it can usually be done from the two positions overlay and underlay. Although both methods are used, it seems that the success rate of the operation and the complications of the post operative are different in the two methods. In this study, 62 patients with tympanic membrane perforation were compared in two groups of 31. Both groups were not significantly different in terms of demographic and basal variables such as age, sex, duration of disease, patient complaint and operation side and there were no side effects of the abovementioned factors on the hearing and landmarks. Compared to the results, the tympanic landmarks, including observing optical cones, Malleus bone and tympanic transparency and tinting, improved in both groups, but no significant differences were observed between the two groups and patients with both grafting methods were approximately the same.
Findings of the audiometry at different frequencies before, and 3 and six months later showed that hearing thresholds at a frequency of 1,000 and 4,000 were better in patients who had done tympanic overlay grafting, but there was no significant difference in other frequencies between the two groups. In general, the rate of recovery in the two groups was not significantly different, and about 80% of the patients had a relative improvement 3 and 6 months later. In a study conducted by Amiri Devan et al. [11] in 2000 in hospitals in Isfahan, two methods of grafting were compared. The success rate of the two groups was 92% and 90% respectively, and there was no significant difference between the two groups. In the study, the mean hearing threshold in the graft on the anulous was more favorable than the graft below the anulous [12]. In a study by Morb et al. [12] in 2009, the success rate of grafting on overlay technique was more favorable in the study of Glasscock et al. [13] it was 91% and 96%, respectively, and there was no significant difference between the two methods.
At the same time, in the study by Doyle et al. [14] the success rate of the two methods was reported 64% and 86%, respectively, and the overlay graft method was significantly more successful. Regarding the similarity in two ways, it seems that the greater success rate in overlay grafting is related to the surgeon’s skill. In the study by Rizer, graft success was 95.6% and 88.8%, respectively, for the two groups, which was the cause of higher success rates in the overlay method by the incision of the back of the ear and the complete anterior flap and accurate graft placement. At the same time, it seems that in addition to the surgeon’s skill to use both methods, other factors such as access to the tympanic perforation, the degree of visibility and the probability of infection in the two methods are different, and they all can affect the accuracy of grafting. On the other hand, the overlay graft seems to take shorter time, which will also affect the postoperative side effects.
According to the results of our study, tinnitus was a common complication in patients. In the first study, more than half of the patients complained of tinnitus (54.8% of the underlay graft and 48.4% of the overlay graft) On the other hand, 6 months after operation, 38.7% of the underlay subjects and 45.2% of the overlay group complained of tinnitus. In other words, tympanic membrane recovery has not had a significant effect on the treatment of tinnitus in patients. The patients follow up to 6 months later showed that the recurrence rate in the underlay graft was 9.7% and 6.5% in the overlay graft group and the recurrence rate in the two groups did not differ significantly, but the incidence of total complications in all patients was 32.3% of whom the main complications were hearing loss, itching, pain, tinnitus and otorrhea. However, in most patients, the complications were minor, mainly due to pain and itching ears, and there was no need for medical intervention. In the study by Doyle et al. [14] the percentage of postoperative complications in both overlay and underlay groups was 10% and 38% respectively. It revealed recurrence of the disease in 5 patients (Pearl Cholesteatom and otorrhea and reinfection), including 3 of the underlay graft group and 2 of the overlay graft group, and there was no significant differences between the two groups. In a study by Rizer et al. [15], there was no recurrence in patients.
Conclusion
The results of this study showed that there is no difference in the success rate of the operation, recurrence of the disease and the incidence of complications in both methods of overlay and underlay grafting. However, the hearing improvement is relatively higher in the overlay graft group. Although the overlay graft is more difficult than the underlay graft, the method is healthier with more favorable auditory results if this technique is sufficiently precise.
Acknowledgment
The present article is the result of a Ph.D. thesis in the field of ENT, which was approved by the Deputy Chancellor of the Faculty of Medicine at No. 394123 with the support of the vice chairman. Therefore, the authors praise and appreciate their efforts.
References
- Paul W, Bruce H, Valerie j (2012) Cummings otolaryngology (6th edn), Elsevier corporation, Netherlands, pp. 2012-2177.
- Dornhoffer J (2003) Cartilage tympanoplasty: indications, techniques, and outcomes in a 1,000-patient series. Laryngoscope 113(11): 1844- 1856.
- Amedee RG, Mann WJ, Riechelmann H (1989) Cartilage palisade tympanoplasty. Am J Otol 10(6): 447-450.
- Duckert LG, Müller J, Makielski KH, Helms J (1995) Composite autograft “shield” reconstruction of remnant tympanic membranes. Otology & Neurotology 16(1): 21-26.
- Luetje CM (2001) Saddle blanket graft tympanoplasty and lateral attic wall reconstruction for defects produced by primary acquired cholesteatoma. Laryngoscope 111(8): 1497–1499.
- Page C, Charlet L, Struns V (2008) Cartilage tympanoplasty: Post operative functional results. Eur Arch Otorhinolaryngol 265(10): 1195- 1198.
- Ozbek C, Ciftci O, Ozdem C (2010) Long- term anatomic and functional results of cartilage tympanoplasty in atelectatic ears. Eur Arch Otorhinolaryngol 267(4): 507-513.
- Hsiao SH, Liu TC (2003) Osteoma of the external ear canal. Otol Neurotol 24: 960.
- www.springerlink.com
- Kirazli T, Bilgen C, Midilli R, Ogüt F (2005) Hearing results after primary cartilage tympanoplasty with island technique. Otolaryngol Head Neck Surg 132(6): 933-937.
- Amiridavan M, Soleimani SH (2000) Comparison of success and improvement of hearing in the two methods of underlay and overlay graft of tympanoplasty. Thesis for obtaining of MD degree of ENT specially, medical school of Isfahan University of Medical Sciences, Iran.
- Murbe D, Zahnert T, Bornitz M, Huttenbrink KB (2009) Acoustic properties of different cartilage reconstruction techniques of the tympanic membrane. Laryngoscope 112(10): 1769-1776.
- Glasscock ME (2003) Tympanic memberance grafting with facia overly vs undersurface technique. Laryngoscope 83(5): 754-770.
- Doyle JP, Schleuring AJ (1992) Typmanoplasty: should grafts be placed medial or lateral to tympanic memberance. Laryngoscope 82(8): 1425- 1430.
- Rizer FM (2007) Overly versus underlay tympanoplasty part II: the study. Laryngoscope 107(12): 26-36.
© 2018 Shahpour Kouhpaei. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






