- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
Analytical Study on Deep Neck Space Infections
Arun O* and George MV
Department of ENT, Jubilee Mission Medical College, India
*Corresponding author: Arun O, Department of ENT, Jubilee Mission Medical College, India
Submission: June 08, 2018;Published: July 19, 2018

ISSN: 2637-7780Volume2 Issue1
Abstract
This study was performed Department of Otor hinolaryngology, Jubilee Mission Medical College, thrissur, Kerala for a period of 2 years commencing from December 2012 to November 2014. To review our experience with deep neck space infections and to study changing trends. The objectives were to study clinical presentation, etiology, associated systemic diseases, bacteriology, radiology, management and outcome of deep neck space infections.40 Patients coming from both urban and rural areas irrespective of age and sex admitted in department of ENT with deep neck space infections which was confirmed either clinically or radiologically. Superficial skin abscesses and abscesses due to infections of external neck injuries were excluded from the study \r\n.
Result: \r\the commonest infections leading to deep neck infection were dental infections and tonsillitis. Commonest symptom was pain odynophagia/dysphagia. Bacteria most often isolated were staphylococcus aureus. Gram negative organisms like klebsiella and pseudomonas were also isola ted. One of our patients underwent tracheostomy. Complications were seen in 12.5% of cases of which 2 patients died.\r\n.
Conclusion: \r\nThe deep neck space infection is still a challenging disease in otolaryngology. Its presentation may be masked and bacterial culture might not be conclusive but it still needs early diagnosis and prompt management either conservative or surgical. Most of our patients needed surgical intervention, especially the pediatric cases. Early surgical intervention can reduce the complications. Tracheotomy should be considered if air way protection is needed\r\n
Keywords: Deep neck space infection; Peritonsillar abscess; Retropharyngeal abscess; Diagnosis; Surgical management
Background
Deep neck infections are frequently accompanied with localized aerodigestive tract compromise and sometimes by life threatening sequelae like severe airway obstruction, mediastinitis, pericarditis, internal jugular vein thrombosis and carotid artery erosion [1]. Failure to recognize deep neck space infections (DNSI) early may be due to an altered clinical practice resulting from the misuse of antibiotics, increasing prevalence of patients with immunodeficiency and changes in the origins of deep neck space infections and its bacteriology.
Dental infections and regional trauma are now more common causes of deep neck infections. Clinical examination alone seems to underestimate the extent of disease in 70% of cases, appropriate radiological imaging can reveal infection spreading between the spaces [2]. Decision making between conservative versus surgical management are very important in the management of DNSI.
Methods
Source of Data
Primary source of information method was used on the patients admitted in the Department of Otorhinolaryngology with clinically diagnosed cases of deep neck space infections in Jubilee Mission Medical College, Thrissur, Kerala, which is a 1800 bedded tertiary care hospital providing medical services to mixed population of 3 districts. The study was conducted for a period of 2 years commencing from December 2012 to November 2014.
Method of Data Collection
Primary source data collected from a specially designed case recording proforma pertaining to the selected patients. Prior to selection, they had to undergo routine history taking, physical examination and investigations. Informed written consent and Ethical committee approval were taken prior to the study. Follow up of the patients during hospital stay were done.
Sample Size
We included 40 cases of deep neck space infections admitted in our department during this study period.
Design of Study
Prospective study design
Inclusion Criteria
Only clinically or radio logically confirmed cases of deep neck space infections of all age groups and both sexes were included in the study.
Exclusion Criteria
Superficial skin abscesses, abscesses due to infections of the external neck wounds (surgical / traumatic) were excluded from the study. Each patient detailed history was taken followed by detailed general and local examination to determine the extent and cause of the deep neck space infections. They were subjected to baseline investigations. It includes hemoglobin, TC, DC, ESR, Random Blood Sugar, urea/creatinine, urine- albumin, sugar, and microscopy. In cases where clinical diagnosis was uncertain, radiological investigations were done to confirm the diagnosis.
Needle aspiration or incision and drainage (I&D) was done at the earliest stage in majority of the patients, pus was sent for culture and sensitivity analysis. All patients were initially started on a combination of third generation cephalosporin and metronidazole. The antibiotics were modified based on culture sensitivity reports or clinical unresponsiveness. Supportive therapy, in the form of intravenous fluid, analgesics, antipyretics, mouth washes etc. were given. Descriptive and inferential statistical analysis has been carried out in the present study.
Result
It was observed that the maximum number of cases was seen in the age group of 40-50 years (22.5%). Youngest patient seen was 45 days old and the oldest patient was 70 years old. Among 40 patients, 32 (80%) patients were adults and 8 patients (20%) were among pediatric age group (≤12 years). 18 (45%) were male and 22 (55%) were female. 33 (82.5%) patients belong to low socioeconomic status. The most common symptom with which the patients presented was odynophagia/dysphagia (38 patients 95%) followed by fever (34 patients 85%), pain in throat (27 patients 67.5%), neck Swelling (27 patients 67.5%), halitosis (21 patients, 52.5%), difficulty in opening the mouth (20 patients 50%) and difficulty in breathing (7 patients, 17.5%).10 patients (25%) had history of DM and were on irregular treatment. 6 patients (15%) were on treatment for HTN and 2 patients(5%) had history of seizure disorder, on treatment. 4 patients (10%) had history of foreign body ingestion, following which symptoms started. On removal of foreign body and subsequent antibiotic treatment, symptoms relieved.
Most common clinical finding was fever among 34 patients (85%) followed by neck swelling 23 patients (57.5%) and lymphadenopathy 23 patients (57.5%). Etiology was unknown in 15 patients (37.5%), dental infections in 12 patients (30%) and tonsillitis in 6 patients (15%). Most common infection was peritonsillar abscess (12 patients-26%) and retropharyngeal abscess (12 patients-26%) followed by parotid abscess (9patients- 20%), parapharyngeal abscess (5 patients-11%), Ludwig’s angina (4 patients- 9%), submandibular abscess (2 patients-4%). Masticator abscess (2 patients-4%). Peritonsillar abscess occurred in 12 patients (26%) and it didn’t progress to other neck spaces. In 32 patients (80%) single space was involved. In 8 patients (20%) more than one space was involved, of these 3 patients (7.5%) had Ludwig’s angina.
As clinical diagnosis was certain in 12 cases (30%) and patients improved symptomatically, no radiological investigation was carried out. In the remaining 28 cases (70%), diagnosis was confirmed radio logically. Ultrasound was done in 16 cases (40%), CT scans (20%), x-rays were taken for 4 patients (10%). Thus out of the 28 cases where radiological investigations are done, 16 cases ( 40%) diagnosed with USG itself. I &D of the abscess done in 22 patients (55%), needle aspiration 8 patients(20%), both Needle aspiration and I & D in 4 patients( 10%) and conservative treatment with intravenous antibiotics in 6 patients(15%).
In 36 out of 40 cases where there was no airway obstruction, no death happened and out of 4 cases where there was airway obstruction, 2 patients died. P value = 0.00013 which shows statistically significance. In pediatric cases where 8 (100%) out of 8 (20%) were treated with non conservative (surgical) methods. In adults out of 32(80%); 26 (81.25) treated with surgical methods and were 6 (18.75%) treated with conservative methods; The P value = 0.184 which was not statistically significant (Table1). Surgical Vs Non surgical treatment
Table 1: Surgical Vs Non surgical treatment.
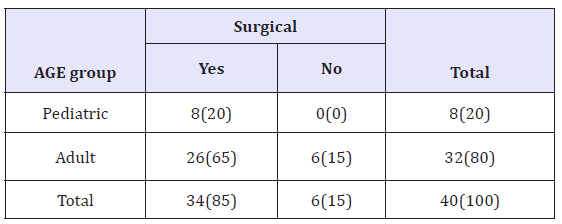
figure 1: Pus being taken for culture and sensitivity in patient with submandibular abscess.
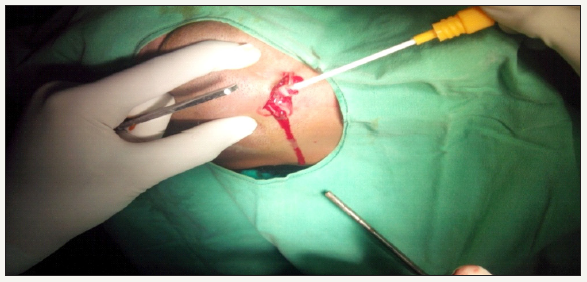
Pus was sent for culture and sensitivity in 40 patients (Figure 1). It was sterile in 16 samples (40%).Organisms were isolated in 24 samples (60%). Culture yielded growth of polymicrobial organisms in 1 sample (2.5%). Due to the unavailability of the facilities in our settings, anaerobic culture was not done.
Most people spent 1-5 days in hospital, minimum duration was 1 day. That patient came with breathing difficulty and sepsis and died within few hours itself. Maximum duration of hospital stay was 19 days. That patient was admitted with parotid abscess and Ludwig’s angina. Symptoms relieved at discharge. Average duration of hospital stay was 6.78 ± 3.9 days.
Discussion
Spaces Involving the Entire Length of Neck
- Anterior visceral (pretracheal or previsceral) space. It is the anterior portion of the visceral compartment that surrounds the trachea, is located against the anterior wall of the oesophagus, its superior limit is the hyoid bone.
- Posterior visceral (retropharyngeal, retrovisceral or retroesophageal space). It lies anterior to the alar fascia. This space extends from the skull base to the tracheal bifurcation (T1), where the alar fascia fuses with the middle layer of deep cervical fascia.
- Prevertebral space. It lies immediately anterior to the spinal column and the anterior longitudinal ligament. It is bounded anteriorly by the prevertebral layer of the deep layer of the cervical fascia and it extends from the base of skull to coccyx.
- Danger Space
- Suprahyoid Spaces. Submandibular space2. Peritonsillar Space3. Parotid Space4. Lateral pharyngeal space (peripharyngeal, parapharyngeal,pterygopharyngeal,pterygomandibular, pharyngomaxillary space)
- Infrahyoid spaces
- Pretracheal (anterior visceral) space
- Suprasternal space Of Burns
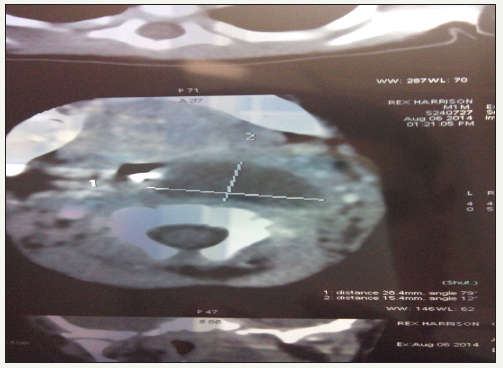
In our study the youngest patient was 45 days old child presented with retropharyngeal abscess and oldest was 70 year old male presented with parotid abscess. 45 days old child presented with stridor, prompt diagnosis of retropharyngeal abscess made with the help of CT scan Figure 2. hild improved after I&D of the abscess.
figure 2: CT scan of 45 days old child showing retropharyngeal abscess.
Clinical Presentation
The most common presenting complaints in our series was odynophagia/dysphagia. This was followed by fever, throat pain and neck swelling. DS Sethi, P. Kamath and Gino Marioni studies have also shown odynophagia, neck swelling and fever to be the commonest presenting complaints [2-4].
Associated systemic disease
In our series of 40 patients, 10 patients had diabetes mellitus (DM) and were on irregular treatment. Out of the two patients who died due to DNSIs, one had both DM and hypertension (HTN) on irregular treatment; other patient had DM and seizure disorder.
Etiology of Deep Neck Infections
Previously established risk factors for DNSIs included peritonsillar infections, upper respiratory tract infections, poor oral health, odontogenic infections, intravenous drug use or other substance abuse, immunocompromised states, and diabetes [5]. More recent trends have demonstrated an overall increase in the prevalence of causes related to odontogenic infection [4].
In our study, in majority of the cases, etiology was unknown followed by dental infections and tonsillitis. This could be a result of the infections being caused by more virulent bacteria, which may be more resistant to standard dental practices. Secondly, the patient population may have reflected a cohort less likely to present to a health practitioner at an earlier stage of infection. Tonsillar infections could be a result of an increased bacterial load harbored within the tonsillar crypts. Presence of foreign body was identified in 10% of the patients. In our study, a 19 yr old girl admitted with odynophagia, on examination diagnosed to have peritonsillar abscess. Further blood evaluation revealed WBC counts above 1 lakh and peripheral smear examination showed the presence of leukemia.
Location of Deep Neck Space Infection
In our study, most common infection was retropharyngeal abscess (26%) and peritonsillar abscess (26%) followed by parotid abscess (20%) and parapharyngeal abscess (11%).
Bacteriological study
In our study culture was negative in 16 cases (40%), it may be because of improper use of antibiotics prior to presenting to our centre. Staph. aureus was the most commonly isolated organism (22.5%), followed by beta hemolytic streptococci (12.5%) and klebsiella (10%). The organisms isolated were similar across the different weight percentile groups Coticchia et al. [6]. Reported that the organisms isolated from an anterior or posterior triangle abscesses (35%) and submandibular abscess (42%) were mostly S. aureus. Similarly, Dodds and Maniglia [7] noted that the most commonly isolated organism was S. aureus in their study. Most of the organisms isolated in our study showed good susceptibility to cephalosporins, amoxicillin+ clavulinic acid, ciprofloxacin, gentamycin and amikacin.
Management
I &D of the abscess done in 22 patients, needle aspiration 8 patients, both needle aspiration and I & D in 4 patients. Studies comparing needle aspiration and incision drainage in the treatment of peritonsillar abscess have shown no statistical significance John et al. [8]. In their study concluded that a trial of intravenous antibiotic therapy could be considered before immediate surgical intervention is performed in patients who are clinically stable [9]. Nagy et al also considered medical line of treatment as the first line of management especially in those with abscess volumes estimated to be less than 2000mm and if no clinical improvement occurs after 24 to 48 hrs, surgical exploration may be indicated [10].
In our study early surgical intervention was the mainstay of treatment.
Complications
Complications developed in 5 patients( 12.5%) of which 4 patients (10%) developed airway obstruction, 2 patients( 5%) died and 1 patient( 2.5%) developed mediastinitis. Death in both the cases was due to respiratory obstruction due to delayed presentation and unwillingness of the patients to undergo tracheotomy. One patient with airway obstruction who was diagnosed to have Ludwig’s angina underwent tracheostomy + I&D and symptoms relieved afterwards.
Radiological Investigations
In 28 cases (70%), diagnosis was confirmed radiologically. Ultrasound was used in 16 cases (40%), CT scan (20%), x-rays were taken for 4 patients( 10%) In rural setting like ours where all patients cannot afford contrast enhanced CT(CECT), ultrasound can be used effectively in cases like Ludwig’s and submandibular abscess. CECT is currently considered the radiologic investigation of choice in deep neck infections. In cases where parapharyngeal and retropharyngeal abscess are suspected CECT not only helps in diagnosis but also helps in identifying impending airway complications before they are clinically detectable, thereby reducing the complications.
Miller et al have concluded in their study that CECT has a high sensitivity and low specificity, which may lead to needless surgery for some patients if used in isolation. Clinical examination and CECT together are the most accurate test to determine the extent of DNSI [11]. There are recent reports of successfully treating small abscesses (< 2000mm on CECT) with intravenous antibiotics alone [12].
Length of Hospital Stay
In terms of length of hospital stay, this study demonstrated that presentation with airway compromise, mediastinitis and diabetes are associated with a prolonged course in hospital, as is consistent with the findings of previous studies [13]. Maximum hospital stay was for 19 days (patient with Ludwig’s angina/DM/HTN) followed by 17 days (patient who developed mediastinitis following retropharyngeal abscess subsequent to accidental foreign body ingestion)
Socio Economic Status
In our study, 33 out of 40 (82.5%) belong to low socio economic status according to the revised Kuppuswamy scale [14]. Lack of awareness of complications and poor health seeking behavior with low literacy rates are responsible for these cases, measures directed towards these issues should be initiated and continued for the prevention of DNSIs.
Conclusion
Our study revealed that deep neck space infections are common in female in the age group 40-50 years. Majority presented with complaints of odynophagia/dysphagia. Etiology found to be dental infections and tonsillitis. Most common infections are peritonsillar abscess and retropharyngeal abscess. Radiological investigations were required in 28 patients. Surgical interventions were done in 34 patients. Staphylococcus aureus isolated in 10 cases, which were 100% sensitive to ciprofloxacin. 2 patients died following respiratory obstruction. Complications were more in patients having systemic disease. Early surgical intervention is important to reduce complications..
Recommendations
- Foreign bodies in the throat are to be removed without delay especially in patients having systemic diseases, also chronic tonsillitis have to be treated without much delay.
- Dental infections are still a major factor in deep neck space infections. Proper oral hygiene can prevent these infections up to a certain extent.
- CECT is essential in appropriate management of deep neck infections especially in those involving parapharayngeal and retropharyngeal spaces. Needle aspiration in the treatment of peritonsillar abscess is successful and cost effective.
- Antibiotic coverage should include gram negative, gram positive and anaerobic micro organisms. A combination of third generation cephalosporins and metronidazole are given as empiric antibiotic coverage.
Health education in rural areas can make people aware of complications of deep neck space infections and need for seeking treatment in time. Early diagnosis, aggressive management with surgical intervention and proper airway management decrease the complications and mortality associated with deep neck abscesses.
References
- Jain S, Kumar S, Kumar N, Puttewar MP, Nagpure PS (2008) Deep neck space infections-a diagnostic Dilemma. Indian J Otolaryngol Head and Neck Surg 60(4): 349-352.
- Marioni G, Staffieri A,Parisi S, Ragona RM, Zuccon A, et al. (2010) Rational diagnostic and therapeutic management of deep neck infections; Analysis of 233consecutive cases. Ann OtolRhinolLarngol 119(3): 181-187.
- Shumrick KA, Stanley AS (2018) Deep Neck infections. In: Paperella, Shumrick, Gluckman, Meyerhoff (Eds.), Chapter 43 Otolaryngology Head and Neck (3rd edn), W.B. Saunders Company, USA
- Har El G, Aroesty JH, Shaha A, Lucente FE (1994) Changing trends in deep neck abscess: a retrospective study of 110 patients.Oral Surg Oral Med Oral Pathol77(5):446 450.
- Weed HG, Forest LA (2005) Deep neck infection. In: Cummings C, Flint P, Harker L, Richardson M, Robbins T, Schuller D, et al, (Eds.), Oto laryngology head and neck surgery, PA: Mosby, Philadelphia, USA, pp. 2515-2524.
- Coticchia JM, Getnick GS, Yun RD, Arnold JE (2004) Age-, site-, and timespecific differences in pediatric deep neck abscesses. Arch Otolaryngol Head Neck Surg130(2): 201-207.
- Dodds B, Maniglia AJ (1988) Peritonsillar and neck abscesses in the pediatric age group. Laryngoscope98(9): 956-959.
- Jennings CR (2008) Surgical Anatomy of the neck, In: Scott Brown (Ed.), Otorhinolaryngology, Head and Neck Surgery, (7thedn), Volume 2, UK Butterworth and Co, UK, pp. 1739-1753.
- McClay JE, Murray AD, Booth T (2003) Intravenous antibiotic therapy for deep neck abscesses defined by computed tomography. Arch Otolaryngol Head and Neck Surg 129(11): 1207-1212.
- Nagy M, Pizzuto M, Backstrom J, Brodsky L (1997) Deep neck infections in children: A new approach to diagnosis and treatment. The Laryngoscope107(12 Pt 1): 1627-1634
- Miller WD, Sandor GKB, Furst JM, Keller A (1999) A prospective blinded comparison of clinical examination and computed tomography in Deep Neck Infections. The Laryngoscope109(11): 1873-1880.
- Nagy M, Backstrom J (1999) Comparison of the sensitivity of lateral neck radiographs and computed tomography scanning in pediatric deep-neck infections. The Laryngoscope109(5): 775-779.
- Boscolo RP, Marchiori C, Zanetti F, Vaglia A, Da Mosto MC (2006) Conservative management of deep neck abscesses in adults: the importance of CECT findings. Otolaryngol Head Neck Surg 135(6): 894- 899.
- Mishra D, Singh HP (2003)Kuppuswamy’s socioeconomic status scale-a revision. Indian J Pediatr 70(3): 273-274.
© 2018 Arun O. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






