- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
The Utility of the Bird’s Eye View in Rhinoplasty
Anil R Shah*
Department of Otolaryngology-Head and Neck Surgery, New York University School of Medicine, USA
*Corresponding author: Anil R Shah, Department of Otolaryngology-Head and Neck Surgery, New York University School of Medicine, 845 North Michigan Avenue, Suite 934E, Chicago, IL 60611, USA
Submission: April 27, 2018; Published: June 15, 2018

ISSN 2637-7780 Volume1 Issue5
Abstract
Objectives: To examine the utility of the bird’s eye view in its use of preoperative rhinoplasty photographic analysis. The nose is a 3 dimensional object and therefore it stands to reason that viewing the nose from an additional angle would both assist in analyzing the deviation of the nose as well as in patient education.
Methods: A survey consisting of twelve patients’ preoperative photos were chosen randomly. Both frontal and bird’s eye views were randomized into a survey which was sent to the Otolaryngology department members (faculty and residents) in order to rate the deviation of the upper, middle and lower third of the nose. 14 responses were obtained. The average ratings of the nose were then compared to measured levels of deviation which were obtained via Adobe Photoshop. These values were placed into scatter plots to obtain R² values.
Results: The R² value for the frontal view photos was 0.1897, whereas the R² value for the bird’s eye view photos was 0.3341. This demonstrated that the bird’s eye view photographs allowed viewers to more accurately assess and rate the level of deviation of the nose.
Discussion: This study demonstrates the utility of adding the bird’s eye view photo to the standard views for preoperative rhinoplasty nasal analysis. It assists the physician in more accurately assessing the deviation of the nose. The authors believe that adding this view assists with patient education and communication in a more cost-effective way than 3D imaging, computer generated images, etc. Photographs serve several important roles in rhinoplasty including the ability to document changes in the nose, help in planning surgery, and facilitate in accurately depicting the shape of the nose. Most rhinoplasty surgeons use standardized views to accomplish these goals. These standard views include a frontal view, right/left oblique views, right/left lateral views, and a base view [1].
It has been the senior author’s experience that an additional view can add additional information in more accurately depicting the nose. The nose is a three dimensional object, therefore it would stand to reason that viewing the nose from another angle may help provide a more complete picture of it and enhance subtle nuances which could be otherwise missed without it. We propose an additional view for use in rhinoplasty, which we term the bird’s eye view. This view, which depicts the top of the nose looking down, has been named such since it is a complimentary view to the base view, otherwise known as the worm’s eye view. It offers several advantages, including enhanced understanding of asal deviation and fracture, improved preoperative planning, and assistance with patient education and communication.
Technical Aspects of the Bird’s Eye View
Figure 1:
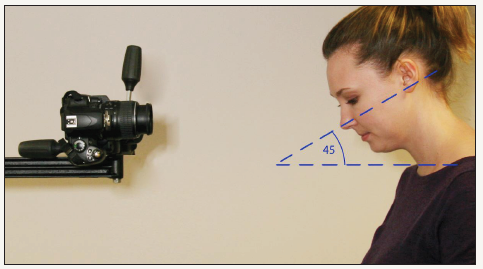
Photographic documentation in a standardized manner is an essential part of pre-operative planning for rhinoplasty. Each of the standard views is photographed accurately, with careful attention to patient positioning. [2,3] The bird’s eye view should be photographed with the same diligence, including a consistent photographer, the same camera, studio, lighting and settings, for before and after photographs. [4] The technical method of photographing the bird’s eye view is described below and seen in Figure 1 & 2.
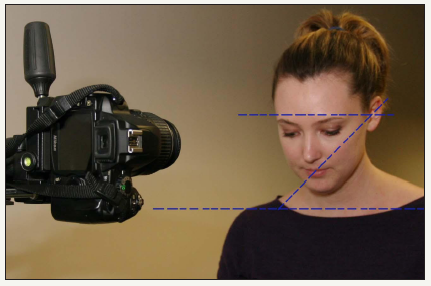
Figure 2:
A. Determine the Frankfort horizontal line. Place patient head at a 45 degree angle from floor using the Frankfort horizontal line.
B. Ensure the nose is kept in focus.
C. Ensure the external auditory canals are aligned and remain parallel to the floor
Methods
12 patients were randomly selected from the surgeon’s extensive database of preoperative rhinoplasty photographs. All of these patients had previously signed written consent for their photographs to be used in educational studies. The frontal and bird’s eye view photos of each of these 12 patients were then placed into random order in a 24 question survey. The frontal view was chosen as a comparison as this is the standard view used to currently assess nasal deviation. The survey was sent out to 9 faculty members and 12 residents in the Otolaryngology Head & Neck department at the University of Chicago. 13 total responses were obtained. These physicians were asked to rate the degree of deviation seen in each photograph in the upper, middle and lower third of the nose on a scale of -5 to +5, with 0 equaling midline.
The photographs were analyzed using Adobe Photoshop. A central line was created to divide the nose into vertical halves. The line was created from measuring midline between the brows down to the midline of the vermilion border Figure 2. Measurements were then taken to determine the degree of deviation. This was accomplished by using the measuring tool in Adobe Photoshop, and measurements were taken on either side of the central line at the level of the medial canthi, the widest point of the nasal ala and then midline between the two. The lateral border of the nose was determined by the shadow line. The ratio of deviation was then calculated and a scale was designed to correlate with the survey based on the ratio of deviation. See Table 1 to view it.
Table 1:

Results
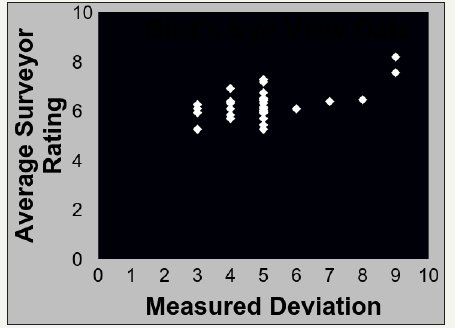
Data from the frontal view photos was placed into a scatter plot in order to compare the measured deviation to the average rating of deviation, see Figure 3. The same was then done for the bird’s eye view data, see Figure 4. A regression analysis was performed in order to determine how accurate the subjects were in rating the deviation. The R² value for the frontal view data is 0.1897, which indicates a positive correlation between the measured and rated deviation. The bird’s eye view data demonstrated in Figure 4 demonstrates an R² value of 0.3341. This is a nearly 3 fold increase in the R² value from the frontal view data vs. the bird’s eye view data. This demonstrates that subjects were more accurate in their rating of deviation when looking at the Bird’s Eye View photos as was predicted.
Figure 3:Frontal view data with linear regression.
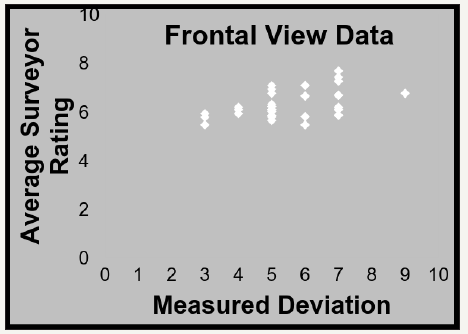
Figure 4:Birds eye view data w/ linear regression
Discussion
Photographic documentation is essential for patient consultation, perioperative planning, and postsurgical evaluation. Standardization of this photography, with goals of consistency and reproducibility, has been studied and validated [5,6]. However, there still exists a role for evaluating extended photographic views, as they may enhance the surgeon’s operative abilities.
The authors feel they are several advantages of incorporating the bird’s eye view into the standard six views currently used in rhinoplasty. First of all, the assessment of nasal deviation is facilitated by this view which is demonstrated by the survey results. Surgeons are better able to see and differentiate between deviation of the bone compared to the middle vault or nasal tip. This is quite significant since the treatment for each is distinct [7]. Furthermore, additional information such as the type of nasal fracture, if one exists, can be analyzed. For example, in a nasal fracture either the entire nasal bone pyramidal structure could be deviated to one side, which may require fracture of the perpendicular plate of the ethmoid. However, in some cases of nasal fracture, the pyramid of the nasal bone is intact except for collapse of a single nasal bone [8]. Although deviation can be seen on frontal view, often times it requires asymmetric lighting to reveal differences in shadowing to reveal deviation. Even then, significant deviation of the nose may look less impressive in photographs than reality. The utilization of the bird’s eye view may enhance the surgeon’s ability to analyze nasal deviation and nasal fracture.
The bird’s eye view can be helpful in the planning stages of the rhinoplasty procedure. In certain situations, patients may require the use of a caudal extension graft to extend the nose which is typically used for structural support or for cosmesis in a foreshortened nose. The senior author has also found utility in using such grafts to help achieve straightening when used appropriately in patients with deviation due to a length discrepancy from one side to the other. For example, if a nose is slightly deviated to the left, a caudal extension graft can be placed on the patient’s right side in select cases to place the nose back in the midline [9]. Utilization of the bird’s eye view preoperatively can assist in the planning of this technique.
The authors have also found this view to be helpful in educating patients about the deviation of the external appearance of the nose. Studies have demonstrated a clear benefit in the use of photographs and computerized models in patient education and expectations [10,11]. In certain cases, even in a significantly deviated nose, the only view which demonstrates deviation clearly can be the bird’s eye view. This view can also be helpful for documentation for insurance preauthorization purposes as well, which are often reviewed by practitioners who may benefit from clearer demonstration of a nasal fracture and deviation of the nose [12]. Although patients were not surveyed in this study the authors anticipate that the results of a survey in a patient population would likely yield similar results. Another merit of this view is for intraoperative assessment of the nose. During a rhinoplasty procedure, the surgeon will often look at the patient from the top of the bed down, effectively mimicking this view. However, if this view is not captured preoperatively, it can be difficult to determine deviation and asymmetry with subsequent swelling in the nose [13].
Although the authors believe this view would be a valuable addition to the standard views, there are some limitations. While this view has merit in preoperative planning and intraoperative use, its use in postoperative photographs is restricted [14]. The most important views to improve are the frontal, oblique and profile view, as these are most representative of how the patient will be viewed. The base view is seen the least in person, and the bird’s eye view would have even less real life benefits. In addition, this view is perhaps the most challenging view to correct [15]. Despite the strength of data implying the utility of the bird’s eye view, one limitation of the study was the small number of physicians which participated in the survey. It would be of great interest to the authors to see if the utility remained as high if a larger number of physicians were to complete the survey. This could warrant pursuing a larger study in the future.
Another limitation of the study was that although the photographs were chosen randomly from the database of photographs they were not randomized based on their level of deviation. It would be interesting to see the accuracy of raters on a wider variety of photographs with a specifically designated range of deviation [16]. It stands to reason that the degree of deviation would be easier to appreciate in the bird’s eye view in patients with a large degree of deviation or a significant degree of asymmetry. Therefore, if in this study by random the patients selected had large degree of deviations it may have over-emphasized the utility of the bird’s eye view [17]. Further investigation may be warranted in relation to the skyline view or “cephalic” view, as this photograph shares a similar goal of demonstrating asymmetry and deviation of the nose, although differ in their execution. The skyline view is captured from above with the head of the patient tilted backward. The authors believe this view to be technically more challenging and therefore believe the bird’s eye view to be more practical a view to capture. In the future, however, the authors would consider comparing the utility of the bird’s eye view versus the previously described skyline view [18].
In summary, the bird’s eye view is introduced as an additional view which has been proven to be helpful in eliciting subtle nasal deformities and deviation, and is also thought to be helpful in preoperative planning, as well as patient counseling.
References
- Kontis T (2002) Photography in facial plastic surgery. Papel I (Ed.), Facial plastic and reconstructive surgery. Thieme Medical Publishers, Germany, p. 119-120.
- Tardy ME, Dayan S, Hecht D (2002) Preoperative rhinoplasty: evaluation and analysis. Otolaryngol Clin North Am 35(1): 1-27.
- Thomas JR, Tardy ME, Przekop H (1980) Uniform photographic documentation in facial plastic surgery. Otolaryngol Clin North Am 13(2): 367-381.
- Shah AR, Dayan SH, Hamilton GS (2005) Pitfalls of photography for facial resurfacing and rejuvenation procedures. Facial Plast Surg 21(2): 154- 161.
- Swany R, Sykes J, Most S (2010) Principles of photography in rhinoplasty for the digital photographer. Clin Plastic Surg 37(2): 213-221.
- Schwartz MS, Tardy ME (1990) Standardized photodocumentation in facial plastic surgery. Facial Plast Surg 7(1): 1-12.
- Haack J, Papel I (2009) Caudal septal deviation. Otolaryngol Clin North Am 42(3): 427-436.
- Chaaban M, Shah AR (2009) Open septoplasty: indications and treatment. Otolaryngol Clin North Am 42(3): 513-519.
- Toriumi DM (2006) New concepts in nasal tip contouring. Arch Facial Plast Surg 8(3): 156-185.
- Muhlbauer W, Hold C (2005) Computer imaging and surgical reality in aesthetic rhinoplasty. Plast Reconstr Surg 115(7): 2098-2104.
- Agarwal A, Gracely E, Silver WE (2007) Realistic expectations: to morph or not to morph? Plast Reconstr Surg 119(4): 1343-1351.
- Sullivan M (2002) Rhinoplasty: Planning photo documentation and imaging. Aesthetic Plastic Surgery 1: S7.
- Jacobx JW, Schoenrock LD (1990) The sky-line view: a new perspective for rhinoplasty surgery. Fac Plast Surg 7(1): 13-17.
- Nayler JR (2003) Clinical photography: a guide for the clinician. J Postgrad Med 49(3): 256-262.
- Cingi C, Songu M, Bal C (2011) Outcomes research in rhinoplasty: body image and quality of life. Am J Rhinol Allergy 25(4): 263-267.
- Galdino GM, DaSilva And D, Gunter JP (2002) Digital photography for rhinoplasty. Plast Reconstr Surg 109(4): 1421-1434.
- Phillips PS, Stow N, Timerley DG, Sacks R, Srubiski A, et al. (2011) Functional and cosmetic outcomes of external approach septoplasty. Am J Rhinol Allergy 25(5): 351-357.
- Kang JM, Nam ME, Dhong HJ, Kim HY, Chung SK, et al. (2012) Modified mattress suturing technique for correcting the septal high dorsal deviation around the keystone area. Am J Rhinol Allergy 26(3): 227-232.
© 2018 Anil R Shah. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






