- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
Outcomes of Composite Chondroperichondrial Clip Tympanoplasty
Mohammad Abd Elazim, Mohammad Khalaf Alla, Magdy Bedir Ali, Said Abdelmonem, Ebtessam Hamed Nada* and SamahShehata Ali El Sayed
Department of Otolaryngology, Zagazig University, Egypt
*Corresponding author: Ebtessam Hamed Nada, Associate Professor of Audio-vestibular Medicine, Department of Otolaryngology, Faculty of Medicine, Zagazig University, Egypt
Submission: April 20, 2018; Published: May 11, 2018

ISSN 2637-7780 Volume1 Issue4
Objectives
Tympanoplasty is a procedure used to eradicate disease in the middle ear and to reconstruct the hearing mechanism. Assessment of the success rate and efficacy of the technique of composite chondroperichondrial clip tympanoplasty for repair of small and medium sized tympanic membrane perforations and to assess this graft and audio logical results of this technique in comparison to the traditional perichondrial/cartilage composite underlay graft technique was addressed.
Study design: A prospective randomized comparative clinically controlled study in patients with small or medium-sized perforation. 40 patients were included and divided into 2 groups.
a) Setting: Operating room in otolaryngology department and audiology unit, Zagazig University, Egypt.
b) Subjects and methods: 40 patients had their ears dry for a least 1 month before surgery without antibiotics. Age was above 12 years and sex included both males and females. All had their perforation located centrally in the TM in case of small perforation (occupy < 1/4th of the TM) and medium-sized perforation occupied < 1/2 of the TM. Patients with total or large perforation, marginal perforation, patients with sensorineural hearing loss (SNHL) or those with active infection or cholesteatoma were excluded from the study. Surgery was done under local anesthesia.
Results: Audio logical profile in the 2 groups was the same with adding easiness in the surgical technique and less intra-operative complications were notices.
Conclusion: The use of cartilage graft is feasible in achieving success in tympanoplasty
Keywords: Tympanic membrane; Csom; Tympanoplasty; Cartilage; Graft and air/bone gab
Introduction
Tympanoplasty is a procedure used to eradicate disease in the middle ear and to reconstruct the hearing mechanism. Repair of tympanic membrane perforation with most accepted technique reaches a success rate over 90%. The most frequently used techniques globally are underlay of temporalis fascia. However, the technique necessarily involves lifting of a tympanomeatal flap for fixation of the graft with its inherent tendency to provoke bleeding that sometimes impairs visualization and causes flap tears [1-3]. On the other hand, the use of cartilage for middle ear reconstruction is not new and cartilage as a graft has been advocated in cases with high risk of graft failure, like those with subtotal perforation.
It was reported that cartilage physically dampens the forced vibration of the tympanic membrane contributing to some impairment in functional results. In other study, cartilage was reported to be easier to manipulate and position than fascia and supplies both the scaffolding necessary during healing and subsequent support which prevents recurrence of perforation [4,5]. The aim of this work is to assess the success rate and efficacy of the technique of composite chondroperichondrial clip tympanoplasty for repair of small and medium-sized tympanic membrane perforations and to assess this graft and audio logical results of this technique compared to the traditional perichondrial/cartilage composite underlay graft technique.
Methods
A prospective randomized comparative clinically controlled study in patients with small or medium sized perforation. 40 patients were included and divided into 2 groups; group (I) which included 20 patients with small or medium-sized perforation who were subjected to composite chondroperichondrial clip tympanoplasty for repair of their perforation. And group (II) which consisted of 20 patients with small or medium-sized perforation who were operated using perichondrium/cartilage composite underlay grafts technique. All patients had their ears dry for a least 1 month before surgery without antibiotics. Age was above 12 years and sex included both males and females. All had their perforation located centrally in the TM in case of small perforation (occupy < 1/4th of the TM) and medium-sized perforation occupied < 1/2 of the TM. Patients with total or large perforation, marginal perforation, patients with sensor in neural hearing loss (SNHL) or those with active infection or cholesteatoma were excluded from the study.
Surgical technique
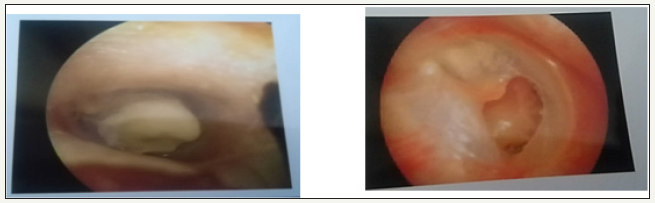
Operation is performed under local anesthesia with 2% xylocaine with 1:100,000 epinephrine. Preparation and sterilization of the relevant ear is performed. Margins of the perforation are freshened. The graft is taken from the concha (to avoid another incision and because conchal graft is thicker and more suitable for composite graft) by incision in the posterior aspect of the auricle over the concha and elevates the soft tissue to expose the conchal cartilage. The perichondrium is cut with same shape as the perforation (2mm larger) and the thickness is thinned out. The graft is then inserted in a trans canal fashion microscopically with cartilage medially and the perichondrium laterally to the edge of the perforation. Gel foam soaked in antibiotic solution is placed in the external auditory canal and post auricular incision is closed using 3/0 silk suture (Figure 1).
Figure 1: post and pre-operative TM perforation.
Statistical analysis
It is made using data collected in a master sheet and analyzed using EPI-INFO medical statistical software version 20. Data were presented as mean ± standard deviation foe quantitative variables and number and percentage for qualitative data [6-8].
Results
Study included 40 patients divided in to 20 patients each with age range from 13-36 years in group I and 15-36 years in group II. There was no statistically significant difference between 2 groups as regard the site or the size of perforation (Table 1). Success was estimated as “graft take” and healing at the follow up period of 6 months post-operative. Follow up included clinical examination by otoscope to assess graft take at 4 weeks, 3 months and 6 months, pure tone audiogram at 6 months. At 4 weeks postoperative success rate was 100% while at 6 months post-operative failure occurred because of infection or persistent association of other head and neck lesions such as sinusitis or Eustachian tube dysfunction (Table 2). Evaluation of hearing of patients in both groups’ pre and 6 months post-operative by pure tone audiometry revealed statistically non-significant difference between the 2 groups in pre and postoperative hearing loss. A highly statistically significant difference was found between pre and post-operative hearing reading of air/bone gap in both groups (Table 3).
Table 1:The clinical presentation of the 2 groups patients as regards side of perforation and size of the TM perforation showed no statistically significant differences.

Table 2Success rate in the 2 groups showed no statistically significant difference.

Table 3:The clinical presentation of the 2 groups patients as regards side of perforation and size of the TM perforation showed no statistically significant differences.

Discussion
In this study, the groups were chosen with no significant differences as regard the size and site of perforation and with history of dry ear for 1 month pre-operative without antibiotics. The first group was operated using the composite chondroperichondrial clip tympanoplasty for repair of their perforation while group (II) were operated using the traditional perichondrium/cartilage composite underlay grafts technique (Table 1). Success was estimated as “graft take” and healing at the follow up period of 6 months postoperative. Follow up included clinical examination by otoscope to assess graft take at 4 weeks, 3 months and 6 months, pure tone audiogram at 6 months. At 4 weeks post-operative success rate was 100% while at 6 months post-operative failure occurred because of infection or persistent association of other head and neck lesions such as sinusitis or Eustachian tube dysfunction. There was no statistically significant difference between 2 groups as regards success rate (Table 2). Graft failure has been attributed to infection. The anatomic success rate in this study may be related to the careful selection criteria used. However, a 100% success rate has also been obtained in other studies using cartilage and perichondrium. Postoperative infection caused minimal displacement of the graft which was overcome by adequate antibiotics for a period of 3 months with good results and restoring of healing mechanism. Evaluation of hearing of patients in both groups was done pre and 6 months post-operative by pure tone audiometry, air conduction and bone conduction thresholds were evaluated. A highly statistically significant difference was found between pre and post-operative hearing reading of air/bone gab in each group (Table 3) while statistically non-significant differences were found between the 2 groups either in the pre or the post-operative hearing thresholds’ evaluation. This is supported by a study that stated that the cartilage does not appear to interfere significantly with tympanic membrane vibration, and this may also depend on its size and placement from the umbo. Preservation of the shape of the post-operative air/bone curve implies no significant inner ear trauma during surgery. Similarly, Gerber et al. [9] reported acceptable results with cartilage techniques and comparisons with temporalis fascia and perichondrium only techniques have shown no significant differences in functional results. As a conclusion, the composite chondroperichondrial clip Tympanoplasty has produced 100% take rate just as the perichondrium/cartilage composite underlay technique with minimal invasion and no visible scar. In addition to the speed of the technique and less post-operative needed care with the feasibility of performing both ears in one session.
References
- Eavey RD (1998) Inlay tympanoplasty: Cartilage butterfly technique. Laryngoscope 108(5): 657-661.
- Jackson RP, Chlebicki C, Krasieva TB, Puria S (2008) Multi photon microcopy imaging of collagen fiber layers and orientation in the tympanic membrane. Proc of Spie pp. 1-7.
- Prescott CAJ (2006) Chronic Otitis Media (COM) - a personal philosophy. Int J ped Oto 70: 1317-1320
- Jansen C (1963) Cartilage-tympano plast. Laryngoscope 73(2): 1288- 1302.
- Aggarwal R, Saeed SR, Green KJ (2006) Myringoplasty. J Laryngo Otol 120(6): 429-432.
- Dornhoffer JL (1997) Hearing results with cartilage tympanoplasty. Laryngoscope 107(8): 1094-1099.
- Tos M, Tomsen J, Peitersen E (1989) Fascia or perichondrium/cartilage in tympanoplasties. A comparative study regarding hearing results and recurrence of perforations in 1529 cases. pp. 1113-1114.
- Adkins WY (1990) Composite autograft for tympanplasty and tympanomastoid surgery. Laryngoscope 100(3): 244-247.
- Gerberm MJ, Mason JC, Lambert PR (2000) Hearing results after primary cartilage tympanoplasty. Laryngoscope 110(12): 1994-1999.
© 2018 George MV. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






