- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
Management Outcomes of Post-Thyroidectomy Bilateral Recurrent Laryngeal Nerve Paralysis at National Hospital Abuja
Olusesi Abiodun Daud*, Opaluwah, Emmanuel, Oyeniran Olubukola and Oyeyipo Yemisi
Department of Ear, Nose & Throat, National Hospital, Nigeria
*Corresponding author: Olusesi Abiodun Daud, Department of Ear, Nose & Throat, National Hospital, Plot 132, Central Area, Garki, (Phase II), Abuja, FCT 900001, Nigeria
Submission: January 17, 2018;Published: January 31, 2018

ISSN: 2637-7780Volume1 Issue3
Abstract
Bilateral recurrent laryngeal paralysis is an uncommon complication of total or subtotal thyroidectomy, observed in approximately 0.4 per cent of cases. This paralysis could be temporary or permanent. An audit of 5 cases referred to the ENT Department of National Hospital Abuja, between January 2010 and July 2017 is presented. All cases were referred already on tracheostomy tubes and were females aged 11 to 59 years. 4 of the cases had external arytenoidectomy, bilateral in 2 cases, and unilateral in 2 cases. 4 out of the 5 cases were successfully decannulated. The preferred approach to cases of post-thyroidectomy bilateral recurrent laryngeal nerve paralysis referred to ENT Specialists in resource-poor economy like ours is not very clear from existing literature and we discuss our adopted protocol for management of such cases in this case series.
Keywords: Post-thyroidectomy; Recurrent laryngeal nerve palsy; Arytenoidectomy
Introduction
Bilateral recurrent laryngeal nerve (RLN) paralysis is an uncommon complication of thyroidectomy (seen in 0.4%), the commonest operation that places normally functioning laryngeal nerves at risk of injury [1,2]. Injury to the RLN could be temporary or permanent, unilateral or bilateral. Recent study showed that the likelihood of temporary RLN paralysis is higher in bilateral near total thyroidectomy compared to bilateral total thyroidectomy [3]. Bilateral RLN paralysis is a major risk factor for airway obstruction and dysphonia, and significant association exists between postthyroidectomy vocal paralysis and long term risks of hospital readmission, dysphagia, hospitalization for lower respiratory tract infection and tracheostomy/gastrostomy tube placement [1,3].
The overall effect of bilateral RLN paralysis is bilateral vocal fold paralysis (BVFP) clinically presenting as inspiratory dyspnoea (due to narrowing of the airway at the glottic level) and endoscopically with both vocal folds assuming a paramedian position [4].
The primary goals for management of BVFP is to relieve the distressing dyspnoea, and endotracheal intubation followed by tracheostomy are usually the first options. However, tracheostomy significantly affects the patient’s quality of life and tracheostomized patients are medically complex and highly vulnerable [5]. Endoscopic management of BVFP includes cordotomy and arytenoidectomy have become alternative options to tracheostomy [6]. In resourceconstrained settings like Africa, alternative cheaper options include external arytenoidectomy via lateral neck approach, or via laryngofissure. There is currently paucity of available literature on outcomes of post-thyroidectomy bilateral RLN paralysis in Africa managed by arytenoidectomy.
Methodology
This is a retrospective review of cases of post-thyroidectomy recurrent laryngeal nerve paralysis managed at the ENT department of National Hospital Abuja between May 2006 and April 2017. Cases were analyzed based on the type of thyroidectomy performed, the duration of RLN paralysis prior to presentation, the presence or absence of tracheostomy at presentation, the type of arytenoidectomy if any (whether unilateral or bilateral) and the approach (lateral neck or laryngofissure), the outcome including duration of post-arytenoidectomy tracheostomy, and duration of follow-up. All patients were given the options of initial attempted decanulation under inhalation anesthesia, after tube down-sizing, and only those that failed decanulation were offered surgery.
Results
A total of 5 cases were referred to the department during the study period. All were females, age ranged 11 to 59 years. One patient had bilateral total thyroidectomy for thyroid malignancy and the remaining 4 had bilateral near-total thyroidectomy for benign thyroid diseases. All thyroidectomies were carried out at private facilities and all had tracheostomy in place at time of presentation to National Hospital. Duration of RLN paralysis prior to presentation ranged from one week to 16 months. Table 1 shows the 5 cases managed based on age, surgery carried out prior to RLN paralysis, and duration at presentation.
Table 1:Age, Duration of presentation and Surgery carried out before presentation in 5 cases with bilateral vocal fold palsy.
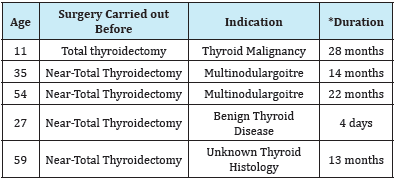
*Duration = time between the surgery leading to vocal fold paralysis and presentation at the hospital.
A total of 6 arytenoidectomies were performed. 2 patients had bilateral sequential arytenoidectomy and 2 patients had unilateral arytenoidectomy. One patient was successfully decannulated after a year on tracheostomy and did not require arytenoidectomy. Of the 6 arytenoidectomies, 4 were via lateral open approach and laryngofissure was employed in 2 cases. Arytenoidectomy was successful (patient successfully decannulated) in 3 of 4 cases-2 unilateral and one bilateral arytenoidectomies, and was not successful in one case (bilateral arytenoidectomy). The duration of RLN paralysis prior to surgical intervention ranged from 14 weeks to 4 years. Table 2 shows the relationship between outcome of intervention and duration of RLN paralysis.
Discussion
Unexpected bilateral vocal fold paralysis (BVCP) is a worrisome complication following thyroidectomy, and it often distresses the patient, his family and the healthcare personnel involved in the management [6]. It could be temporary or permanent. Temporary BVCP could be due to branching recurrent laryngeal nerve, endotracheal intubation, laryngeal mask anesthesia, and other risk factors including age above 50, and co-morbid hypertension or diabetes mellitus [6]. Our patient number 5, aged 59 years with a history of hypertension most likely had temporary BVCP.
Table 2: Duration of Vocal Fold Paralysis, Surgical Intervention and Outcomes in 5 patients with bilateral post-thyroidectomy abductor vocal fold palsy.
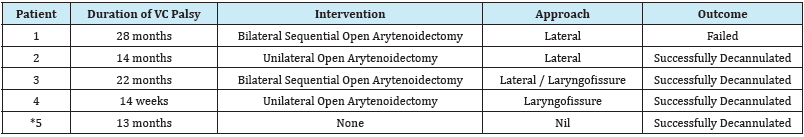
*Patient 5 had no surgical intervention, as she was successfully decanulated on the table, prior to carrying out arytenoidectomy.
Both temporary and permanent BVCP present as acute respiratory distress which could be noticed immediate following extubation or be delayed. Tracheostomy is often warranted as an emergency measure. All our cases in this series already had tracheostomy at presentation.
Tracheostomy however greatly influences patient’s quality of life. Definitive surgical options for BVCP that is not temporary include open arytenoidectomy, bilateral posterior cordectomy, laser arytenoidectomy with posterior cordectomy, and endolaryngeal suture laterofixation.
When confronted with BVCP, which is usually abductor paralysis, the challenge is to determine whether it is temporary or permanent and to determine the appropriate time for surgical intervention. Only one out of our series presented within 4 days of BVCP, and we have to observe watchful waiting for 14 weeks before surgical intervention. Chen et al. [7] recommended, based on review and meta analysis of available literature, that surgical intervention should be carried out after 12 months if no spontaneous recovery [7]. It has also been recommended that laryngeal electromyography data can be used to prognosticate recovery of vocal fold motion [8].
Since it was first popularized by Woodman [9], and subsequently popularized by Sessions, Ogura et al. [10], open arytenoidectomy has remained a reliable option for surgical treatment of bilateral abductor paralysis. Advances in endoscopic procedures and laser have resulted in wide adoption of endoscopic approach to management of BVCP. However open approach is still applicable in resource-constrained setting like ours, as shown in the current series. We employed the technique of Sessions, Ogura, and Heeneman of sequential arytenoidectomy, employing the second arytenoidectomy only if the first fails.
Only one of our cases failed bilateral arytenoidectomy. She was successfully decanulated initially after the second arytenoidectomy, but gradually became dyspneic after 4 days of decantation, and had to be re-intubated. We subsequently sent her to facility where laser equipments were available. Perhaps she is a candidate for laser cordectomy.
Summary
Our series of 5 cases of post-thyroidectomy bilateral vocal cord paralysis of abductor type showed the management outcomes employing open arytenoidectomy. Clinician should be on look-out for temporary palsy irrespective of duration of tracheostomy. The exact timing of intervention in permanent BVCP is not certain and patients often want the tracheostomy out at earliest possible time. We recommend at least 3 months of watchful waiting for cases presenting acutely.
References
- Cannizzaro MA, Lo Bianco S, Picardo MC, Provenzano D, Buffone A (2017) How to avoid and to manage post-operative complications in thyroid surgery. Updates Surg 69(2): 211-215.
- Nouraei SAR, Allen J, Kaddour H, Middleton SE, Aylin P, et al. (2017) Vocal palsy increases the risk of lower respiratory tract infection in low-risk, low-morbidity patients undergoing thyroidectomy for being disease: A big data analysis. Clin Otolaryngol 42(6): 1259-1266.
- Dinc T, Kayilioglu SI, Simsek B, Guldogan CE, Gulseren MO, et al. (2017) The evaluation of the complications observed in patients with bilateral total and bilateral near total thyroidectomy. Ann Ital Chir 88: 198-201.
- Li Y, Garret G, Zealear D (2017) Current treatment options for bilateral vocal fold paralysis: A state-of-the-art review. Clin Exp Otorhinolaryngol 10(3): 203-212
- Goff D (2017) Dysphagia management in tracheostomized patients: where are we now? Curr Opine Otolaryngol Head Neck Surg.
- Kikura M, Suzuki K, Itagaki T, Takada T, Sato S (2007) Age and comorbidity as risk factors for vocal cord paralysis associated with tracheal intubation. Br J Anaesth 98(4): 524-530.
- Chen X, Wan P, Yu Y, Li M, Xu Y, et al. (2014) Types and timing of therapy for vocal fold paresis/paralysis after thyroidectomy: a systematic review and meta-analysis. J Voice 28(6): 799-808.
- Guha K, Sabarigirish K, Singh SK, Yadav A (2014) Role of laryngeal electromyography in predicting recovery after vocal fold paralysis. Indian J Otolaryngol Head Neck Surg 66(4): 394-397.
- Woodman DG (1948) The open approach to arytenoidectomy for bilateral abductor paralysis, with a report of 23 cases. Ann Otol Rhinol Laryngol 57(3): 695-704.
- Sessions DG, Ogura JH, Heeneman H (1976) Surgical management of bilateral vocal cord paralysis. Laryngoscope 86(4): 559-566.
© 2018 Titas Kar. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






