- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
An Unusual Presentation of Squamous Cell Carcinoma of Bilateral Temporal Bones
Asok Kumar Saha, Titas Kar* and Nirmalya Roy
Department of ENT & Head Neck surgery, Medical College Kolkata, India
*Corresponding author: Titas Kar, Department of ENT & Head Neck surgery, Medical College Kolkata, India
Submission: January 17, 2018;Published: January 22, 2018

ISSN: 2637-7780Volume1 Issue2
Abstract
Squamous cell carcinoma of temporal bone is a rare entity, comprising of a very small percentage of all head neck tumours, mostly occurring in aged population. Bilateral presentation of tumours in both temporal bones is extremely rare and only a few cases have been reported. We report a case of bilateral squamous cell carcinoma of both temporal bones in a young adult male patient who presented very late.
Keywords: Squamous cell carcinoma; Bilateral; Temporal bone; External auditory canal
Introduction
Malignancies of the temporal bone are rare with an incidence of less than 0.2% amongst all head neck cancers [1]. Amongst them, most are squamous cell carcinoma of the external auditory canal. Despite advances in surgical and radiotherapeutic techniques, prognosis for patients with this disease has remained poor [2,3]. The median age at presentation of squamous cell carcinoma (SCC) of the temporal bone is in the seventh decade. Occasionally, SCC of the temporal bone can develop in younger adults and the possibility should not be ignored merely on the basis of age [4]. We report a case of SCC of both temporal bones in a 30 year old male patient, who presented very late with extensive disease in one ear, and so could be managed by palliative therapy only. Bilateral presentation of SCC in the external ear canal is an exceedingly rare presentation and a handful of them have been reported till date in literature. To the best of our knowledge, this is the 11th case of SCC of bilateral temporal bones in literature [5,6].
Case Report
Figure 1a & 1b

30 years old male patient presented to ENT OPD with complaints of bilateral foul smelling, painful, occasionally blood mixed ear discharge for the past three years, painful swelling on the right side of the face for the past six months, and deviation of the angle of the mouth on the right side for the past two weeks. There was a history of the patient undergoing some ear surgery about three years prior, but no documents pertaining to the surgery were found. He was a farmer by profession, and there was no prior history of any exposure to radiation. On examination, there was a large swelling on the right side of the face, about 8cm x 5cm in size, which was hard, tender, fixed to the lower structures and skin, with the overlying skin inflamed, and ulcerated at places. The ear lobule was displaced laterally by the swelling which involved the right parotid. There was also right sided Lower Motor Neurone type facial palsy, with incomplete closure of the eyes on maximum effort (Figure 1a & 1b). Mouth opening was restricted to one and a half fingers. He had no other neurodeficit. On otoscopy and otoendoscopy, both ear canals were occluded by reddish proliferative tissue that was extremely vascular and bled on touch. A dirty white discharge was also found to be smeared around the reddish masses (Figure 2). He complained of decreased hearing in both the ears, but pure tone audiometry was impossible as mere placement of the headphones over the mastoid resulted in severe pain. Rest of the systemic examination did not reveal any abnormality.
Figure 2

Figure 3HRCT Temporal bone.
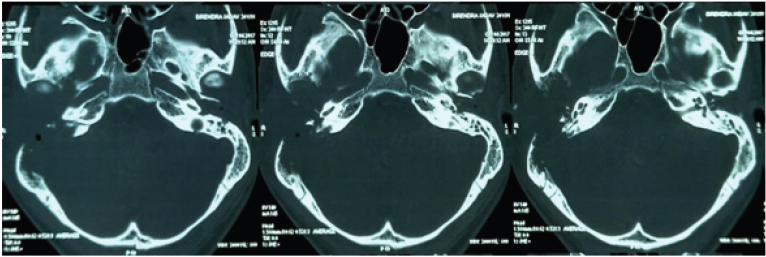
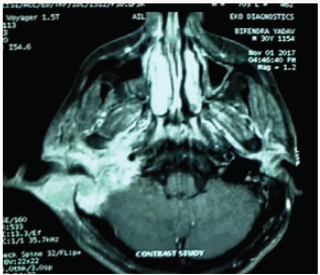
The patient was admitted and started on intravenous antiobiotics and analgesics. A high resolution CT scan of both temporal bones was ordered, which revealed a large heterogenous soft tissue density behind right pinna, measuring about 37mm x 23mm in the maximum cross sectional diameter, which extended to involve the right parotid. Soft tissue densities were also noted in bilateral ear canals. There was a large post operative cavity on the right mastoid region. Bilateral inner ear structures were normal (Figure 3). To know the extent of soft tissue involvement, a contrast MRI of both temporal bone region along with neck was ordered. T2 weighted FSE & STIR images showed large heterogenous lesion with complete bony destruction of right middle ear, involving right ear canal, pinna, right parotid and extending to middle & posterior cranial fossa, with involvement of the neurovascular planes. Focal enhancing lesion was also seen in left ear confined to petrous bone, about 28mm x 24mm x 26mm in size. These pointed towards a neoplastic lesion (Figure 4).
Figure 4Contrast MRI.
Biopsy was taken from both the ears under general anaesthesia and the ears were packed with gauze packing to control the significant amount of bleeding. Histopathological studies revealed well differentiated infiltrating keratinising squamous cell carcinoma of both the ears, with the tumour cells arranged in solid nests and sheets with peritumoral chronic inflammatory cell infiltration (Figure 5).
Figure 5H & E, 40X.
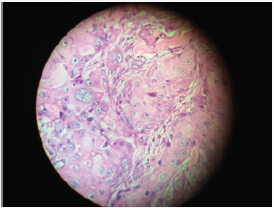
Since the tumours on both sides did not have any interconnection beween them, both were diagnosed as primaries. Using the University of Pittsburgh staging system for temporal bone tumours, the lesions on both the sides were independently staged. The right side was staged to Stage IV (T4N0M0) while the left side was staged to Stage II (T2N0M0).
Since such a large tumour required multimodality treatment, a tumour board was constituted. The lesion was deemed unresectable, so the patient was put up for palliative radiotherapy in a dosage of 30 Gy over 10 fractions. During the course of his treatment, he developed intractable pain, and his analgesics were stepped up gradually and ultimately, he had to be started on opioid analgesics (morphine tablets). Eye care for prevention of exposure keratitis was prescribed. Since prognosis was grave, the patient’s relatives were counselled about providing the best supportive care. At the last follow up, patient had completed his course of palliative chemotherapy but his general condition was extremely poor. He is alive as of January 2018.
Discussion
Squamous carcinoma of the temporal bone is a rare but aggressive tumour, usually having a poor prognosis. Survival rate decreases with increasing stage of the disease [7]. The main staging system used today, despite being flawed, is the revised Pittsburgh classification system [8,9]. Surgical resection of the tumour, with adjuvant radiotherapy for advanced stage disease appears to be the treatment of choice with the extent of surgery being a subject of debate [4,10]. Prasad et al. [11], in their meta-analysis on temporal bone carcinoma treatment, found that survival rates in case of advanced stage disease stayed poor, despite the extent of primary surgery.
Pensak et al. [12] considered that invasion of any of the following structures: cavernous sinus, carotid artery, infratemporal fossa, paraspinous musculature make a tumour unresectable. In the present case, the tumour was deemed unresectable due to spread to the infratemporal fossa and also had extensive involvement of the neurovascular planes. Since the patient already had very advanced disease in the right ear, there was no obvious benefit for operating on the left ear, and so surgery was not contemplated for the left ear although it was Stage II.
References
- Kuhel WI, Hume CR, Selesnick SH (1996) Cancer of the external auditory canal and temporal bone. Otolaryngol Clin North Am 29(5): 827-852.
- Moffat D, Wagstaff SA (2003) Squamous cell carcinoma of the temporal bone. Curr Opin Otolaryngol Head Neck Surg 11(2): 107-111.
- Beyea JA, Moberly AC (2015) Squamous cell carcinoma of the temporal bone. Otolaryngol Clin North Am 48(2): 281-292.
- Kinney SE, Wood BG (1987) Malignancies of the external ear canal and temporal bone: surgical techniques and results. Laryngoscope 97(2): 158-164.
- Bibas AG, Gleeson MJ (2006) Bilateral Squamous Cell Carcinoma of the Temporal Bones. Skull Base 16(4): 213-218.
- Vamvakidis T, Sengas J, Xenellis J (2010) Bilateral carcinoma of the temporal bone: case report and literature review. J Craniomaxillofac Surg 38(6): 473-476.
- Stell PM, McCormick MS (1984) Carcinoma of the external auditory meatus and middle ear. Clin Otolaryngol 99(9): 847-850.
- Arriaga M, Curtin H, Takahashi H, Hirsch BE, Kamerer DB (1990) Staging proposal for external auditory meatus carcinoma based on preoperative clinical examination and computed tomography findings. Ann Otol Rhinol Laryngol 99: 714-721.
- Hirsch BE (202) Staging system revision. Arch Otolaryngol Head Neck Surg 128(1): 93-94.
- Lewis JS (1983) Surgical management of tumors of the middle ear and mastoid. J Laryngol Otol 97(4): 299-311.
- Prasad S, Janecka IP (1994) Efficacy of surgical treatment for squamous cell carcinoma of the temporal bone: a literature review. Otolaryngol Head Neck Surg 110(3): 270-280.
- Pensak ML, Gleich LL, Gluckman JL, Shumrick KA (1996) Temporal bone carcinoma: contemporary perspectives in the skull base surgical era. Laryngoscope 106(10): 1234-1237.
© 2018 Titas Kar. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






