- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
Regeneration of Traumatic Tympanic Membrane Perforations
Zhengcai-Lou1* and Zihan Lou2
1Department of Otorhinolaryngology, Wenzhou Medical University, China
2Department of clinical medicine, Xinxiang medical university, China
*Corresponding author: Zhengcai-lou, Department of Otorhinolaryngology, Wenzhou Medical University, 699 Jiangdong Road, Yiwu, Zhejiang 322000, China
Submission: September 09, 2017;Published: October 27, 2017

ISSN: 2637-7780Volume1 Issue2
Abstract
Objectives/Hypothesis: To analyse the therapeutic strategies for treating traumatic tympanic membrane perforations (TTMPs).
Study Design: Literature review
Methods: The relevant literature on methods for treating human TTMPs was reviewed. The advantages and disadvantages of each treatment were analysed.
Results: A total of 24 articles were included. Among them, eight reported the efficacy of growth factors, eight considered patches, and five only observed spontaneous healing. The remaining three studies focused on other treatment methods.
Conclusion: Although 80% of TTMPs tend to spontaneously heal within 3 months, large perforations usually fail to close. Topical application of growth factors or ofloxacin ear drops is simple, convenient, and inexpensive, and it can accelerate the healing of the eardrum and improve the closure rate of large TTMPs.
Keywords: Tympanic membrane perforation; Trauma; Patch; Growth factor; Closure
Introduction
Traumatic tympanic membrane perforations (TTMPs) are commonly encountered by otologists. They can be caused by a physical blow to the ear (such as a collision or slap), blast, barotrauma (pneumatization of the mastoid cells) or insertion of sharp objects (such as cotton swabs, bobby pins and sticks) [1- 3]. Among these, collision is more often the cause in males, while perforation induced by insertion of a cotton swab is approximately twice as common in females [2]. Moreover, some previous studies have shown that the injury occurs more often in the left ear than the right [2,4,5]. TTMP patients always suffer reversible high-frequency deafness, occasionally complicated with tinnitus and vertigo [2,6,7]. Most TTMPs (about 80%) can heal spontaneously within 3 months post injury [3,4,8-11]. However, large perforations usually fail to close, and appropriate treatment should be performed to reduce the incidence of permanent impairment [9,11-14]. In this paper, a narrative review is presented to provide an overview of the selection of current therapeutic strategies for TTMP.
Method
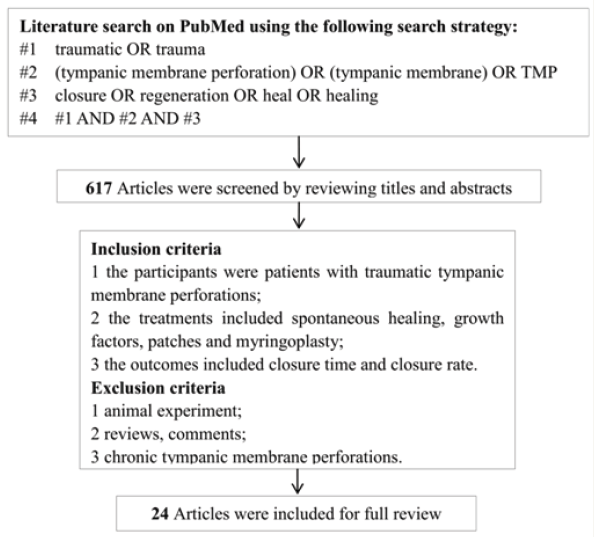
A literature search was performed on PubMed up to May 2016 to identify all published studies regarding TTMP. The search strategy is shown in Figure 1. A total of 617 articles were identified by an initial search using the following key words: “traumatic” or “trauma” and “tympanic membrane perforation” or “tympanic membrane” or “TMP” and “closure” or “regeneration” or “heal” or “healing”. These articles were screened by reviewing the titles or abstracts based on inclusion and exclusion criteria.
The inclusion criteria were patients with TTMP; treatments including spontaneous healing, growth factors, patches or myringoplasty; and outcomes including closure time and/or closure rate. Studies were excluded if patients had chronic TMP, if study subjects were animal models, and/or if the reports were reviews or comments only. Ultimately, a total of 24 articles were included: 8 reported the efficacy of growth factors for treating TTMPs [15- 22], 8 considered patches for TTMP repair [23-30], 5 focused only on the spontaneous healing of TTMPs [10,11,14,31,32], and the remaining 3 focused on other treatment methods [33-35].
Review
Spontaneous healing
Although TTMPs has a high chance of healing spontaneously [9], many factors such as the size of perforations, age of patients, aetiology (such as lightning and molten metal injuries), serosanguineous discharge and other injuries in the ear (such as malleus or umbo damage) can affect the closure rate and/or time to heal [3,12,13,32]. During spontaneous healing of TTMPs, infection is a common complication that can adversely affect the outcome [9,11,12]. TTMPs that occur under wet conditions can easily be infected and are always associated with otorrhea and purulent discharge [5,32,36]. Thus, ears with a fresh TTMP must be kept clean to prevent infection during spontaneous healing [37].
Figure 1: Literature search on Pubmed using the following search strategy.
Application of growth accelerators to promote TTMP closure
Table 1: Clinical studies on growth factors for treatment of human traumatic TMP.
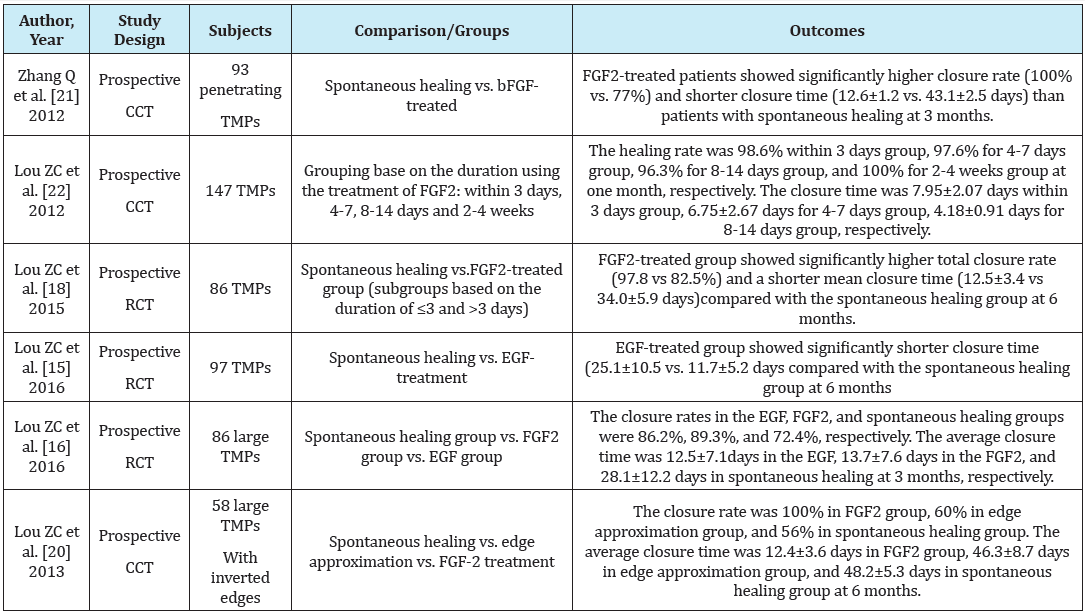
TMP: Tympanic Membrane Perforation; CCT: Clinical Control Study; RCT: Randomized Control Study; FGF2: Fibroblast Growth Factor 2.
Currently, epidermal growth factor (EGF) and basic fibroblast growth factor (bFGF/FGF-2) are the commonly used growth accelerators for TMPs; they can induce the proliferation and migration of epithelial cells and fibroblasts and stimulate angiogenesis, thereby facilitating wound healing [21,27,38,39]. For TTMPs, EGF and bFGF are effective agents that promote closure and seem to have equal efficacy [15,16,20,22] (Table 1). Moreover, a low dose of bFGF (0.1-0.15mL) has a better effect on reducing closure time compared to a high dose (0.25-0.3mL) [19]. Besides the dosage, history of chronic otitis media, residual tympanic membrane calcification and umbo or malleus injury are also risk factors associated with non-healing in patients treated with bFGF [17]. Healing outcomes are not affected by time-to-treatment (from injury to treatment with bFGF), the size of perforations and/or the presence of inverted edges [17,18,22]. There is insufficient evidence on the efficacy of EGF for accelerating TTMP healing, and more studies are needed. The efficacies of other growth factors have been explored for the treatment of TMPs. A previous study demonstrated the effects of repeated application of transforming growth factor-β1 for accelerating perforation closure in rats with acute TTMP [40]. In addition, the growth accelerator hyaluronic acid has been shown to have an equal effect as EFG for treating acute TTMP in rats and pigs [41,42]. Hyaluronic acid is a naturally occurring polysaccharide associated with various cellular processes involved in wound healing [43]. A previous study speculated that it might be a potential delivery vehicle for growth factors, thus promoting wound healing [44]. Thus, the combined application of hyaluronic acid and growth factors may have better efficacy in promoting the healing of TTMP, which should be evaluated in future studies. There is still a lack of evidence proving the efficacy of hyaluronic acid and transforming growth factor-β1 in humans. On the other hand, growth factors are inexpensive, at approximately US$3.0-4.0 per bottle. However, unfortunately, topical application of a large dose of growth factor solution may induce otorrhea and prolong closure time [15-19].
Other agents for treating TTMP
Generally, antibiotics such as ofloxacin otic drops are used to treat infections in the ear [45,46]. These drops can shorten closure time and improve the closure rate [33], possibly by inhibiting the adverse effects of infection on TMP healing [47]. However, it remains unclear whether the antibiotics or the moist environment created by the drops accelerates healing. Some studies have shown that moisture balance is important during wound healing, and a moist environment facilitates cellular growth and collagen proliferation within a healthy noncellular matrix, thereby hastening the healing of both acute and chronic wounds and promoting the growth of new tissue [48,49]. Indeed, moist TMPs have been shown to heal more rapidly than dry perforations [49,50]. In addition, eardrum healing can be affected by the environmental pH, with an acidic environment accelerating healing and an alkaline environment inhibiting it [51]. Thus, the mechanisms underlying the closurepromoting effects of ofloxacin otic drops on TTMPs should be explored in further studies. Such eardrops are common and inexpensive at approximately US$3.0 per bottle. An appropriate dose does not induce infection of the middle ear in TMPs [33]. In addition, other agents such as heparin, insulin and vitamins (vitamins C and E) may also help promote the healing of TTMPs [34,52-54]. However, the efficacies of these agents still need to be verified by clinical studies.
Patches to repair TTMP
Table 2: The healing outcome of patching on the regeneration of traumatic TMP.
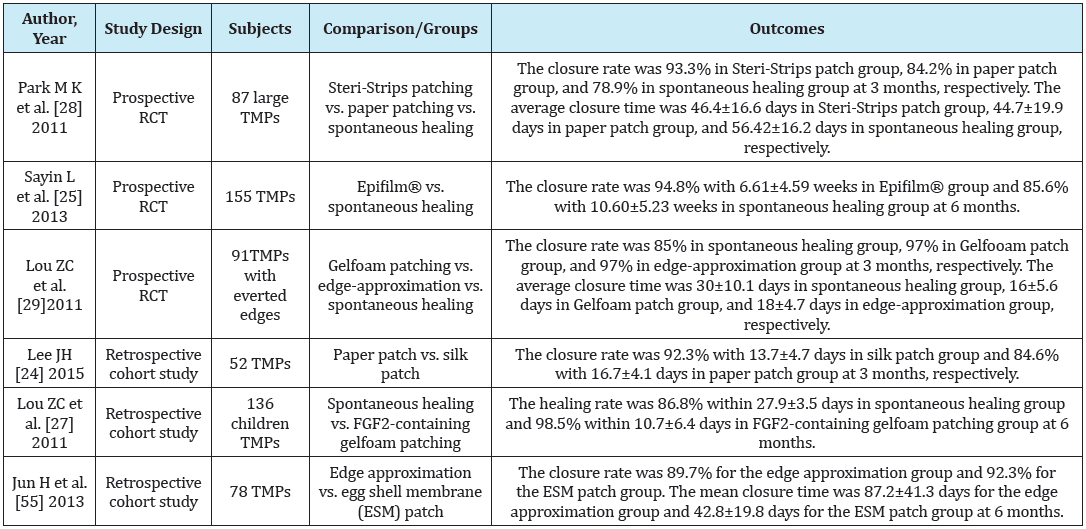
TMP: Tympanic Membrane Perforation; RCT: Randomized Control Study; FGF2: Fibroblast Growth Factor 2.
Data analysis was performed using IBM-SPSS Statistics version 23. Thechi-square test or the Fisher´s exact test (when appropriate) was used to determine whether the prevalence of the different types of bacteria was significantly different between the two groups of patients, with polyps (CRSwNP) and without polyps (CRSsNP).
Although TMPs have a high rate of spontaneous healing and they heal well with the effective application of growth factors, patching is an intermediate choice for large perforations. This strategy has good efficacy and allows surgery to be avoided when a patient complains of decreased hearing and tinnitus. Since Toynbee [23,55] successfully used a rubber disc to close a TMP in 1857, many materials have been tested for TMP repair, such as paper, silk, acellular collagen, gelfoam, Steri-Strips and watersoluble chitosan [23-28]. For TMPs, the efficacies of some patches have been evaluated in recent studies (Table 2). Gelfoam patching has a significant effect on shortening healing time without edge approximation [23,29-31]. In addition, time-to-treatment does not significantly affect its efficacy [26]. However, its results vary by the size and type of perforation [23]. Besides that, Silk [24], hyaluronic acid ester [25], Steri-Strip and paper patches [28] all significantly reduce closure time but do not significantly improve the closure rate of TMPs. However, Steri-Strips may be associated with a high incidence of otorrhea [28], which should be further investigated in future studies. In addition, some new materials have been used as patching, such as egg shell membrane and elastin, and have shown efficacy for healing TMPs [25,55]. Patching has some advantages. It facilitates centripetal epithelial migration, induces inflammation at the edges of the perforation and is associated with the proliferation of granulation tissue, which accelerates TMP closure [23]. In addition, it is associated with temporary recovery of physiological function and rapid improvement of some symptoms such as tinnitus and conductive hearing loss. Still, evidence of the effects of patching in terms of improving closure rate is still lacking [23,25,29,55]. A previous study reported that the application of gelfoam patching containing fibroblast growth factors significantly reduced closure rate and shortened closure time [27]. Thus, the combined application of growth factors and patching may be an appropriate approach for enhancing the effects of patching on closure rate. However, patches may adhere to the eardrum and be difficult to remove. In addition, although some patches such as paper and Gelfoam patches are readily available and inexpensive, other types such as acellular collagen and water soluble chitosan patches are expensive. Hence, future studies should aim to identify the most appropriate material that improves closure rate, shortens closure time and does not adhere to the eardrum.
Myringoplasty
Tang et al. successfully used a lateral graft tympanoplasty to close a TMP and improve the air-bone gap [56]. However, early surgical intervention for TTMP is rarely performed because there is a high probability of spontaneous healing [9]. Moreover, myringoplasty requires elaborate facilities and techniques, must be performed under anaesthesia in a hospital, is associated with high medical costs and can trigger various complications. Thus, it is rarely recommended. However, it should be performed if spontaneous healing does not occur after 6 months [56]. In addition, general anaesthesia may be associated with a higher percentage of defect closure, compared to untreated cases [57]. Thus, myringoplasty should be used prudently in the clinical treatment of TTMPs.
Conclusion
About 80% of traumatic TMPs heal spontaneously within 3 months. However, large perforations usually fail to close and surgical intervention should be initiated when spontaneous healing does not occur within 6 months. Nonetheless, invasive surgery is not recommended because it is associated with higher costs and risk for various complications. bFGF is an effective growth factor that accelerates the healing of traumatic TMPs. Diverse materials are used in patches and many have been shown to considerably reduce healing time but not necessarily improve closure rate. More appropriate materials should be explored in further studies. The combined application of growth factors and patching is recommended to further accelerate healing and increase the closure rate.
Funding
This study was supported by the Health & Medicine Agency of Zhejiang Province, and the Science and Technology Agency of Yiwu City, China (Grant2015KYB420 and 2015-3-06).
References
- Aktaş D, Kutlu R (2000) The relationship between traumatic tympanic membrane perforations and pneumatization of the mastoid. ORL J Otorhinolaryngol Relat Spec 62(6): 311-315.
- Hempel JM, Becker A, Müller J, Krause E, Berghaus A, Braun T (2012) Traumatic tympanic membrane perforations: Clinical and audiometric findings in 198 patients. Otol Neurotol 33(8): 1357-1362.
- Lou ZC, Lou ZH, Zhang QP (2012) Traumatic tympanic membrane perforations: A study of etiology and factors affecting outcome. Am J Otolaryngol 33(5): 549-555.
- Chun SH, Lee DW, Shin JK (1999) A clinical study of traumatic tympanic membrane perforation. Korean Journal of Otolaryngology-Head and Neck Surgery 33(5): 853-862.
- Kim CN (1986) Effect of the cellophane prosthesis to the traumatic tympanic membrane perforation. The Ewha Medical Journal 9: 197-205.
- Hussain S (1995) Hearing loss in the 4-8 kHz range following tympanic membrane perforation from minor trauma. Clin Otolaryngol Allied Sci 20(3): 211-212.
- Pusz MD, Robitschek JM (2013) Traumatic hearing loss in the context of blast-related tympanic membrane perforation. Mil Med 182(1): e1645-e1648.
- Yamazaki K, Ishijima K, Sato H (2010) A clinical study of traumatic tympanic membrane perforation. Nihon Jibiinkoka Gakkai Kaiho 113(8): 679-686.
- Al-Juboori AN (2014) Evaluation of spontaneous healing of traumatic tympanic membrane perforation. General Medicine 2: 1000129.
- Kristensen S (1992) Spontaneous healing of traumatic tympanic membrane perforations in man: A century of experience. J Laryngol Otol 106(12): 1037-1050.
- Orji F, Agu C (2008) Determinants of spontaneous healing in traumatic perforations of the tympanic membrane. Clin Otolaryngo 33(5): 420- 426.
- Griffin WL (1979) A retrospective study of traumatic tympanic membrane perforations in a clinical practice. Laryngoscope 89(2): 261- 282.
- Armstrong BW (1972) Traumatic perforations of the tympanic membrane: Observe or repair? Laryngoscope 82(10): 1822-1830.
- Jellinge M, Kristensen S, Larsen K (2015) Spontaneous closure of traumatic tympanic membrane perforations: Observational study. J Laryngol Otol 129(10): 950-954.
- Lou Z, Yang J, Tang Y, Fu Y (2016) Topical application of epidermal growth factor with no scaffold material on the healing of human traumatic tympanic membrane perforations. Clin Otolaryngol 41(6): 744-749.
- Zhengcai-Lou M, Zihan-Lou M, Yongmei-Tang M (2016) Comparative study on the effects of EGF and bFGF on the healing of human large traumatic perforations of the tympanic membrane. Laryngoscope 126(1): E23-E28.
- Lou Z, Yang J, Tang Y, Xiao J (2015) Risk factors affecting human traumatic tympanic membrane perforation regeneration therapy using fibroblast growth factor-2. Growth Factors 33(5-6): 410-418.
- Lou Z, Wang Y (2015) Evaluation of the optimum time for direct application of fibroblast growth factor to human traumatic tympanic membrane perforations. Growth Factors 33(2): 65-70.
- Lou Z, Wang Y, Yu G (2014) Effects of basic fibroblast growth factor dose on traumatic tympanic membrane perforation. Growth Factors 32(5): 150-154.
- Lou ZC, Wang YBZ (2013) Healing outcomes of large (> 50%) traumatic membrane perforations with inverted edges following no intervention, edge approximation and fibroblast growth factor application: a sequential allocation, three-armed trial. Clin Otolaryngol 38: 289-296.
- Zhang Q, Lou Z (2012) Impact of basic fibroblast growth factor on healing of tympanic membrane perforations due to direct penetrating trauma: A prospective non-blinded/controlled study. Clin Otolaryngol 37(6): 446-451.
- Lou Z, Tang Y, Wu X (2012) Analysis of the effectiveness of basic fibroblast growth factor treatment on traumatic perforation of the tympanic membrane at different time points. Am J Otolaryngol 33(2): 244-249.
- Lou Z, Tang Y, Chen H, Xiao J (2015) The perforation margin phenotypes and clinical outcome of traumatic tympanic membrane perforation with a Gelfoam patch: Our experience from a retrospective study of seventyfour patients. Clin Otolaryngol 40(4): 389-392.
- Lee JH, Lee JS, Kim D-K, Park CH, Lee HR (2015) Clinical outcomes of silk patch in acute tympanic membrane perforation. Clin Exp Otorhinolaryngol 8(2): 117-122.
- Sayin I, Kaya KH, Ekizoğlu O, Erdim İ, Kayhan FT (2013) A prospective controlled trial comparing spontaneous closure and Epifilm® patching in traumatic tympanic membrane perforations. Eur Arch Otorhinolaryngol 270(11): 2857-2863.
- Lou ZC, Hu YX, Tang YM (2011) Effect of treatment at different time intervals for traumatic tympanic membrane perforation on the closure. Acta Otolaryngol 131(10): 1032-1039.
- Lou Z, Xu L, Yang J, Wu X (2011) Outcome of children with edge-everted traumatic tympanic membrane perforations following spontaneous healing versus fibroblast growth factor-containing gelfoam patching with or without edge repair. International Journal of Pediatric Otorhinolaryngology 75(10): 1285-1288.
- Park MK, Kim KH, Lee JD, Lee BD (2011) Repair of large traumatic tympanic membrane perforation with a Steri-Strips patch. Otolaryngol Head Neck Surg 145(4): 581-585.
- Lou ZC, He JG (2011) A randomised controlled trial comparing spontaneous healing, gelfoam patching and edge-approximation plus gelfoam patching in traumatic tympanic membrane perforation with inverted or everted edges. Clin Otolaryngol 36: 221-226.
- Lou ZC, Hu YX, Tang YM (2011) Prognosis and outcome of the tympanic membrane flap at traumatic tympanic membrane perforation edge. ORL J Otorhinolaryngol Relat Spec 73(4): 212-218.
- Lou ZC, Lou ZH, Zhang QP (2012) Traumatic tympanic membrane perforations: A study of etiology and factors affecting outcome. Am J Otolaryngol 33(5): 549-555.
- Lou ZC, Tang YM, Yang J (2011) A prospective study evaluating spontaneous healing of aetiology, size and type-different groups of traumatic tympanic membrane perforation. Clin Otolaryngol 36(5): 450-460.
- Lou Z, Lou Z, Tang Y, Xiao J (2016) The effect of ofloxacin otic drops on the regeneration of human traumatic tympanic membrane perforations. Clin Otolaryngol 41(5): 564-570.
- Xin W, Zhang X, Cui L, Wei M, Yang G, et al. (2015) Comparative study of the clinical observation on traumatic perforation of tympanic membrane. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 29(18): 1610-1614.
- Tang S, Brown KD (2015) Success of lateral graft technique for closure of tympanic membrane perforations. Otol Neurotol 36(2): 250-253.
- Fagan P, Patel N (2002) A hole in the drum. An overview of tympanic membrane perforations. Aust Fam Physician 31(8): 707-710.
- Amadasun J (2002) An observational study of the management of traumatic tympanic membrane perforations. J Laryngol Otol 116(3): 181-184.
- Acharya AN, Coates H, Tavora-Vièira D, Rajan GP (2015) A pilot study investigating basic fibroblast growth factor for the repair of chronic tympanic membrane perforations in pediatric patients. Int J Pediatr Otorhinolaryngol 79(3): 332-335.
- Kaftan H, Vogelgesang S, Lempas K, Hosemann W, Herzog M (2007) Inhibition of epidermal growth factor receptor by erlotinib: wound healing of experimental tympanic membrane perforations. Otol Neurotol 28(2): 245-249.
- Kaftan H, Herzog M, Miehe B, Hosemann W (2006) Topical application of transforming growth factor-β1 in acute traumatic tympanic membrane perforations: An experimental study in rats. Wound Repair and Regeneration 14: 453-456.
- Chauvin K, Bratton CC (1999) Healing large tympanic membrane perforations using hyaluronic acid, basic fibroblast growth factor, and epidermal growth factor. Otolaryngol Head Neck Surg 121(1): 43-47.
- Güneri EA, Tekin S, Yilmaz O, Özkara E, Erdag TK, et al. (2003) The effects of hyaluronic acid, epidermal growth factor, and mitomycin in an experimental model of acute traumatic tympanic membrane perforation. Otol Neurotol 24(3): 371-376.
- Price RD, Myers S, Leigh IM, Navsaria HA (2005) The role of hyaluronic acid in wound healing. Am J Clin Dermatol 6(6): 393-402.
- Xie Y, Upton Z, Richards S, Rizzi SC, Leavesley DI (2011) Hyaluronic acid: Evaluation as a potential delivery vehicle for vitronectin: Growth factor complexes in wound healing applications. J Control Release 153(3): 225- 232.
- Poetker DM, Lindstrom DR, Patel NJ, Conley SF, Flanary VA, et al. (2006) Ofloxacin otic drops vs. neomycin-polymyxin B otic drops as prophylaxis against early postoperative tympanostomy tube otorrhea. Arch Otolaryngol Head Neck Surg 132(12): 1294-1298.
- Tong MC, Woo JK (1996) Main Articles: A double-blind comparative study of ofloxacin otic drops versus neomycin-polymyxin B-hydrocortisone otic drops in the medical treatment of chronic suppurative otitis media. J Laryngol Otol 110(4): 309-314.
- Ott MC, Lundy LB (2001) Tympanic membrane perforation in adults: How to manage, when to refer. Postgrad Med 110(5): 81-84.
- Okan D, Woo K, Ayello EA, Sibbald G (2007) The role of moisture balance in wound healing. Adv Skin Wound Care 20(1): 39-53.
- Schultz GS, Sibbald RG, Falanga V, Ayello EA, Dowsett C, et al. (2003) Wound bed preparation: A systematic approach to wound management. Wound Repair Regen 11: S1-28.
- Lou Z, Wang Y, Su K (2014) Comparison of the healing mechanisms of human dry and endogenous wet traumatic eardrum perforations. Eur Arch Otorhinolaryngol 271(8): 2153-2157.
- Akkoc A, Celik H, Arslan N, Demirci S, Hucumenoglu S, et al. (2016) The effects of different environmental pH on healing of tympanic membrane: An experimental study. Eur Arch Otorhinolaryngol 273(9): 2503-2508.
- Araujo MM, Murashima AAB, Alves VM, Jamur MC, Hyppolito MA (2016) The topical use of insulin accelerates the healing of traumatic tympanic membrane perforations. Laryngoscope 126(1): 156-162.
- Güneş A, Mutlu M, Akın İ, Köybaşioğlu F, Güvey A, et al. (2015) The impact of systemic and local administration of ascorbic acid on traumatic perforation of tympanic membrane and myringosclerosis. J Int Adv Otol 11(1): 48-52.
- Susaman N, Yalcin S, Ilhan N, Ozercan I, Kaygusuz I, et al. (2003) The effect of vitamin E on histopathologic healing and lipid peroxidation levels in experimentally induced traumatic tympanic membrane perforations. Kulak Burun Bogaz Ihtis Derg 10(3): 87-92.
- Mitchell JF (1958) Repair of tympanic perforations. Journal of Laryngology and Otology 72: 724-32.
- Tang S, Brown KD (2015) Success of lateral graft technique for closure of tympanic membrane perforations. Otol Neurotol 36(2): 250-253.
- Winerman I, Man A, Segal S (1982) Early repair of traumatic perforations of the tympanic membrane in children. Int J Pediatr Otorhinolaryngol 4(1): 23-27.
© 2017 Zhengcai-Lou, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






