- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
Choice of the Occluso-Prothetic Concept in Implantary Prosthesis
Zenati L*, Belkhieri Amel, Pr Boukais and Boukemouche A
Department of Dentistry, University of Blida, Algeria
*Corresponding author: Zenati L, Department of Dentistry, University Saad Dahlab of Blida, Algeria
Submission: August 17, 2017;Published: October 11, 2017

ISSN: 2637-7780Volume1 Issue1
Abstract
Improved implant surgery procedures and pre-implantation investigations have helped to increase the success rate of dental implants by enhancing osteo-integration and stability. The major objective of the implant act is the durability of the prosthetic construction. We have now entered the era of occluso-integration which ensures the sustainability of our implant restorations but an important question that requires a moment of reflection: Which occlusal concept to choose and for which clinical case?
Biomechanical Implant Considerations
Today the clinician is faced with widely varying concepts regarding the number, location, distribution and inclination of implants required to support the functional and para-functional demands of occlusal loading. We have to plan the occlusal scheme of our restorations supported by implants to ensure durability of our treatment. In its wider sense this includes considerations of multiple inter-relating factors of ensuring adequate bone support, implant location number, length, distribution and inclination, splinting, vertical dimension aesthetics, static and dynamic occlusal schemes [1].
Implant Positioning
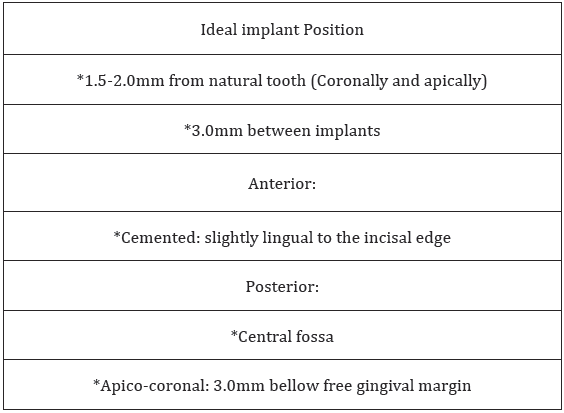
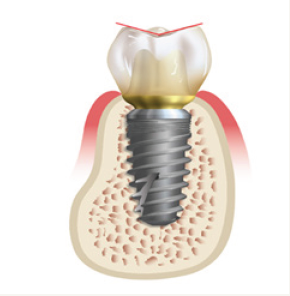
The position of the implant on the arch is crucial to minimize stress sent to the implant system. Occlusal forces are typically three-dimensional, with components directed along one or more of the clinical coordinate axes. The occlusal forces oriented along the long axis of the implant are better tolerated than if they were directed obliquely by the latter; compression will be absorbed by the bone (Table 1). Ideally, the implant body should be positioned perpendicular to the curves of Wilson and Spee to minimize the possibility of non-axial, angled forces (Figure 1).
Figure 1: Positioning implants.

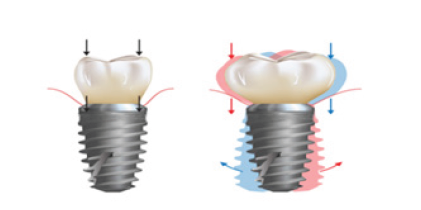
Table 1: Ideal position implant.
Maintain Narrow Posterior Occlusal Table
The greater the offset, the greater the load to the implant system the width of the occlusal table should be directly proportional to the implant body diameter. Normally, a 30-40 percent reduction in the occlusal table is recommended Figure 2.
Figure 2: Qcclusal table width.
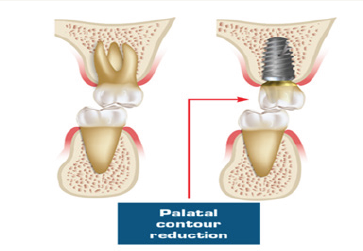
We prefer to make a maxillary crown with reduced lingual face in order not to generate forces on the implant system, this act is possible because it is endorsed by the aesthetic on the other hand the vestibular face will have a contour with a domed deflector restaurant, Aesthetic without ever coming into contact with its antagonist Figure 3.
Figure 3: The occlusal table width should be decreased by reducing the palatal contour of the maxillary implant crown.
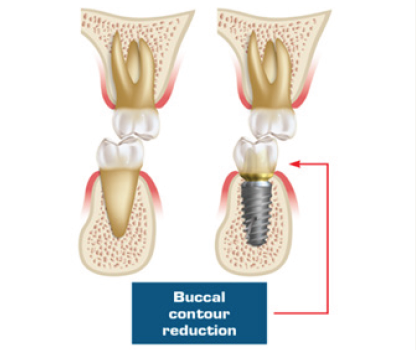
Mandibular posterior implants should have the buccal contour modified and reduced to decrease offset loads [2]. The lingual contour of the mandibular implant crown should be similar to the natural tooth to prevent tongue biting during function; however, it should be void of contacts Figure 4.
Figure 4: The occlusal table width should be decreased by reducing the buccal contour of the mandibular implant crown.
Minimal Posterior Cusp Inclination
Figure 5: Cusp inclination is reduced to flat.
The cuspidian angulations of the occlusal face must be reduced to the maximum such that the occlusal force generated during the functions and para-functions are minimal and absorbed along the major axis of the implant [3]. Studies have shown that the cortical bone of human long bones is strongest in compression, 30 percent weaker in tension, and 65 percent weaker in shear (Figure 5).
No Premature Contacts on Implant Prostheses
Any occlusal contact is considered premature if it causes a mandibular deviation during the closing path, the side towards which the mandible moves is the side or prematurity exists; that premature contact may become an occlusal interference during man dibular movements. Therefore, the occlusion should always be meticulously evaluated.
Ideal Occlusal Contact Position
Anterior
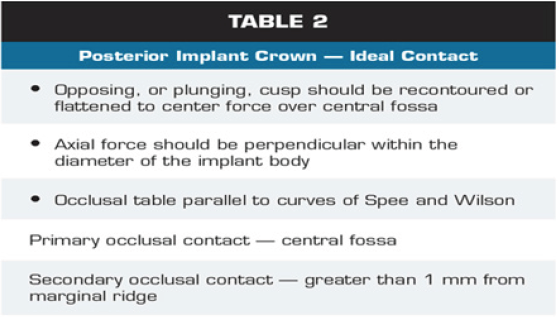
In an ideal occlusion scheme, the anterior segments are used whenever possible to disocclude the posterior teeth. Any anterior tooth placed on an implant must restore the aesthetic, on the other hand the adjacent natural teeth ensure static and dynamic occlusion, the aim is to reduce the intensity of any force. Occlusal contacts should be evaluated under heavy biting forces and during all excursive movements to ensure premature contacts are not present (Table 2).
Table 2:
Posterior
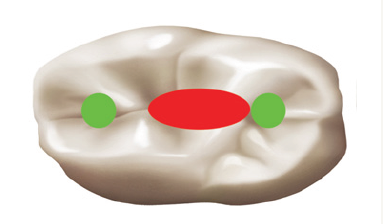
The ideal occlusal contact must be at the center of the occlusal surface a secondary contact must be 1mm in the periphery of the preliminary occlusal contact (Figure 6).
Figure 6: Central fossa preliminary contact and secondary centric contacts (green) may be placed greater than 1mm from marginal ridge.
Posterior Contact Area
Timed occlusal contacts
Ideally, natural teeth should exhibit greater initial contacts in comparison to implants through timing of the contacts. In cases where implant restorations oppose each other, the prostheses must account for the vertical movement of the adjacent teeth. The implant crown should have no contact in light biting force, which can be verified using shim stock articulating paper (i.e., less than 12 microns thick). Then, after a greater occlusal force is applied to the articulating paper, equal contact of implant crown and natural teeth should occur. For this difference mobility between the teeth and implant sobligedus to appeal the “timed” occlusion (Figure 6).
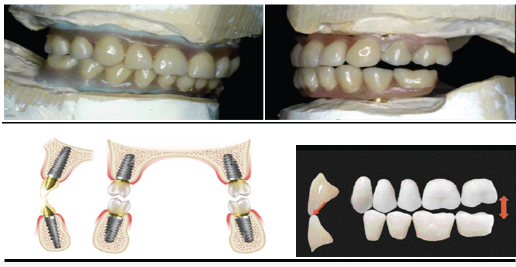
Mutually Protected Articulation
Ideally, mutually protected occlusion is the occlusal scheme for single implant restorations. This type of occlusion scheme occurs when maximum inter-cuspation coincides with the optimal condylar position or centric relation. In fact the posterior teeth protect the anterior teeth during Inter-cuspidation and the anterior teeth protect the posterior teeth during the mandibular excursions during lateral and protrusive movements. In the lateral excursions, the canines, and sometimes the lateral incisors, will disocclude the posterior teeth; we must ensure that, when the anterior teeth are implant restorations, they should not occlude in centric; especially when the opposing dentition is also implant-supported cause they procure overloads forces on the implants bodies (Figure 7 & 8).
Figure 7: The ideal primary occlusal contacts in the posterior implant prosthesis will reside within the diameter of the implant, in the central fossa area of the crown. Secondary occlusal contact should remain a minimum of 1 mm from the periphery of the implant to decrease moment loads.
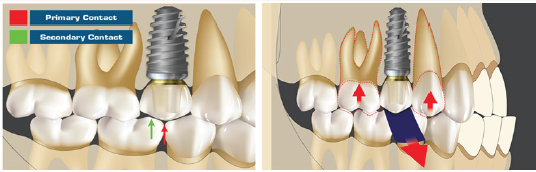
Figure 8: In an ideal occlusion scheme, the anterior segments are used whenever possible to disocclude the posterior teeth.

Clinical cases
Today the clinician is faced with widely varying concepts regarding the number, location, distribution and inclination of implants required to support the functional and para-functional demands of occlusal loading (Figure 9 & 10).
Figure 9: In class II of Kennedy-Applegate, there must be contacts in light and maximum clamping since the posterior teeth ensure the setting and centering of the mandible.
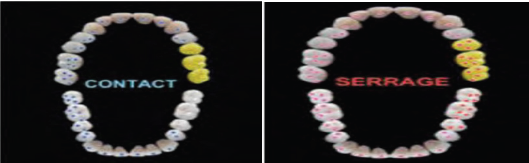
Figure 10: In case of a full-arch fixed prosthesis, if the opposing arch is a complete denture, balanced occlusion is recommended. Group function or mutually protected occlusion with shallow anterior guidance is recommended when opposing natural dentition or a full-arch fixed prosthesis. There should be no working side and balancing contact on the cantilever.
Discussion and Results
Figure 11: In case of over dentures, bilateral balanced occlusion with lingualized occlusion should be used.

The key to the success of the implant solution is how the forces are transmitted to the interface between the bone and the implant. Occlusal over loads can induce two major complications: fatigue of the metal constituting the implants, the signs calling for this state of fatigue being unscrewing, twisting or fracture of the screws, fractures of implants or the overlying prosthesis; And marginal bone loss. Failures due to occlusal overload are classified as secondary failures, after the osseointegration phase and after the loading of the implant. It seems that the main causes of complications, Fractures, are the factors of occlusal surcharge. These occlusal overloads (Figure 11), harmful both in intensity and direction, are due to two factors: initial errors in the occlusoprosthetic design and the evolution of the occluso-articular system over time (Figure 12).
Figure 12: Complications of the implants occlusal overloads.
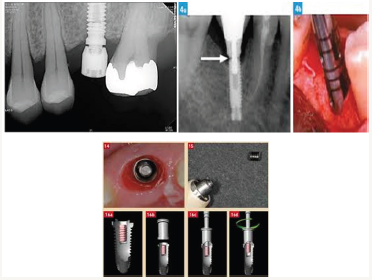
These factors can be broken down into:
A. Differential mobility between teeth and implants coupled with poor balance of the occlusal contacts in static and dynamic,
B. Interference,
C. Poor management of occlusal curves (Spee and Wilson) [4].
Conclusion
Vast subject but simple rules and commonsense can clarify it. Through our communication, we would like to emphasize the elements that underpin the choice of the occluso-prosthetic concept of implant prosthesis.
References
- Le Gall MG, Lauret JF (2011) La fonction occlusale: implications cliniques. Wolters Kluwer, Europe.
- Orthlieb JD (2000) Occlusodontie pratique. Wolters Kluwer, Europe.
- Orthlieb JD, Darmouni L, Pedinielli A, Jouvin DJ (2013) Fonctions occlusales: aspects physiologiques de l’occlusion dentaire humaine. EMC - Médecine buccale 8(1): 1-11.
- Duminil G, Laplanche O, Tardivo D (2011) Analyse occlusale instrumentale. EMC Médecine buccale 6(2): 1-11.
© 2017 Zenati L, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






