- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
What is the Role of the Transversus Abdominis Muscle in Maintaining Urinary Continence?
Ibarz Giné C1*, Girbau Moreno A2, Carnicer Cáceres J3, Cassadó Garriga J4, Rodriguez Carballeira M5 and San Segundo Mozo RM6
1Rehabilitation and Physical Medicine Department, Joan XXIII University Hospital, Spain
2Rehabilitation and Physical Medicine Department, CAP Sant Andreu, Spain
3Rehabilitation and Physical Medicine Department, Sant Pau and Santa Tecla Hospital, Spain
4Obstetrics and Gynaecology Department, Mutua Terrassa University Hospital, Associate Professor at the University of Barcelona, Spain
5Internal Medicine, Vall Hebron University Hospital, Spain
6Rehabilitation and Physical Medicine Department, Joan XXIII University Hospital, Associate professor at the Rovira I Virgili University, Spain
*Corresponding author:Cristina Ibarz Giné, Joan XXIII University Hospital, Dr Mallafré Guasch street, 4, 43005, Tarragona, Spain
Submission: February 08, 2024; Published: February 29, 2024

ISSN 2637-7934 Volume4 Issue5
Abstract
Introduction: The aetiology of urinary incontinence is multifactorial. There are ultrasound parameters
that define continence risk factors. The synergism of the abdominoperineal muscles may be lost in
incontinent patients, and it is unknown what role the transversus abdominis plays in maintaining urinary
continence. The aim is to assess whether the thickness of the transversus abdominis muscle can be a
predictive factor of continence in premenopausal women.
Material and method: A prospective case-control study was conducted among 515 women (48.5%)
incontinent, 51.5% continent. The thickness of the participants’ transversus abdominis was measured
using bidimensional ultrasound on the abdominal wall. To assess synergistic contraction,
the same measurements were taken at rest, and again after 3-4 seconds of maximum perineal muscle
contraction in the supine position while slightly flexing the knees.
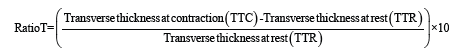
Results: 515 women were assessed: 48.5% incontinent, 51.5% continent. Abdominoperineal physiological co-contraction was identified in all of them (except one with Oxford=0). The intraclass correlation coefficient of the TTR was 0.94, and of the TTC, 0.93 (p=0.00). The TTR tended to be higher in incontinent women (0.32; SD 0.11) versus continent women (0.30; SD 0.11) (p>0.05). TTC tended to be higher in 81 continent women (0.54; SD 0.19) versus incontinent women (0.53; SD 0.20) (p>0.05), and the RatioT was higher in continent women (85.07; SD 63.4) versus incontinent women (75.5; SD 61.74) (p<0.05) in bivariate analysis. The ultrasonographic variables of the transverse thicknesses were not shown as an independent continence predictor during the multivariate analysis.
Conclusion: The procedure for measuring the thickness of the transversus abdominis thickness is simple and easily reproducible. Both continent and incontinent women experience synergistic abdominoperineal contraction. The TTC tends to be higher in continent women, as does the RatioT, while the transversus abdominis thickness cannot be defined as an independent predictor of continence in premenopausal women.
Keywords:Pelvic floor muscle; Urinary incontinence; Transversus abdominis; Ultrasound measure; Women
Abbreviations: TA: Transversus Abdominis Muscles; PFM: Pelvic Floor Muscles; TTR: Transversus Thickness at Rest; TTC: Transversus Thickness at
Contraction; ICIQ-SF: International Consultation of Incontinence Questionnaire-Short Form; 2D US: Bidimensional Ultrasound; ICC: Intraclass Correlation
Coefficient; UUI: Urgency Urinary Incontinence; SUI: Stress Urinary Incontinence; MUI: Mixed Urinary Incontinence; UI: Urinary Incontinence; IAP: Intra-
Abdominal Pressure
Key Message: The transversus abdominis muscle cannot be defined as an independent predictor of continence in premenopausal women.
Introduction
The most common urogynecological dysfunction in women is urinary incontinence. Its prevalence is estimated to be between 20- 30% [1] and varies according to age. Its aetiology is multifactorial and there are multiple pathophysiological theories that try to explain its onset [2-4], which are the subject of research and study. The literature features many studies that show coactivation and co-contraction of the abdominoperineal (core) musculature [4- 10]. The dysfunction of this synergism has been linked to urinary incontinence [11,12]. This synergism has been proven in continent women [6,13] through Electromyography (EMG). Significant differences have been identified between the EMG amplitude of the abdominal muscles during maximum voluntary contraction of the pelvic floor muscles in continent women, and those affected by severe Stress Urinary Incontinence (SUI) [7,14]. EMG, however, is an invasive procedure when it involves a needle, and inaccurate when talking about surface electromyography [7,15]. In recent years, ultrasound has become a predominant choice as a valid, economic, non-invasive and easily repeatable technique for estimating the activation and contraction of the abdominoperineal muscles in real time [7,16-18], and the abdominal muscles, as demonstrated by many studies [3,7,19].
Under normal conditions, during maximum contraction of the PFM, there is a greater recruitment and activation of the TA [14,17]. Changes in the thickness of the TA can be used to indicate changes in the electromyographic activation of the levator ani muscle. The greater the thickness of the TA, the easier and greater the electromyographic activation of the PFM [8,14]. Tajiri et al. [19] have identified the thickness of the TA in incontinent patients to be lower during PFM contraction versus continent patients. Through a study of 32 women [18], they reached the conclusion that the thickness of the TA may be a predisposing factor in the cause of urinary incontinence. In recent years, evidence of the benefits of strengthening the abdominoperineal muscles instead of the pelvic floor muscles when treating urinary incontinence is increasing [20- 22]. Despite this, there is controversy surrounding the question of whether the abdominal muscles are a predisposing factor of urinary incontinence. It is for this reason that we propose this study. This study will assess abdominoperineal synergism and whether the thickness of the TA during maximum contraction of the pelvic floor muscles, when measure using ultrasound imaging, are a predictive factor of continence in premenopausal women.
Materials and Methods
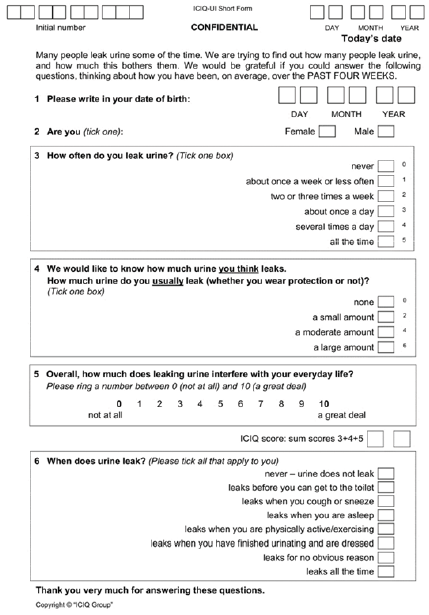
This is a prospective study: case-control with a group of continent women (ICIQ-SF=0) who scored 0 on the ICIQ-SF questionnaire, and women affected by urinary incontinence (ICIQ-SF>0) who answered affirmatively for at least the following questions: urine loss when coughing, sneezing and/or during physical exercise (question 4 of the ICIQ-SF. See appendix S1). Based on a previous pilot study that assumed a standard deviation of 85 with an α risk of 0.05 and ß risk of 0.20 (to find differences of at least 20 points in the ratio: Transversus difference between the PFM during contraction and during rest) a sample size of 500 patients was calculated: N=250 for continent patients and n=250 for incontinent.
Inclusion criteria: continent and incontinent (SUI and MUI) premenopausal women (to avoid hormonal climacteric effects on the muscles under study) over the age of 18, who wish to participate in the study.
Exclusion criteria: Menopause, pregnancy or delivery during the previous twelve months, neurological or psychological disorders resulting in a difficulty to understand and correctly perform the exercises, intense lower-back pain in the last six months and >stage two pelvic organ prolapse (Baden Walker classification). Patients with Urgency Urinary Incontinence (UUI) were excluded.
Ethics statement
All participants were informed of the purpose of the study. They agreed to collaborate voluntarily and signed an informed consent form, which had been previously assessed and approved by the Committee on Ethics and Clinical Research and Medicines (CEIm) of the Mútua de Terrassa University Hospital. The study code was EO/1608 and was accepted on 29 February 2016 with the title: „What is the role of the transverse abdominis muscle in the maintenance of urinary continence?”. The study was conducted over a period of 18 months. Continent women were recruited from gynecology and obstetrics consultations from the Occupational Health Risk and Prevention Unit of the Mútua de Terrassa University Hospital (HUMT). Incontinent women were recruited from the Pelvic Floor Unit of the same centre. All participants were interviewed by a medical professional who collected the variables, explained the ICIQ-SF questionnaire, described the procedure and provided the informed consent form. Subsequently, participants were evaluated by two blinded researchers who proceeded to assess TA thickness and simultaneous contraction of the PFM using ultrasound.
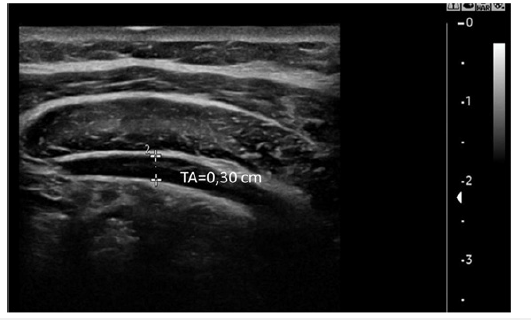
The ultrasound measurement of the TA was carried out using an ultrasound scanner from General Electric, model LOGIQ C5 Premium (manufactured in Denmark in 2012), with a linear transducer with a frequency between 8-12MHz. The patient was placed in the supine decubitus position and asked to slightly flex their knees. The transducer was placed in a transverse position on the left side of the abdominal wall, in the middle axillary line between the twelfth rib and iliac crest [7,19] (Figure 1). The TA below the Obliquus Externus (OE) and Obliquus Internus (OI) is identified between the aponeurosis of the transversus fascia of the TA at its widest point, with the perineum at rest; and subsequently, without moving the transducer, while patients performed maximum contraction of the PFM for between three and four seconds (measuring strength with the validated Oxford test) (Figures 2-4). The image is frozen with a cine-loop function returned to measure the thickness of the TA.
Figure 1:Linear transducer positioning in abdominal wall, in a half-axillary line between iliac crest and twelth rib.
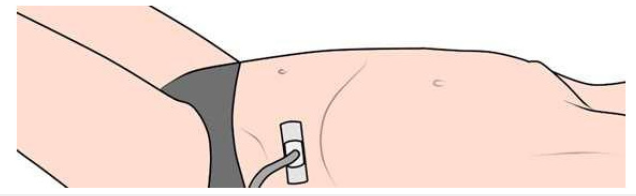
Figure 2:Location of the abdominal musculature from upper to lower. 2D-US in axial plane. OE, Obliquus externus; OI, Obliquus Internus; TA, Transversus Abdominis.
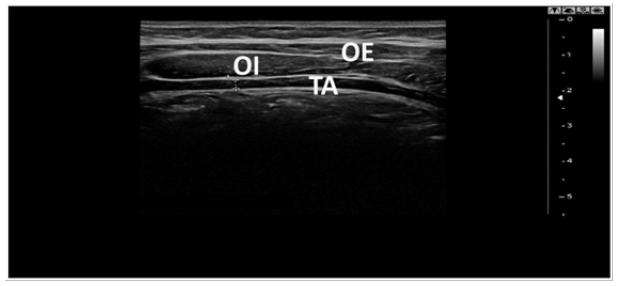
Figure 3:2D-US axial plane image of the measurement of the Transversus Abdominis (TA) muscle at rest of the pelvic floor.
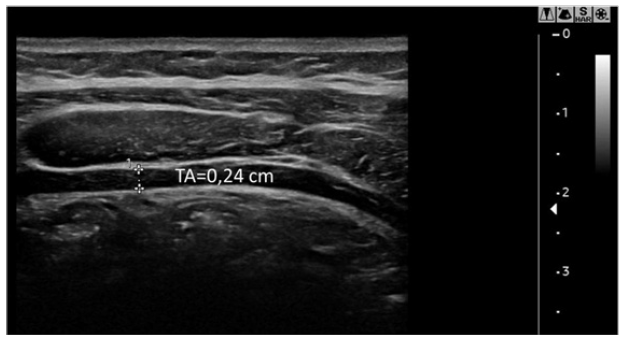
Figure 4:2D-US axial plane image of the Transversus Abdominis (TA) muscle in contraction of the pelvic floor.
Before the ultrasound was performed, the Oxford test was performed on all participants using bidigital vaginal palpation (Laycok 2002). The results obtained from the Oxford test were recorded in the database, regardless of their value. Synergic contraction was considered as “present” when the patient was asked to contract their PFM and a simultaneous contraction of the TA muscle was observed using 2D US. It was considered as “absent” when simultaneous contraction was not observed. The following epidemiological variables were collected from the total sample: Age, continence or incontinence, type of incontinence, weight, height, Body Mass Index (BMI), Oxford test results, parity, type of childbirth: Natural, assisted (forceps, vacuum), caesarean, foetal macrosomia (>4 kg), prolapse presence and if so, which type. The following ultrasound variables were defined: thickness of the transversus muscle in centimetres with the perineum at rest (TTR) and contraction (TTC). The RatioT was also calculated to avoid interpatient differences due to anatomical variables. In a group of 30 women, the thickness of the TA at rest and when the PFM when contracted was measured by the two blinded researchers described above to assess interobserver variability.
Statistical analyses
The data were analysed using the statistical package SPSS 21.00 and by means of a descriptive study of the sample obtained. The means and standard deviations for normal quantitative variables were calculated, as well as the percentages for the categorical ones. The Kolmogorov-Smirnov test was carried out to assess the type of distribution followed by the variables. When it did not follow a normal distribution pattern, non-parametric tests (U-Mann-Whitney) were carried out for the bivariate study. The reproducibility of the TA measurement using intraclass correlation coefficients was analysed (Chronbach’s alpha) with a reference value of 0 and an IC of 95%. A multivariate analysis was carried out using a logistic regression model: Forward stepwise regression method of all variables with p<0.05 (statistically significant) and of those that were clinically relevant. In the case of significant data, ROC curves were created to evaluate the capacity of the GTR, GTC and RatioT variables, and to distinguish between states of continence or incontinence.
Results
Table 1:Mean and standard deviation of the continuous
variables and number of cases and percentages of
qualitative variables referred to the total sample 515
patients. We have considered the use of 2 decimal places
in all our calculations. We have used Baden classification
for prolapses.
BMI: Body Mass Index; Ratio T: Transverse Ratio; TTC:
Thickness of Transversus at Contraction; TTR: Thickness
of Transversus at Rest.
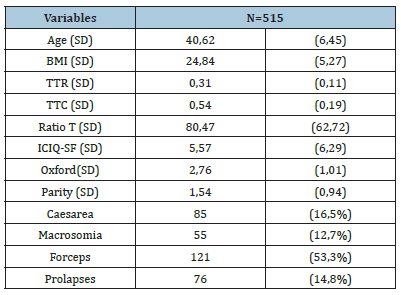
A total of 515 women were assessed: 48.5% incontinent, 51.5% continent. The mean age of incontinence was 42.10 (DS 5,45) and of continence, 39.23 (DS 6,99). Of all the incontinent patients, 83.2% had SUI and 16.8% had MUI. Some 83.5% had given birth, of which 42.9% had had an assisted birth (caesarean, forceps or vacuum), and 53.3% of these involved forceps; 12.7% of these babies had macrosomia; 14.8% of participants presented prolapse and 52.6% presented grade II cystocele (Baden Walker classification). The epidemiological and ultrasound variables are specified in Table 1. The statistical significance in bivariate and multivariate analysis for those variables is displayed in Table 2. The sample’s mean age, BMI, Oxford, parity and RatioT showed statistically significant differences in relation to continence. TTR tends to be higher in incontinent women (0.32; SD 0.11) versus continent women (0.30; SD 0.11) (p>0.05). TTC tends to be higher in continent women (0.54; SD 0.19) versus incontinent women (0.53; SD 0.20) (p>0.05) and RatioT is higher in continent women (85.07; SD 63.4) versus incontinent women (75.5; SD 61.74) (p<0.05) in bivariate analysis. Synergistic contraction was observed in all participants except one, who had Oxford 0.
Table 2:Differences between continent and incontinent patients. Statistical significance for continents and incontinent patients of the total n=515. We have considered the use of 2 decimal places in all our calculations. We have used Baden classification for prolapses.
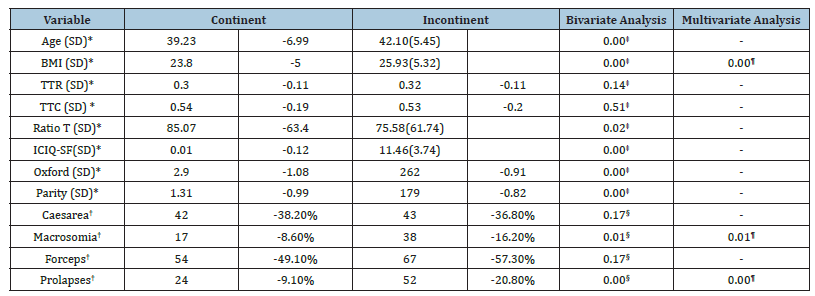
*Continuous Variables: Mean and standard deviation. †Discrete variables: Number of cases and percentages. ‡U-Mann- Whitney Statistical Test. §Pearson Chi Square Test. ¶Logistic regression (constant -1,49 and significance 0,005). BMI, Body Mass Index; Ratio T: Transverse Ratio; TTC: Thickness of Transversus at Contraction; TTR: Thickness of Transversus at Rest.
In a logistic regression model using the forward stepwise method, the incontinence variable is defined by IMC (expB 1,06; p=0,00), celes (expB 2,10; p=0,00) and macrosomia (expB 2,24; p=0,01) variables. The ultrasound variable (RatioT) measured did not prove to be an independent predictive factor of continence. Even so, the model is not wholly robust, with a Nagelkerke R Square of 0.074. The intraclass correlation coefficient (ICC) was calculated for the sample n=30 of the TTR, which is 0.94 (p=0.00), and of the TTC, 0.93 (p=0.00). The ROC curves were calculated for the variables TTR, TTC and RatioT. Area values under the curve close to 0.5 were obtained for all of them (0.46; 0.51; 0.55 respectively). As such, they confirm that the RatioT measurement does not correctly determine continence (Figure 5).
Figure 5:2D-US axial plane image of the Transversus Abdominis (TA) muscle in contraction of the pelvic floor.
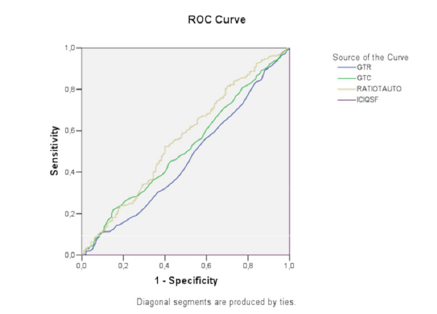
Roc curves. GTC, thickness of Transversus Abdominis in contraction; GTR, thickness of Transversus Abdominis in relaxation; RATIOAUTO, Transverse Ratio (RatioT); ICIQSF test.
Discussion
The aetiological mechanism of urinary incontinence seems to be multifactorial [3]. We found several clinical risk factors associated with urinary incontinence. Regarding the demographic variables in the present study, BMI, foetal macrosomia and the presence of prolapse were linked to incontinence as independent variables, as is widely described by other authors [23,24]. However, we also studied the biomechanical and anatomical risk factors of urinary incontinence. “Sapsford, Hodges [17], Thompson and Neumann [11,13] have shown there is a synergistic contraction of the abdominoperineal muscles under normal conditions”. Other authors have observed a synergistic co-contraction of the abdominal muscles when the PFM are contracted in both continent and incontinent women [7,9,25], as in this study. However, this synergism may be lost in incontinent women [8,26]. This synergism is widely understood as having a positive effect on lower-back pain and urinary incontinence [25,27,28]. Some authors suggest that this synergism could be a new paradigm in the treatment of urinary incontinence [22,29,30] since it could be lost. There is insufficient knowledge on the specific role of the TA muscle in this dysfunction [31-35].
Some authors argue [36] that the PFM are the only muscles capable of increasing urethral closure pressure and lifting the pelvic floor inside the pelvis to improve structural support and favour continence. A contraction of the abdominal muscles would increase IAP in the pelvic floor, and favour UI. “Tajiri et al. [18] noted that TTC was lower in incontinent patients versus continent patients in maximum contraction of the PFM and in maximum co-contraction of the PFM and TA (p<0,05)”. “They did not find statistical differences in TTR, but this value was higher in incontinent women versus continent women (p>0,05)”. In this study, we have also observed that the TTR tends to be higher in incontinent women than in continent women, perhaps in order to compensate for pelvic floor weakness. The TTC also tends to be higher in continent versus incontinent women. Neither of these two results showed statistically significant differences, as they have done in other studies [7,25].
On the other hand, the calculation of a new variable (RatioT) has been considered appropriate to avoid interpatient biases (interpersonal anatomical variability) [25,37]. The Ratio T defines the contraction capacity (measured by the change in thickness) of the transversus muscle, thereby reducing the inter-individual anatomical variability. In our study, we have seen that this ratio is higher in continent women than incontinent women (85 versus 75; p<0,05). But it is not possible to determine a predictor of continence when performing a multivariate analysis. The contraction of the transversus abdominis causes an increase in IAP. This could be the reason incontinent patients have an inhibited transversus abdominis, precisely to avoid an increase in IAP, which aggravates incontinence [11,37]. For many years, pelvic floor strengthening exercises have been shown to be predominant in treating stress urinary incontinence (evidence grade A). “Bo et al. argue that the PFM are the only muscles capable of increasing urethral closure pressure and lifting the pelvic floor within the pelvis to improve structural support”. The TA, on the other hand, has been shown to be effective in increasing IAP [13]. Therefore, the contraction of the TA can weaken the pelvic floor if there is no simultaneous cocontraction of the PFM. The lack of a temporary and strong enough co-contraction may be an explanation for female SUI. “Contrary to the work of Tajiri et al. [18], we have not been able to determine the thickness of the transversus abdominis as an independent variable of continence in premenopausal women, despite expanding the sample size”.
“Tajiri et al. [19] observe that the thickness of the TA muscle during maximum co-contraction of the abdominoperineal musculature may be useful in assessing the risk of urinary incontinence, but they do not observe statistically significant differences when assessing it during maximum contraction of the PFM alone, something the present study has not been able to demonstrate either”. The strengths of the study also lie in its sample size. The real-time assessment of abdominal muscles using 2D US has been found to provide easily reproducible and reliable values [7,18] and support the synergistic co-contraction of the abdominoperineal muscles in continent and incontinent women. This may open up another treatment paradigm for female incontinence. In summarising the results of this study, we have found that several aspects of the medical records analysis require critical review. One such aspect is that the sample of continent and incontinent patients was not homogeneous in relation to age, BMI and parity. In second place, the RatioT does not have sufficient discriminatory power between continent and incontinent patients. Given the large standard deviation of TA thickness, this can translate into a larger standard error of the mean and a less precise estimate of the population mean.
In third place, the sample of incontinent women only reported mild urinary incontinence (a severity index score of 1-2 using the Sandvik test). In fourth place, ultrasound is an indispensable tool for the morpho functional analysis of the pelvic floor and for predicting urinary incontinence [38]: vesicourethral angle, urethral mobility, bladder neck position [24,38]. In this study, these parameters were not assessed concomitantly with the 2D US study of the abdominal wall.
In fifth place, the behaviour of this muscle was not evaluated while performing the Valsalva manoeuvre, coughing or in other positions different from those mentioned in the Material and Method section of this paper [26]. In sixth place, another limited factor is that the degree of PFM strength (with a perineometer or dynamometer) was not objectively analysed, nor was the increase of IAP (or lack thereof) recorded in participants, which could both bias the results and be a reason for further study [5]. This was also not a multicentric study. There is a cohort of patients and a bias regarding participant selection. “Falah-Hassani et al. [3] argue that the aetiology of SUI is multifactorial. Urethral support [39], maintenance of PFM strength, integrity of the endopelvic fascia, neurological indemnity, and motor control can all influence urinary continence [2]”.
The factors of synergism (motor control, maintenance of IAP) and how they influence the contraction of the levator ani and abdominal muscles are unknown. It is difficult to screen continence with a single ultrasound value, as attempts had already been made to demonstrate urethral hypermobility as a predictive factor of incontinence [39]. Continence does not depend on a single factor. Further studies conducted with scientific rigour are needed to show evidence of the contraction of the levator ani muscle and its relationship with all the supporting elements of the bladder and abdominoperineal musculature.
Conclusion
The measurement of the thickness of the TA muscle (TTR and TTC) is a simple, easily reproducible and reliable value. A synergistic abdominoperineal contraction can be observed in both continent and incontinent women. The measurement of transversus abdominus thickness (RatioT) using transabdominal ultrasound imaging was not found to be an independent predictor of continence in premenopausal women.
Appendix S1:ICIQ-UI Short Form.
References
- Persson J, Wølner-Hanssen P, Rydhstroem H (2000) Obstetric risk factors for stress urinary incontinence: A population-based study. Obstet Gynecol 96(3): 440-445.
- DeLancey JOL (1996) Stress urinary incontinence: Where are we now, where should we go? Am J Obstet Gynecol 175(2): 311-319.
- Falah-Hassani K, Reeves J, Shiri R, Hickling D, McLean L (2021) The pathophysiology of stress urinary incontinence: A systematic review and meta-analysis. Int Urogynecol J 32(3): 501-552.
- Cundiff GW (2004) The pathophysiology of stress urinary incontinence: A historical perspective. Rev Urol 6(3): S10-S18.
- Thompson JA, O’Sullivan PB, Briffa NK, Neumann P (2006) Differences in muscle activation patterns during pelvic floor muscle contraction and Valsalva manouevre. Neurourol Urodyn 25(2): 148-155.
- Neumann P, Gill V (2002) Pelvic floor and abdominal muscle interaction: EMG activity and intra-abdominal pressure. Int Urogynecol J 13(2): 125-132.
- Arab AM, Chehrehrazi M (2011) Ultrasound measurement of abdominal muscles activity during abdominal hollowing and bracing in women with and without stress urinary incontinence. Man Ther 16(6): 596-601.
- Vesentini G, El Dib R, Righesso LAR, Piculo F, Marini G, et al. (2014) Pelvic floor and abdominal muscle cocontraction in women with and without pelvic floor dysfunction: A systematic review and meta-analysis. Clinics 74(12): e1319.
- Tajiri K, Huo M, Maruyama H (2014) Effects of co-contraction of both transverse abdominal muscle and pelvic floor muscle exercises for stress urinary incontinence: A randomized controlled trial. J Phys Ther Sci 26(8): 1161-1163.
- Sapsford R (2004) Rehabilitation of pelvic floor muscles utilizing trunk stabilization. Man Ther 9(1): 3-11.
- Thompson JA, O’Sullivan PB, Briffa NK, Neumann P (2007) Comparison of transperineal and transabdominal ultrasound in the assessment of voluntary pelvic floor muscle contractions and functional manoeuvres in continent and incontinent women. Int Urogynecol J 18(7): 779-186.
- Thompson JA, O’Sullivan PB (2003) Levator plate movement during voluntary pelvic floor muscle contraction in subjects with incontinence and prolapse: A cross-sectional study and review. Int Urogynecol J 14(2): 84-88.
- Sapsford RR, Hodges PW (2001) Contraction of the pelvic floor muscles during abdominal maneuvers. Arch Phys Med Rehabil 82(8): 1081-1088.
- Tajiri K, Huo M, Akiyama S, Fujisawa S, Maruyama H (2010) Measurement reliability and kinetic chain of the thickness of the transverse abdominal muscle and action potential of the levator ani muscle. J Phys Ther Sci 22(4): 451-454.
- Lee K (2019) Investigation of electromyographic activity of pelvic floor muscles in different body positions to prevent urinary incontinence. Med Sci Monit 25: 9357-9363.
- Sapsford RR, Clarke B, Hodges PW (2013) The effect of abdominal and pelvic floor muscle activation patterns on urethral pressure. World J Urol 31(3): 639-644.
- Mitova S, Avramova M, Gramatikova M (2022) Effectiveness of hypopressive gymnastics in women with pelvic floor dysfunction. J Phys Educ Sport 22(2): 416-422.
- Sapsford RR, Hodges PW, Richardson CA, Cooper DH, Markwell SJ, et al. (2001) Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn 20(1): 31-42.
- Tajiri K, Huo M, Yin K, Fujisawa S, Maruyama H (2012) An approach to assessment of female urinary incontinence risk using the thickness of the transverse abdominal muscle. J Phys Ther Sci 24(1): 43-46.
- ShahAli S, Arab AM, Talebian S, Esmaeil Ebrahimi, Andia Bahmani, et al. (2015) Reliability of ultrasound thickness measurement of the abdominal muscles during clinical isometric endurance tests. J Bodyw Mov Ther 19(3): 396-403.
- Magdalena Hagovska, Peter Urdzik, Ján Svihra (2020) Predictive Value of pelvic floor muscle morphometry using 3D/4D ultrasound in relation to the success of pelvic floor muscle training in women with stress urinary incontinence. Int J Environ Res Public Health 19(22):14757.
- Hung HC, Hsiao SM, Chih SY, Lin HH, Tsauo JY (2010) An alternative intervention for urinary incontinence: Retraining diaphragmatic, deep abdominal and pelvic floor muscle coordinated function. Man Ther 15(3): 273-279.
- Cameron AP (2022) Female urinary incontinence. Springer Publishers, USA, pp. 1-530.
- Handa V (2022) Effect of pregnancy and childbirth on urinary incontinence and pelvic organ prolapse. In: Linda Brubaker, Kristen Eckler (Eds.), UpToDate, pp. 1-11.
- Burzynski B, Gibala P, Jurys T, Knapik M, Mazur-Bialy A, et al. (2023) Ultrasound imaging of abdominal muscles activity among women with stress urinary incontinence: case-control study in Poland. Ginekol Pol 94(5): 344-349.
- Tavahomi M, Dadgoo M, Vasaghi-Gharamaleki B, Talebian S, Emami M, et al. (2023) Lateral abdominal muscle thickness during breathing maneuvers in women with and without stress urinary incontinence. Int Urogynecol J 34(8): 1939-1946.
- Nipa SI, Sriboonreung T, Paungmali A, Phongnarisorn C (2022) The effects of pelvic floor muscle exercise combined with core stability exercise on women with stress urinary incontinence following the treatment of nonspecific chronic low back pain. Adv Urol 2022: 2051374.
- Figueiredo VF, Amorim JSC, Pereira AM, Ferreira PH, Pereira LSM (2015) Associations between low back pain, urinary incontinence, and abdominal muscle recruitment as assessed via ultrasonography in the elderly. Brazilian J Phys Ther19(1): 70-76.
- Burzynski B, Jurys T, Knapik M, Burzynski K, Rzymski P, et al. (2021) Abdominal complex muscle in women with stress urinary incontinence –prospective case-control study. Arch Med Sci 19(4): 1016-1021.
- Kucukkaya B, Kahyaoglu SH (2021) Effectiveness of pelvic floor muscle and abdominal training in women with stress urinary incontinence. Psychol Heal Med 26(6): 779-786.
- Abuín-porras V, Cueva-Reguera M, Benavides-Morales P, Ávila-Pérez R, Cruz-Torres B, et al. (2020) Comparison of the abdominal wall muscle thickness in female rugby players versus non-athletic women: A cross-sectional study. Med 56(1): 1-8.
- Koppenhaver SL, Hebert JJ, Fritz JM, Parent EC, Teyhen DS, et al. (2009) Reliability of rehabilitative ultrasound imaging of the transversus abdominis and lumbar multifidus muscles. Arch Phys Med Rehabil 90(1): 87-94.
- Molnár T, Domján A, Szucs M, Surányi A, Bódis J (2022) Utilizing synergism between the transverse abdominal and pelvic floor muscles at different postures in nulliparous women: A randomized case-control study. Urol Int 106(3): 274-281.
- Larivière C, Gagnon DH, Henry SM, Preuss R, Dumas JP (2018) The effects of an 8-week stabilization exercise program on lumbar multifidus muscle thickness and activation as measured with ultrasound imaging in patients with low back pain: An exploratory study. PMR 10(5): 483-493.
- Larivière C, Gagnon D, De Oliveira E, Henry SM, Mecheri H, et al. (2013) Reliability of ultrasound measures of the transversus abdominis: Effect of task and transducer position. PMR 5(2): 104-113.
- Bø K, Sherburn M, Allen T (2003) Transabdominal ultrasound measurement of pelvic floor muscle activity when activated directly or via a transversus abdominis muscle contraction. Neurourol Urodyn 22(6): 582-588.
- Madokoro S, Miaki H (2019) Relationship between transversus abdominis muscle thickness and urinary incontinence in females at 2 months postpartum. J Phys Ther Sci 31(1): 108-111.
- Wang K, Xu X, Jia G, Jiang H (2020) Risk factors for postpartum stress urinary incontinence: A systematic review and meta-analysis. Reprod Sci 27(12): 2129-2145.
- Cassadó J, Pessarrodona A, Tulleuda R, Lluís Cabero, Marta Valls, et al. (2006) Introital ultrasonography: A comparison of women with stress incontinence due to urethral hypermobility and continent women. BJU Int 98(4): 822-828.
© 2024 Cristina Ibarz Giné. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






