- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
What are the Perceived Therapy Needs of Adults Living with Osteogenesis Imperfecta? A Focus Group Study
Sophie Barlow1*, Lucy Dove2, Gregory Booth1, Anju Jaggi3, Richard Keen4 and Judith Bubbear4
1Highly specialist physiotherapist in pain management and rehabilitation at the Royal National Orthopaedic Hospital, UK
2Advanced Practice Spinal Physiotherapist, Royal National Orthopaedic Hospital, UK
3Consultant Physiotherapist at Royal National Orthopaedic Hospital, UK
4Consultant Rheumatologist at Royal National Orthopaedic Hospital, UK
*Corresponding author:Sophie Barlow, Highly specialist physiotherapist in pain management and rehabilitation at the Royal National Orthopaedic Hospital, Brockley Hill, Stanmore, Middlesex HA7 4LP, UK
Submission: January 3, 2023; Published: January 24, 2023

ISSN 2637-7934 Volume4 Issue5
Abstract
Background: Osteogenesis Imperfecta (OI) is a rare genetic disorder characterised by fragile bones.
Clinical presentation includes multiple health issues which impact on quality of life. There is no published
data on what adults with OI perceive their therapy needs to be.
Objective: This study aims to explore the therapy needs of adults with OI.
Methods: A convenience sample of adults were recruited from a multidisciplinary OI clinic. Participants
were split into two groups based on their clinical classification. Semi-structured questions were asked
focusing on perceived needs for therapy. Thematic analysis identified common themes from the data.
Result: Eleven participants were allocated to two focus groups, ages ranged from 27-68 years. The
discussions from both groups elicited similar interconnecting themes of 1) knowledge and expertise, 2)
confidence in healthcare services, 3) access to healthcare and community services. There was consensus
that therapy was required for adults with OI and treatment was not only for fractures. However,
participants valued continuity of care with healthcare professionals who understood OI and where this
wasn’t available dissatisfaction with healthcare was identified. Therapy included multiple disciplines
reflecting the participants’ wide-ranging needs which reflected a bio-psycho-social framework.
Conclusion: The results reflect the life-long nature of OI and its impact on quality of life. Participants felt a
holistic approach to treatment was the most beneficial due to the complexity and variability of OI. Impact
statement: This study demonstrates a need for specialist multidisciplinary services to be commissioned
for adults with OI.
Keywords:Osteogenesis imperfecta; Multidisciplinary team; Therapy; Quality of life; Physiotherapy; Occupational therapy; Psychology
Introduction
Osteogenesis Imperfecta (OI), commonly known as ‘brittle bone disease’, is a rare genetic disorder of collagen synthesis. OI affects approximately 1 in every 10,000 people [1]. The clinical presentation of OI is wide ranging, the dominant clinical feature is increased fracture rates and bone fragility, but non-skeletal issues also co-exist. For example blue sclerae, joint laxity, dentinogenesis Imperfecta, cardiopulmonary involvement and hearing loss are common [2]. Medical management has traditionally involved reducing fractures, alleviating pain and increasing mobility. Adults with OI, however, have a wide range of healthcare needs, including musculoskeletal disorders, chronic pain and mental health issues which impact on quality of life [2,3].
In England, a highly specialist pediatric service was commissioned in 2016/17 by NHS England to include a Multidisciplinary Team (MDT) to manage OI in children at four centres across the UK [4] within a bio-psycho-social model of care. This provision at one of these centres includes specialist consultants, clinical nurse specialists, physiotherapists, occupational therapists, psychologists and social workers [5]. At present, no such service has been commissioned for adults with OI despite the wide ranging effects OI has on individuals’ health and wellbeing. A recent questionnaire study by the Brittle Bone Society found that a physiotherapist was the primary healthcare professional a person with OI would like to see [6] and physiotherapy involving muscle strengthening has been cited to be an important aspect of managing OI [7]. To date there has been no published data on what adults with OI perceive their therapy needs to be. The recently published Rare Disease Framework (UK) [8] acknowledges the importance of the patients’ voice as one of the key factors in the design and delivery of services in rare diseases. This study therefore aims to explore the therapy needs of adults living with OI from their own perspective to inform future service design.
Methods
Recruitment and sampling
A convenience sample of patients were recruited from a multidisciplinary OI clinic at a tertiary orthopaedic hospital in North London between August 2020 and October 2020. Patients were given a patient information leaflet detailing the aims and rationale of the study and asked to return the consent form to the lead author via email if they wished to participate. After formal consent was received, participants were given a date and link for the online focus group.
Data collection
Participants were split into two groups based on their
classification/severity of OI: group one included Type I/IV (mildmod)
and group two included Type III (severe). This split was made
due to an expected difference in response related to the severity
of their condition, which impacts their functional needs and may
influence their views on therapy requirements. Focus groups were
chosen due to several factors, they lead to insightful data and allow
participants to form connections as well as being cost and time
effective in the context of a clinical workload. Due to the COVID-19
pandemic the focus groups were held virtually per group via the
ZOOM videoconferencing platform [9]. The focus groups were
facilitated by the lead author, who is a specialist physiotherapist in
the multidisciplinary OI clinic, and a research physiotherapist with
no affiliation to the OI clinic. The focus groups consisted of four
topics that focused on:
a) The need for therapy input;
b) Previous therapy input and their experience with
accessing it;
c) What an optimal therapy service would look like and
d) Further research required for adults with OI.
These were asked as open questions and the lead author prompted further discussion as the need arose. Focus groups were audio recorded and transcribed verbatim.
Data Analysis
Braun and Clarke’s thematic analysis method (2006) [10] was used to identify commonly occurring themes from the focus group data. The lead author and consultant Rheumatologist organised the data and major themes were identified by both researchers through a coding framework. The data was reviewed line by line and attributed to the major themes identified with pertinent quotes. Once this was complete the two authors discussed the findings to agree the headings and attribute meaning to the data. A third author reviewed the analysis and themes and subthemes were discussed and agreed. Ethical approval was obtained from NHS Research Ethics Committee (Ref: IRAS 275117) prior to commencing the recruitment process. The funders played no role in the design, conduct, or reporting of this study.
Reflexivity
The purpose of this study was to understand the therapy needs for an adult population with OI. Previous discussions with patients in clinics have pertained to a dissatisfaction with previous therapy input therefore we recognise the preconceptions of the lead author. To balance this, the research physiotherapist who co-facilitated the group was not known to the patients or had any involvement in the OI MDT clinic. The data analysis was also reviewed by a third researcher who was not involved in the OI service to reduce reporting bias.
Result
Between August and October 2020, eleven participants were
recruited and participated in a focus group. Three participants
were characterised as having type I OI and three were characterised
with type IV. They were allocated to focus group one due to mildmoderate
severity. Five participants with OI type III were allocated
to group two as they have more severe disease. Their ages ranged
from 27-67 years. Participant characteristics are presented in Table
1. Each focus group lasted one hour with a 10-minute break in the
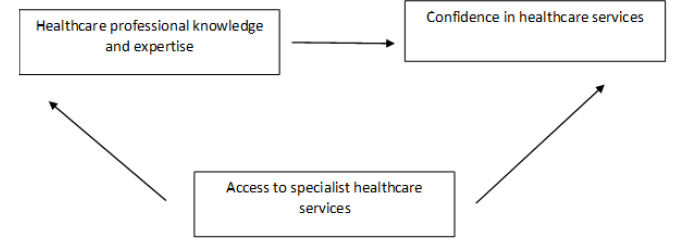
middle. With analysis of patterns across the data, the discussions
from both focus groups identified the main interconnecting themes
of
i. Knowledge and expertise,
ii. Confidence in healthcare services,
iii. Access to healthcare and community services, with
knowledge and expertise impacting someone’s confidence in
healthcare, but they are influenced by access (Figure 1).
Table 1:Demographic data of participants.
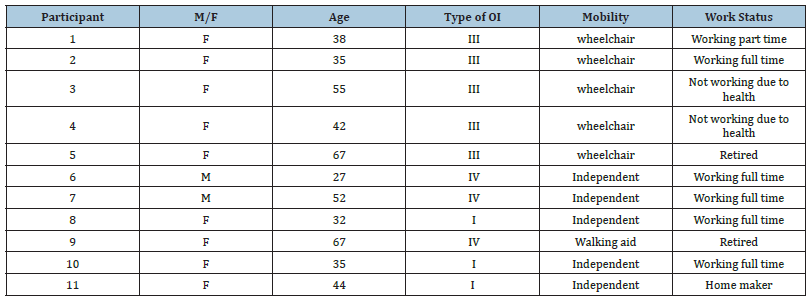
Figure 1:Inter-relationship of themes.
Specialist knowledge and expertise
Participants spoke about their desire for healthcare professionals to have specialist knowledge and expertise in OI and that understood the complexity of the condition: in
“Everyone is different and [there] is more to OI disability than just fractures” (P10).
“Yes [we] need therapy, but … with professionals who understand OI”(P8).
“I didn’t feel that it [local outpatient physiotherapy] fully took into account, understood, or adapted to my specific needs”(P7).
It was clear that where specialist knowledge was not available it presented adversity for the patient with OI:
“It’s very difficult trying to explain to someone what your condition is when they don’t have it and that could be very challenging, frustrating at times”(P9).
Where specialist healthcare was provided it was reported in terms of a complete, holistic understanding of OI as a medical condition, leading to positive connection with healthcare professionals.
“Suddenly, it was like someone actually cares about me between fractures and that was a huge deal for me because I’d not got that in all that time”(P11).
Where specialist knowledge was available, in the tertiary care multi-disciplinary clinic, for example, it was reported enthusiastically and favourably.
“Being able to develop a relationship with doctors, Physios and OTs who understand the condition [OI]…and how that is going to fluctuate over time…becomes preventative management because there is an understanding of your condition and how it affects you” (P8).
Specialist knowledge and skills were discussed in paediatric
care of OI and directly contrasted with a lack of the same in adult
care:
“When you become an adult, it kind of feels like you fall off the
precipice of any support”(P2).
“We went to [pediatric hospital], it was just amazing, the quality of the people seeing my daughter and the number of them… there was a consultant, there was a psychologist, a physiotherapist, an OT [occupational therapist] all in the room at once and we could discuss all of her needs in one go. I was just aghast and thought where’s this been for adults?” (P7).
Specialist knowledge was also discussed in terms of wider knowledge gaps in how ageing, menopause, family planning, dental treatment and mental health are affected in OI.
“I have noticed my hearing has decreased in the last year, but it seems like that is an OI sign” (P11). “[I would like] to be able to preplan, as best as possible, for life” (P7).
“I’m in my 50s now and I’m going through it [menopause]…I haven’t had any information on HRT, there’s nothing about women with OI and the menopause” (P3).
“I’m in my 30s, I am wanting to find out a bit more about it [OI]… especially as I am around the age of wanting to have children in the not-too-distant future, I want to understand how OI might impact that”(P10).
“They may not even realise how OI can affect your teeth and what the treatment was” (P9).
“I was hospitalised with CPTSD (complex post-traumatic stress disorder) due to the trauma of fractures and surgeries but they don’t get it… or have the expertise to treat it so they’re not willing to refer me on, I’m on my own as well, but lucky I have my dog” (P4).
Confidence in healthcare services
Participants talked widely of their need to have confidence and trust their healthcare professionals.
“Over time you know who you have respect for and faith in and confidence as care providers” (P3).
There were examples of one participant travelling hundreds of miles to see a specific healthcare professional who they trusted. The value of trusting healthcare professionals was implicit in the desire for continuity of care with a healthcare professional who knows and understands their background. In contrast, they also spoke about their lack of confidence in healthcare delivered in nonspecialist settings.
“I would break my leg in London and a family member [would] drive me to Sheffield to go into A&E so my surgeon can look at me” (P2).
“It’s a spectrum of services we need… with someone who really knows our individual history and therefore we don’t have to sit and explain everything” (P7).
“I didn’t have much confidence in them, [local physiotherapy] even though they were well qualified, they didn’t understand the nuances of what it means to grow up or live with OI”(P7).
“I’ve struggled to get local therapy I’ve had any degree of confidence in” (P7).
Attending emergency care for management of fractures is a common theme for people with OI. However, the participants cited multiple examples of having to explain OI to the healthcare professional. Reasons for their distrust were also given, not being believed by emergency care staff, for example
“Every time you go to [accident and emergency] you start from scratch having to explain who you are and how it [OI] affects you”(P11).
“So, when I present to [accident and emergency] with a fracture, they don’t believe me, ‘you can’t have a broken leg because you can move’”P4).
Access to healthcare and community services
Being able to access specialist healthcare services is important to people with OI and when access to specialist care was not possible there was a sense of isolation. Participants also spoke of the psychological isolation in terms of feeling different to others in society. However, they are often not able to access the psychological support they need:
“I’m really tired of not being able to get to people if and when I need them and that really ends up in me feeling a bit more isolated and having to manage myself even more”(P6).
“I don’t feel there’s enough mental therapy for people with our condition to be able to go and talk to people and express how we feel and how day-to-day life is very different” (P7).
Although participants identified the cyclical nature of their symptoms and how therapy might be helpful, they reported difficulty in accessing the right care at the right time, and that they would benefit from multidisciplinary pain management support.
“So at the moment I am going through a cycle of pain, not sleeping, worsening mental health, so physio would be great, psychotherapy would also be great, occupational therapy as well… because it helps to have another person come in to give you a different perspective”(P4).
“[It is] difficult to find the skills we need at the right time to support us”(P6). “Accessing healthcare, such a challenge, so sometimes I don’t even try to access it”(P3).
“It would be good to have some way to access them fairly directly and them be able to get back to you and then come up with some plan”(P2).
“I would go to my GP and ask to be referred to [orthopaedic surgeon at a tertiary service], they would say no you have to go to a secondary care hospital first” (P2).
Access to community services which may help to maintain wellbeing and physical health were discussed. Participants also discussed motivation to exercise was often challenging with their condition.
“My legs are a funny shape so I don’t really fit exercises bikes so I didn’t think my therapy [local exercise referral] was adapted to my specific needs” (P7).
“I did try swimming at my local pool but it wasn’t really suitable …in hospital swimming pools, they’re warm and there’s grab handles where you can hold and feel safe, [locally] I had to use a rubber ring which hurt my shoulders and the water was always cold which defeated the object” (P3).
“Maybe [exercise] in a group setting so that you can motivate each other” (P3).
Discussion
The results of this study reflect the life-long nature of OI and the need for multidisciplinary care throughout adulthood. The themes identified provide an inter-relationship between knowledge and expertise of healthcare professionals which influences a patient’s confidence in healthcare services. Patient’s need to be able to access specialist healthcare services to be able to benefit from healthcare professional’s knowledge and expertise and build confidence in them. The results demonstrate the need for specialist care delivered by healthcare professionals with specialist knowledge in OI. This promotes trust in the information and treatment they are provided with. Conversely, where there isn’t access to specialist services there seems to be a perceived lack of knowledge of OI which leads to the participants feeling isolated and excluded which promotes fear and mistrust in the healthcare they are receiving. The results also demonstrate barriers to accessing both specialist healthcare and local facilities which leads to frustration and isolation. There are similarities for patients with other rare bone disease such as x-linked hypophosphataemia (XLH). A study by Seefried [11] found that the burden of disease is often unmet which can be explained by a lack of knowledge of the spectrum of clinical problems which have an impact on patients quality of life and function. This leads to patients not receiving therapy they require and they identified the need for ongoing specialist care in adulthood..
The participants voiced their frustrations with accessing specialist care at the point of need. Hill et al. [12] recognised that adult services are not centralised and therefore participants reported having to ‘fight’ for services such as physiotherapy and often had long waiting times. This reflects the participants experience with not being able to access the right treatment at the right time. Applying the NHS ‘Going Lean’ initiative to patients with OI, which aims to enhance the patients journey by improving flow and eliminating waste, could better support access to services at the point of need [13]. It also supports co-ordination of care discussed as a priority in the NHS Rare Disease Framework [8]. This could also be achieved through a disease specific multidisciplinary team which is highly effective for children with OI [4] but not commissioned for adults in the UK.
Participants who were seen in a newly formed MDT clinic at a tertiary centre were highly satisfied with the care they received. One of the main reasons identified for this was being able to build a relationship with healthcare professionals who understand OI and who can co-ordinate appropriate treatment when required. As stated previously, patients with OI report various healthcare and therapy needs which fit within a biopsychosocial model [14]. This may include physiotherapy, occupational therapy or psychology as well as medical interventions they require over time. Developing services which involve a multidisciplinary team would support the participant’s desire for continuity of care and align with the NHS Rare Disease Framework to improve access to specialist care and treatment [8]. This is also supported by Seefried et al. [11] who reported it is important to ensure continuous healthcare for adults with XLH from a coordinated multidisciplinary team, including physical therapy and mental health support where appropriate due to the impact the disease has on patients.
One of the challenges mentioned in the results was the transition of care from paediatrics services to adult services. The experience of the participants where they felt unsupported transitioning to adult services mirrored those in a Canadian study whereby young adults with OI felt unprepared and ill equipped to navigate and access the adult health system; despite wanting to engage with healthcare providers to manage their condition [15]. It is well known that children with chronic medical conditions have benefited greatly from a robust transition programme such as those with cystic fibrosis, type 1 diabetes mellitus and congenital heart disease and Ross et al. [16] outline the need for the same for young adults with metabolic bone disease such as Hypophosphatasia (HPP), XLH, OI. They stated that improvements in medical interventions were allowing patients to live long fulfilling lives alongside their condition and therefore should have a strategic progression through adolescence into adulthood so that, their medical care remains consistent and meets their specific needs [16].
Participants in this study also recognised the importance of maintaining physical fitness and activity but were often unable to access appropriate facilities for this. Despite the benefits of building and maintaining muscle strength to improve and maintain function in people with mild to moderate OI, there is a link between disease severity and disengagement with physical activity [3]. The participants in this study provided potential solutions to support engagement in physical activity. These included setting up group exercise class specifically for adults with rare bone disease and there was a perception that this may improve motivation as well. Exercise programmes for older adults, which included peer support, can promote and improve adherence to physical activity [17]. Incorporating peer support initiatives could be considered when setting up future services that promote physical activity for people with OI [18,19].
Limitations
Participants were all recruited from a single clinical centre although it was conducted at a tertiary hospital with patients from all over the country with a range of experiences, which likely makes the study findings more transferable elsewhere. However, these patients have experience of a MDT OI clinic therefore this may be reflected in the results. The discussions held in the focus group are limited to eleven participants who were motivated and able to participate virtually in the focus groups at the time allocated. Focus groups limit the depth you can go into during conversations but are useful for participants comparing experiences and ideas. However, participants did not have to travel to the hospital for the focus groups which could have increased engagement especially during the pandemic. Multiple authors were involved in the analysis, including one who is not involved in the OI clinic which minimised bias and increased validity of the findings.
Conclusion
The results of this study reflect the life-long nature of OI and the need for multidisciplinary care throughout adulthood. Therapy services should include physiotherapy, occupational therapy and psychology to support these participants wide ranging needs. Consideration of local provision for hydrotherapy and holistic treatment centres would support adults with OI to self-manage their condition; as well as group exercise programmes which are tailored to individual needs [20]. This could be delivered as part of a wider MDT alongside medical consultants and clinical nurse specialists. Improvements in communication between services and a robust transition to adult service provision, would be beneficial to support the patient’s journey and reduce the frustrations of navigating adult services. The participants recognised the challenges of accessing the right people at the right time which is why current services need to be reformed in order to offer specialist multidisciplinary services for adults with OI [21,22]. Future research should explore the barriers to transitioning to adult services and how to facilitate this effectively. Due to the multifaceted nature of OI further research should explore the outcomes of a therapy led multidisciplinary selfmanagement programme. As well as exploring the effects of aging for the OI population.
Funding
This analysis was funded by the Brittle Bone Society, UK via a grant
Acknowledgments
With thanks to the research and innovation centre at the Royal National Orthopaedic Hospital for their support.
References
- Marr C, Seasman A, Bishop N (2017) Managing the patient with osteogenesis imperfecta: A multidisciplinary approach. Journal of Multidisciplinary Healthcare 10: 145-155.
- Swezey T, Reeve B, Hart T, Floor M, Dollar C, et al. (2018) Incorporating the patient perspective in the study of rare bone disease: Insights from the osteogenesis imperfecta community. Osteoporosis International 30(2): 507-511.
- Tosi L, Oetgen M, Floor M, Huber M, Kennelly A, et al. (2015) Initial report of the osteogenesis imperfecta adult natural history initiative. Orphanet Journal of Rare Diseases 10(1): 146.
- (2022) Highly Specialist services 2017. pp. 1-64.
- (2022) Great Ormond Street Hospital for children NHS Foundation Trust. NHS foundation Trust, UK.
- (2022) Personal Communication, Adult Service Questionnaire 2015/16 Brittle Bone Society, pp. 1-16.
- Balkefors V, Mattsson E, Pernow Y, Sääf M (2012) Functioning and quality of life in adults with mild-to-moderate osteogenesis imperfecta. Physiotherapy Research International 18(4): 203-211.
- UK Rare Diseases Framework (2022) UK Government.
- (2022) Zoom Video Communications.
- Braun V, Clarke V (2006) Using thematic analysis in psychology. Qualitative Research in Psychology 3(2): 77-101.
- Seefried L, Smyth M, Keen R, Harvengt P (2021) Burden of disease associated with X-linked hypophosphataemia in adults: A systematic literature review. Osteoporosis International 32(1): 7-22.
- Hill M, Hammond J, Sharmin M, Lewis C, Heathfield M, et al. (2022) Living with osteogenesis imperfecta: A qualitative study exploring experiences and psychosocial impact from the perspective of patients, parents and professionals. Disabil Health J 15(1): 101168.
- Going lean in the NHS (2007) NHS Institute for Innovation and Improvement. pp. 1-24.
- Kusnanto H, Agustian D, Hilmanto D (2018) Biopsychosocial model of illnesses in primary care: A hermeneutic literature review. J Family Med Prim Care 7(3): 497-500.
- Michalovic A, Anderson C, Thorstad K, Rauch F, Tsimicalis A (2020) Exploring the perceived self-management needs of young adults with osteogenesis imperfecta. Clinical Nurse Specialist 34(3): 99-106.
- Ross J, Bowden M, Yu C, Diaz-Thomas A (2023) Transition of young adults with metabolic bone diseases to adult care. Frontiers in Endocrinology 14: 1137976.
- Burton E, Farrier K, Hill K, Codde J, Airey P, et al. (2017) Effectiveness of peers in delivering programs or motivating older people to increase their participation in physical activity: Systematic review and meta-analysis. Journal of Sports Sciences 36(6): 666-678.
- Hu J, Wang Y, Li X (2020) Continuity of care in chronic diseases: A concept analysis by literature review. Journal of Korean Academy of Nursing 50(4): 513-522.
- Paterson C, McAllion S, Stellman J (1984) Osteogenesis imperfecta after the menopause. New England Journal of Medicine 310(26): 1694-1696.
- Finkelstein J, Brockwell S, Mehta V, Greendale G, Sowers M, et al. (2008) Bone mineral density changes during the menopause transition in a multiethnic cohort of women. The Journal of Clinical Endocrinology & Metabolism 93(3): 861-868.
- Watt F (2018) Musculoskeletal pain and menopause. Post Reproductive Health 24(1): 34-43.
- James Lind (2022) Priority 8 from the rare musculoskeletal diseases in adulthood PSP.
© 2023 Sophie Barlow. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






