- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
Behavioral and Psychological Symptoms of Alzheimer’s Disease, The Impact on Caregiver
Tomasello L1,2*, Ranno M1, Laganà A3, Pitrone C1 and Alibrandi A4
1Faculty of Medicine and Dentistry, Sapienza University of Rome, Italy
2Department of Clinical and Experimental Medicine, University of Messina, Italy
3Department of Biomedical and Dental Sciences, Morphological and Functional Images, Italy
4Departiment of Ecomomics, University of Messina, Italy
*Corresponding author:Letteria Tomasello, Faculty of Medicine and Dentistry, Sapienza University of Rome, 00185 Rome, Italy and Department of Clinical and Experimental Medicine, University of Messina, 98122 Messina, Italy
Submission: November 02, 2023; Published: December 22, 2023
ISSN 2637-7934 Volume4 Issue4
Abstract
Behavioural and Psychological Symptoms in Alzheimer’s disease: The burden on the caregiver patients with Alzheimer Disease need assistance and supervision in their daily activities. In literature, the term “burden” has been used to indicate the overload of work experienced by the caregiver. In our country, the patients domiciliar “take-care system” is based firstly on the family support together with the supply of health care providers and home care professionals provided by the National Health System. Caregivers of Alzheimer’s Disease (AD) patients are usually subjected to enormous physical and mental stress, as well as emotional, which may have repercussions on personal, familiar and social contest and, consequently, on quality of life [1]. The aim of our study was to investigate if behavioral and psychological symptoms could be considered as caregivers burden “predicting factors”. The objective of our study was to investigate and describe the behavioural disorders perceived by caregivers in patients with AD and evaluats to improve the quality of their caregivers.
Keywords:Alzheimer’s disease, Neuropsychiatic disorders, Caregiver distress
Introduction
Due to the progressive increase of the older population (ISTAT, 2020), nowadays there is a rise in the number of people at risk of chronic and invalidant age-related diseases. Among these, neurological diseases have peculiar significance, including dementias which are one of the most important causes of disability in older people. In most cases, Alzheimer’s Disease (AD) begins with declarative memory deficit along with slowly progressive temporal disorientation, in conjunction with the decay of another cognitive area, more often speech or executive functions [2]. This association is called “amnestic-dysexecutive syndrome”. AD involves many cognitive functions and their deficits appear in any individual with different clinical impairments [3]. The main psychological symptoms are dominated by anxiety (often associated with depression) and by psychotic manifestations with delirium of damage, abandonment and the so-called “future myopia”. Beside cognitive symptoms, there are no-cognitive symptoms, that concern personality sphere, affectivity, ideation, vegetative functions, and behavior, such as apathy, irritability, agitation, aggressiveness, disinhibition, hallucinations, deliria and eating No-cognitive symptoms are very heterogeneous and represent the major commitment in the patients management by their caregiver [4]. Depression is the second most frequent NPS in patients with Alzheimer achieves prevalence rates higher than 60 % in the lateral stages, and is often associated with anxiety [5,6].
Apathy is a set of motivational deficits, and on the affective level and in carrying out activities, is the symptom with the highest prevalence rate in patients with AD and its frequency increases with the progression of the disease, following the extension of the neuropathological process: In the early stages 42% of patients show apathy, increasing to 90% in the more advanced and serious phases [7] Agitation and aggression fall into a cluster of NPSs that is divided into two subcategories „motor agitation” and „verbal agitation ). These attitudes constitute a serious danger for the caregiver and for the patient, related to a severe degree of illness and often cause early institutionalization. Psychotic symptoms, delusions and hallucinations, are less frequent but more serious neuropsychiatric symptoms (frequent cause of institutionalization) and indicate a more rapid cognitive decline. [8,9]. The presence of neuropsychiatric symptoms, as has been amply demonstrated, anticipates the onset of cognitive symptoms. It represents a huge emotional and work overload for those who take care of the patient, often imposing the choise of hospitalization or hospitalization within specialized. For these reasons, today, we emphasize the importance of a careful assessment of that neuropsychological picture of the patient from the first moments. It is essential that the approach is taken by a multidisciplinary team both from a diagnostic and a therapeutic (pharmacological and non-pharmacological) point of view, in order to guarantee the patient a better management of the clinical picture.
Sometimes, these symptoms may be already present at early disease phases, are heterogeneous, fluctuanting and may be modified by somatic and/or environmental variables. Compromission of functional abilities of daily living has a dramatic impact on quality of life in both patients and their caregivers [10]. Treatment of behavior disturbances represents one of the principal objectives in demented patient care and it is often a challenge that requires a multimodal approach, including familial and caregiver education. Dementia is a constantly mutable disease not only from patient to patient, but also and moreover during the time. This leads to necessarily adapting rehabilitation objectives and methods in function of clinical stage, but also of person’s history. It is a “social” disease, that involves the entire familial core instead of one single person, and in which the support to caregivers is as important as the one to patients.
Patients and Caregivers
We enrolled 126 patients (61% F, 39% M; mean age 73.9 years, SD=6.51; mean M.M.S.E.:15.97, SD=5.46) consecutively admitted to the Alzheimer Special Care Unit of the Department of Neurosciences at the University of Messina. The diagnosis was made in accordance with diagnostic criteria funded on other causes of dementia exclusion by means of a standardized protocol by National Institute of Comunicative Disorders and Stroke-Alzheimer’s Disease and Related Disorder Association Work Group Criteria (NINCDSADRDA). Other cerebral pathologies absence was ascertained by brain CT or MRI without contrast mean and made at diagnosis time. One caregiver per patient participated in the study (73% F, 27% M; mean age 55.73 years).
Materials and Methods
Inclusion criteria
a) Age more than 55 years
b) Diagnosis of probable AD in accordance with NINCDSADRDA
criteria or diagnosis of MCI in accordance with criteria
proposed by Petersen et al. (1999).
Exclusion criteria
a) Positive anamnesis of stroke or precedent head traumas
b) Other neurological pathologies in comorbidity
c) Severe internal diseases, comorbidity with psychiatric
disturbances (schizophrenia)
d) Positive anamnesis of alcohol or psychotropic drug abuse
Insurgence probable period was supposed after the anamnestic investigation provided by the main caregiver. All patients underwent a specific protocol (presented as follows), a neuropsychological evaluation and a behavioral one. The study followed the ethical standards of the 1964 Helsinki declaration and written informed consent was obtained from all participants before the survey. They were assured that the transcript of the interview would remain strictly confidential and that patients would not be named in the final description and analysis.
Diagnostic iter
In the study were inserted patients from our Centre that respected inclusion criteria and that gave authorization to a clinical research participation. Both patients and their caregivers were enrolled (relatives and no-professional assistants). The dementias diagnostic iter is articulated in a “cascade” process, most of it of clinical and neuropsychological type. First, a general patient evaluation is made in order to identify the presence of dementia; then, diagnostic detailed analyses and tests array are performed so as to investigate cognitive functions (explained in details as it follows). The aim is looking for the causes, making a nosographic diagnosis, and making a differential diagnosis among various forms of dementia. In this study tests results of the proves of memory and executive functions were not reported because they were only used for diagnostic purposes. It is also important to underline that the neuropsychological array was performed after dating, in a following phase of ambulatorial visit (by the way within a week). The array was administered in order to evaluate the grade of global cognitive deterioration [11].
Clinical evaluation
We also investigated activities of daily living (with ADL and IADL scales) as well as cognitive level (with MMSE). The Behavioural and Psychological Symptoms of dementia (BPSD) and caregiver distress were assessed with the Neuropsychiatric Inventory (NPI). Activity Daily Living Scale (ADL) [12] is the most appropriate instrument to assess functional status as a measurement of the client’s ability to perform activities of daily living independently. Clinicians typically use the tool to detect problems in performing activities of daily living and to plan care accordingly. The Index ranks adequacy of performance in the six functions of bathing, dressing, toileting, transferring, continence, and feeding. Clients are scored yes/no for independence in each of the six functions. A score of 6 indicates full function, 4 indicates moderate impairment, and 2 or less indicates severe functional impairment.
Instrumental Activities of Daily Living Scale (IADL)
IADL is an appropriate instrument to assess independent living skills [13]. These skills are considered more complex than the basic activities of daily living as measured by the Katz. The instrument is most useful for identifying how a person is functioning at the present time. There are eight domains of function measured with the Lawton IADL scale. Women are scored on all 8 areas of function; historically, for men, the areas of food preparation, housekeeping, laundering are excluded. Clients are scored according to their highest level of functioning in that category. A summary score ranges from 0 (low function, dependent) to 8 (high function, independent) for women, and 0 through 5 for men. The Neuropsychiatric Inventory (NPI) [11] is a validated clinical rating instrument specifically to provide a comprehensive evaluation of neuropsychiatric symptomatology in demented patients. It is based on caregiver reporting of 10 domains of neuropsychiatric symptoms and includes both symptom frequency and severity ratings, comprising independent measures of symptom attributes, as well as a composite symptom score (frequency × severity).
Behavioral and cognitive assessment
The NPI is a validated, caregiver-based interview that assesses 10 neuropsychiatric symptom domains over the previous 4-week period: Delusions, hallucinations, dysphoria/depression, agitation/ aggression, anxiety, apathy/indifference, euphoria/elation, irritability/lability, disinhibition, and aberrant motor behaviors. Test-retest and interrater reliability, as well as content and convergent validity of the NPI, have been demonstrated previously.
Caregiver Distress Scale (NPI-D)
The NPI-D was developed to provide a quantitative measure of the distress experienced by caregivers in relation to the individual symptom domains assessed by the NPI. After rating the frequency and severity of each symptom domain of the NPI, caregivers were asked to rate the emotional or psychological distress they experienced in relation to that symptom on a 6-point scale: 0 (Not at all distressing), 1 (Minimally distressing), 2 (Mildly distressing), 3 (Moderately distressing), 4 (Severely distressing), and 5 (Very Severely or Extremely distressing). The RSS is a 15-item validated measure of general caregiver stress rated on a 4-point scale [14].
Overall cognition: The MMSE consists of thirty items that assess orientation, short and long-term memory, language, attention, visuospatial skills, and the ability to follow simple verbal and written commands. This easy-to-use and relatively quick neuropsychological test is often employed to assess the overall cognitive status We referred to norms for the Italian population considering age and education corrections [15]. All patients underwent an extensive anamnestic, neuroradiological, neurological and neuropsychological evaluation. We also investigated activities of daily living (with ADL and IADL scales) as well as cognitive level (with MMSE). The Behavioural and Psychological Symptoms of Dementia (BPSD) were assessed with the Neuropsychiatric Inventory [11]. An in-depth interview was carried out with the caregiver that included the administration of various scales and questionnaires; in particular, ADL, IADL.
Statistical Analyses
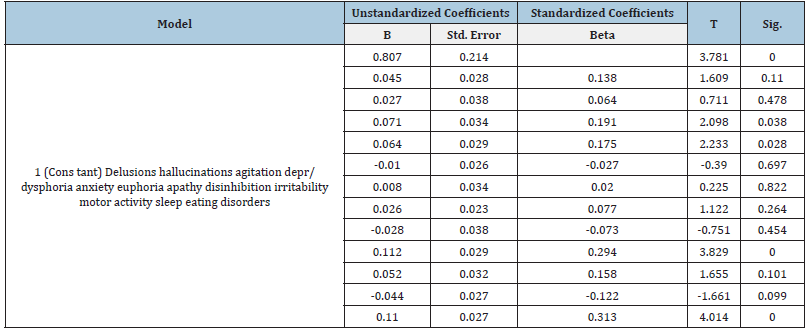
Numeric variables were described as mean and standard deviation (SD). Pearson correlation coefficient was applied in order to individuate possible correlations between NPY test, BADL scale, IADL scale and MMSE scores. Statistical analyses were conducted by means of SPSS software for Windows (22.0 version). A p-value under 0,05 was considered statistically significant. A multiple regression analysis was carried out with the various neuropsychiatric symptoms on the NPI as independent variables and the distress of the caregiver as dependent variable.
Results
The sons mainly take care of the sick (60.2%) and the spouse (32.5%), middle aged 56.8±13.5 years, mostly little educated (9.4±3.9 anni). The 76.8% of the respondents lives with the sick relative, the 65% of those is conjugated. Women are the highest percentage of caregivers with the 74.7%, significantly younger than men (p<0.01), mainly housewives (p<0.05), able to spend more hours of the day than men to the care of the family member (p<0.001). however, the mid load of stress , detected from the distress’s scale, didn’t appear considerably different in both sexes. Patients are mainly women (61.3%) and 112 men (38.7%) medium age 74.4±6 and educational level 7.5± 3.9. Ranking patients according to their MMSE scores, according the neuropsychological scales cut off, we can see that the 56.4% of the sample have a moderate to severe impairment, and the 15.9% a mild impairment. Regard to the scales that measure the independence in carrying out the activity of daily activities , we have that the average score in ADL is 3.0±1.9,while the IADL is 3.3±2.4. Any significant statistic different was found between the two sexes, for no clinical scale. The sons mainly take care of the sick (60.2%) and the spouse (32.5%), middle aged 56.8 ±13.5 years, mostly little educated (9.4±3.9 anni). About the patient’ s cognitive state of deterioration, we saw that patients with a moderate to severe impairment (MMSE<16), compared to the rest of the sample, show statistically high scores in physical activity (p<0.001),lack of sleep (p<0.001), disinhibition (p<0.001), hallucinations (p< 0.01), agitation (p<0.01), delirium (p<0.05) and irritability (p<0.05), while lower scores for depression (p<0.05). However fainlty, clinical scale’s scores are releted to the global rating of NPI. In particular the correlation between NPI and MMSE is r=-0.26 (p<0.001), r=-0.39 (p<0.001) that between NPI and ADL, and r=-0.33 (p<0.001) that between NPI and IADL. The multiple regression model showed that the most predictive patients’ symptoms were the presence of agitation, depression/ dysphoria, irritability and eating disorders. The distress of the caregivers correlated with all NPI scales except apathy. Overall, the model explained 64% of the total variance. High values in these scale produce higher levels of stress in the caregiver. Aim of this study was to examine what neuropsychiatric symptoms detected by NPI, predict the distress of the caregiver. As you can see from the schedule, distress correlate with all the scale of NPI except with apathy. Correlations between caregiver distress and neuropsychiatric symptoms at NPI (Tables 1 & 2).
Table 1:Correlations.
Source: **. Correlation is significant at the 0.01 level (2-tailed).
*Correlation is significant at the 0.05 level (2-tailed).
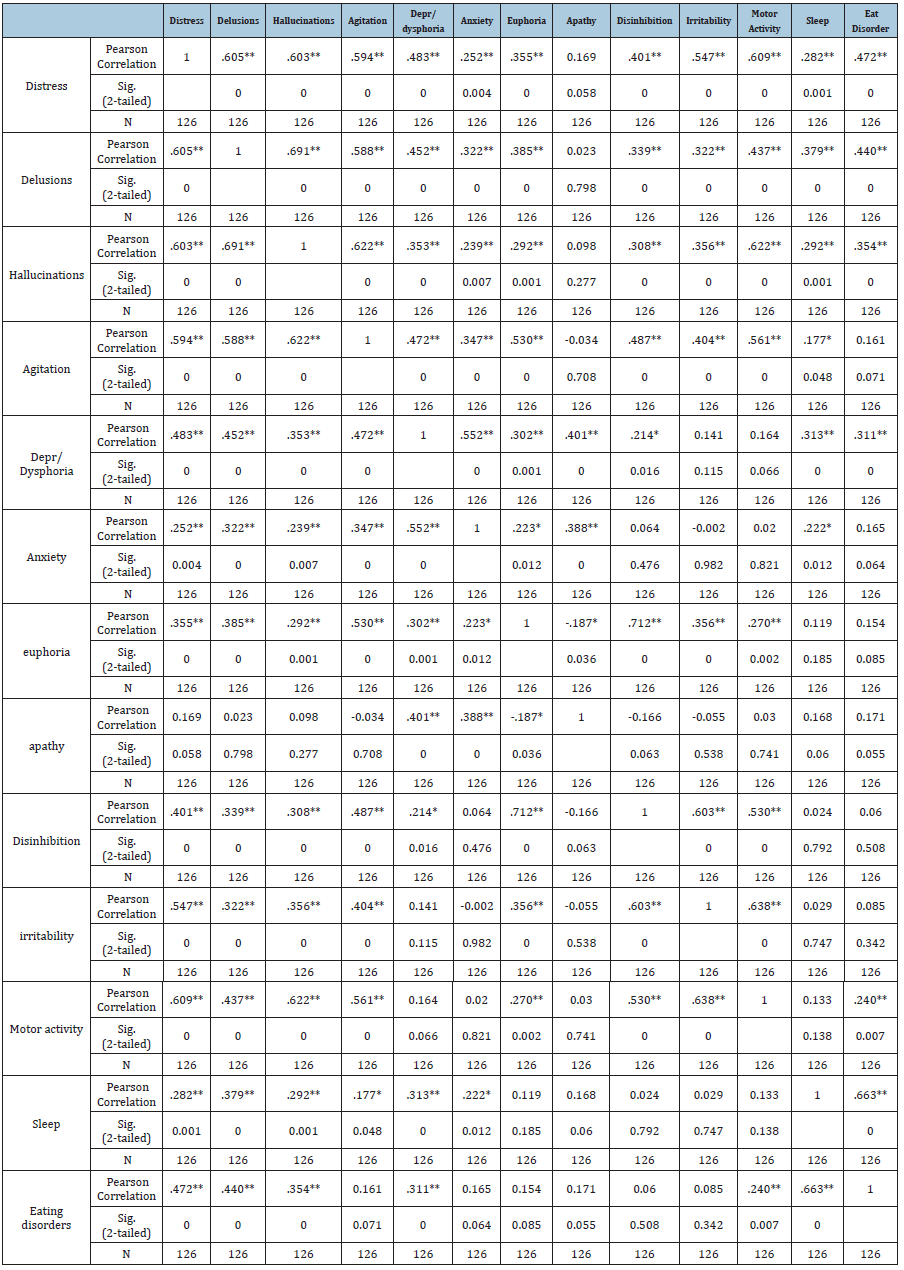
Table 2:Multiple regression conducted on the Caregiver Burden. The indipendent measures are neuropsychiatric symptoms from NPI (Cummings 1994).
About the patient’ s cognitive state of deterioration, we saw that patients with a moderate to severe impairment (MMSE<16), compared to the rest of the sample, show statistically high scores in physical activity (p<0.001),lack of sleep (p<0.001), disinhibition (p<0.001), hallucinations (p<0.01), agitation (p<0.01), delirium (p<0.05) and irritability (p<0.05), while lower scores for depression (p<0.05). However fainlty, clinical scale’s scores are releted to the global rating of NPI. In particular the correlation between NPI and MMSE is r=-0.26 (p<0.001), r=-0.39 (p<0.001) that between NPI and ADL, and r=-0.33 (p<0.001) that between NPI and IADL.
Discussion
Aim of this study was to examine what neuropsychiatric symptoms detected by NPI, predict the distress of the caregiver. The multiple regression model showed that the most predictive patients’ symptoms were the presence of agitation, depression/ dysphoria, irritability and eating disorders. The distress of the caregivers correlated with all NPI scales except apathy. Overall, the model explained 64% of the total variance. High values in these scale produce higher levels of stress in the caregiver. As you can see from the schedule, distress correlate with all the scale of NPI except with apathy. The results confirmed a very close relationship between severity of BPSD and distress of caregivers and indicated the most critical factors mediating this relationship. The behavioural and psychological symptoms of the patient affect the caregiver’s wellbeing as much (or more) than the cognitive deficits. It is known that the progression of the disease leads to greater confusion and less control over behaviour in the patient, and therefore has a profound meaning, as a reaction or response to needs, impulses, emotions, desires [16]. Also, testing the effect of residual base range of the patient in the activity of life (ADL) and in Instrumental Activities of Daily Life (IADL) on caregiver’s burden showed that the ADL and IADL scores significantly predict burden. This data can definitely be interpreted taking into account what the lack of autonomy of the patient, inevitably weighs on the caregivers, contributing significantly to burden relief.
Unlike the results reported in the study of Cipriani et al. [17] whose researchers draw attention , on the fact that apathy is recognized as a cause of considerable impact on the functional abilities of patients and as a source of care stress, from our results it is clear that distress, correlates with all behavioural disorders, except for apathy . From the review analysis in relation to the effect of ,our results , confirm the significant importance of these symptoms in patient with AD, reported with NPI , main diagnostic tools used for BPSD. Our results agree with others in the literature , that detect , the increase of BPSD with more severe cognitive impairment [18,19]. However it should be clarified that the seriousness of cognitive impairment is influenced by other things [20]. We must reflect on the appearance of BPSD hat can be watched and monitored as predictive factors of dementia [21-24].
These symptoms would also be an index of cognitive impairment [24] or functional [20], that occur with personality changes , and may be index of dementia in early stages [23]. To confirm with this osservation, in our study , the 80% of caregivers show even before behavioural disorder than cognitive ,with manifestation of mood change (apathy,irritability, sleep disorders). The presence of neuropsychiatric symptoms, as has been amply demonstrated, anticipates the onset of cognitive symptoms [25]. It represents a huge emotional and work overload for those who take care of the patient, often imposing the choice of hospitalization or hospitalization within specialized structures. For these reasons, today, we emphasize the importance of a careful assessment of that neuropsychological picture of the patient from the first moments. It is essential that the approach is taken by a multidisciplinary team both from a diagnostic and a therapeutic (pharmacological and non-pharmacological) point of view, in order to guarantee the patient a better management of the clinical picture. From a study published in 2008 (Cache County Study), in which Steinberg M. and coll. followed a group of patients for five years in order to assess the onset and progression of neuropsychiatric disorders in parallel with the course of the disease, 97% of people with dementia have experienced at least one of the symptoms during the course of the disease. In addition, it has been found that there is a greater tendency to develop symptoms such as depression (77%), apathy (71%) and anxiety (62%), while euphoria and disinhibition are less likely to develop [26].
Conclusion
Dementia is a constantly mutable disease not only from patient to patient, but also and moreover during the time. BPSD symptoms may be already present at early disease phases, are heterogeneous, fluctuanting and may be modified by somatic and/or environmental variables. Compromission of functional abilities of daily living has a dramatic impact on quality of life in both patients and their caregivers. Behavioral and Psychological Symptoms of Dementia (BPSD) are very common and are significant symptoms of the illness, contributing most to caregiver burden and often resulting in premature institutionalization of the person with dementia. According to International Psychogeriatric Association [27], among the most intrusive and difficult BPSD types to cope comprise of delusions, hallucinations, depression, and anxiety. Delusion and agitation were significantly associated with caregiver burden; Treatment of behavior disturbances represents one of the principal objectives in demented patient care and it is often a challenge that requires a multimodal approach, including familial and caregiver education [28].
This leads to necessarily adapting rehabilitation objectives and methods in function of clinical stage, but also of person’s history. It is a “social” disease, that involves the entire familial core instead of one single person, and in which the support to caregivers is as important as the one to patient. The biomedical approach is based on pathology and interventions aimed at lowering the symptoms or curing the disease. For this reason, it is more appropriate to focus on improving the quality of life rather than just on healthcare. A systematic review of Chiao et al. 2015 analyzed the functional status of patients, behavioural problems, and levels of neuropsychiatric symptoms as most loads some to informal caregivers. The consequence is that people with dementia may feel lonely or isolated [29-31]. The approach to the patient with dementia must be based on a principle of sharing both goals and care plans. The capacity of each assistant to have an interpretative approach to the disease, with its set of cognitive and non-cogni-tive symptoms, is the guarantee of an adequate interpretation and management of behavioural disorders, for a better quality of life for all family members or for patients or caregiver. Caregiver support and the treatment of behavioural disturbances in AD patients represents one key area of intervention in the care for patients with dementia. The capacity of each assistant to have an interpretative approach to the disease, with its set of cognitive and non-cognitive symptoms, is the guarantee of an adequate interpretation and management of behavioural disorders, for a better quality of life for all family members or for patients or caregivers [32].
References
- Ryu SH, Ha JH, Park DH, Yu J, Livingston G (2011) Persistence of neuropsychiatric symptoms over six months in mild cognitive impairment in community-dwelling Korean elderly. International Journal of Psychogeriatry 23(2): 214-220.
- De Vreese LP, Neri M, Fioravanti M, Belloi L, Zanetti O (2001) Memory rehabilitation in Alzheimer’s disease: A review of progress. Int J Geriatr Psychiatry 16(8): 794-809.
- Cummings JL, Frank JC, Cherry D, Kohatsu ND, Kemp B, et al. (2002) Guidelines for managing Alzheimer's disease: Part II. Treatment. Am Fam Physician 65(12): 2525-2534.
- Vugt ME, Riedijk SR, Aalten P, Tibben A, Swieten JC, et al (2006) Impact of behavioural problems on spousal caregivers: A comparison between Alzheimer’s disease and frontotemporal dementia. Dement Geriatr Cogn Disord 22(1): 35-41.
- Chi S, Wang C, Jiang T, Zhu XC, Yu JT, et al. (2015) The prevalence of depression in Alzheimer's disease: A systematic review and meta-analysis. Curr Alzheimer Res 12(2): 189-198.
- Daly M, Sutin AR, Robinson E (2021) Depression reported by US adults in 2017-2018 and march and April 2020. J Affect Disord 278: 131-135.
- Lyketsos CG, Carrillo MC, Ryan JM, Khachaturian AS, Trzepacz P, et al. (2011) Neuropsychiatric symptoms in Alzheimer's disease. Alzheimers Dement 7(5): 532-539.
- Jeste DV, Finkel SI (2000) Psychosis of Alzheimer's disease and related dementias. Diagnostic criteria for a distinct syndrome. Am J Geriatr Psychiatry 8(1): 29-34.
- Lyketsos CG, Olin J (2002) Depression in Alzheimer’s disease: overview and treatment. Biol Psychiatry 52(3): 243-252.
- Eikelboom WS, Singleton E, Berg E, Coesmans M, Raso FM, et al. (2019) Early recognition and treatment of neuropsychiatric symptoms to improve quality of life in early Alzheimer’s disease: Protocol of the BEAT-IT study. Alzheimers Res Ther 11(1): 48.
- Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, et al. (1994) The neuropsychiatric inventory: Comprehensive assessment of psychopathology in dementia. Neurology 44(12): 2308-2314.
- Katz S (1983) Assessing self-maintenance: Activities of daily living, mobility and instrumental activities of daily living. JAGS 31(12): 721-726.
- Lawton MP, Brody EM (1969) Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist 9(3): 179-186.
- Greene JC, Smith R, Gardiner M, Timbury GC (1982) Measuring behavioural disturbance of elderly demented patients in the community and its effects on relatives: A factor analytic study. Age Ageing 11(2): 121-126.
- Folstein MF, Folstein SE, McHugh PR (1975) “Mini-Mental State”: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3): 189-198.
- Kolanowski A, Boltz M, Galik E, Gitlin LN, Kales HC, et al. (2017) Determinants of behavioral and psychological symptoms of dementia: A scoping review of the evidence. Nurs Outlook 65(5): 515-529.
- Poletti M, Nuti A, Cipriani G, Bonuccelli U (2013) Behavioral and psychological symptoms of dementia: Factor analysis and relationship with cognitive impairment. Eur Neurol 69(2): 76-82.
- Almberg B, Grafström M, Winblad B (1997) Major strain and coping strategies as reported by family members who care for aged demented relatives. J Adv Nurs 26(4): 683-691.
- Piercy KW, Fauth EB, Norton MC, Pfister R, Corcoran CD, et al. (2012) Predictors of dementia caregiver depressive symptoms in a population: The cache county dementia progression study. J Gerontol B Psychol Sci Soc Sci 68(6): 921-926.
- Poletti M, Nuti A, Cipriani G, Bonuccelli U (2013) Behavioral and psychological symptoms of dementia: Factor analysis and relationship with cognitive impairment. Eur Neurol 69(2): 76-82.
- Palmer K, Lupo F, Perri R, Salamone G, Fadda L, et al. (2011) Predicting disease progression in Alzheimer's disease: The role of neuropsychiatric syndromes on functional and cognitive decline. J Alzheimers Dis 24(1): 35-45.
- Pocnet C, Rossier J, Antonietti JP, Gunten A (2013) Personality traits and behavioral and psychological symptoms in patients at an early stage of Alzheimer's disease. Int J Geriatr Psychiatry 28(3): 276-283.
- Ayuso-Mateos JL, Lasa L, Vazquez-Barquero JL, Oviedo A, Diez-Manrique JF (1999) Measuring health status in psychiatric community surveys: internal and external validity of the Spanish version of the SF-36. Acta Psychiatr Scand 99(1): 26-32.
- Arritxabal IE, Soler AG, Silva AI, Artola EU, Gonzalez IL, et al. (2011) Effects of training in emotional regulation strategies on the well-being of carers of Alzheimer patients. Rev Esp Geriatr Gerontol 46(4): 206-212.
- Bullinger M, Alonso J, Apolone G, Leplege A, Sullivan M, et al. (1998) Translating health status questionnaires and evaluating their quality: The IQOLA Project approach. International Quality of Life Assessment. J Clin Epidemiol 51(11): 913-923.
- Steinberg M, Corcoran C, Tschanz JT, Huber C, Welsh-Bohmer K, et al. (2006) Risk factors for neuropsychiatric symptoms in dementia: The Cache County study. International Journal of Geriatric Psychiatry 21(9): 824-830.
- International Psychogeriatric Association (2001) IPA Complete Guides to Behavioral and Psychological Symptoms of Dementia (BPSD).
- Huang SS, Lee MC, Liao YC, Wang WF, Lai TJ (2012) Caregiver burden associated with behavioral and psychological symptoms of dementia (BPSD) in Taiwanese elderly. Arch Gerontol Geriatri 55(1): 55-59.
- Moyle W, Kellett U, Ballantyne A, Gracia N (2011) Dementia and loneliness: An Australian perspective. Journal of Clinical Nursing 20(9-10): 1445-1453.
- Miranda-Castillo C, Woods B, Orrell M (2013) The needs of people with dementia living at home from user, caregiver and professional perspectives: A cross-sectional survey. BMC Health Serv Res 13: 43.
- Cohen-Mansfield J, Marx MS, Freedman LS, Murad H, Regier NG, et al. (2011) The comprehensive process model of engagement. Am J Geriatr Psychiatry 19(10): 859-870.
- Tomasello L, Zaccone C, Galletta S, Laganà A, Pitrone C, et al. (2023) Alzheimer’s disease and caregiver’s burden: The efficacy of a psychoeducational and psychotherapeutic groups. J Clin Images Med Case Rep 4(9): 1-7.
© 2023 Tomasello L. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






