- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
Effectiveness of a Hip Prosthetic Leg for Cardiopulmonary Two-Legged Cycle Ergometer Exercise Testing in a Trans-Pelvic Amputee: A Case Report
Takuya Osada1,2*, Tsubasa Urabe1, Masahiro Ishiyama1, Seiichi Nishino3 and Ryuuichi Ueno1
1Rehabilitation Center, Tokyo Medical University Hospital, Japan
2Cardiac Rehabilitation Center, Tokyo Medical University Hospital, Japan
3Toda Chuo Rehabilitation Hospital, Japan
*Corresponding author:Takuya Osada, Rehabilitation Center, Tokyo Medical University Hospital, 6-7-1, Nishishinjuku, Shinjuku-ku, Tokyo 160-0023, Japan
Submission: November 06, 2023; Published: November 20, 2023

ISSN 2637-7934 Volume4 Issue4
Abstract
Background:This clinical trial examined the effectiveness of a hip prosthesis (HP) for exercise tolerance/ performance using cardiopulmonary ergometer exercise testing in a trans-pelvic amputee for improving physical fitness.
Case Presentation: A 50-year-old male had undergone left trans-pelvic amputation due to osteosarcoma primarily in the left femur. After 9 months of continuous post-amputation physiotherapy, he performed breath-by-breath incremental upright cycle ergometer exercise (CERx) with 5W ramp-up (1W increasing every 12sec) to exhaustion in three different conditions: without the HP (HPoff) and with a fitted prosthetic leg HP with/without pedal rotation by the prosthetic leg (HPon+ and HPon-, respectively). Peak oxygen consumption (VO2peak), work rate, exercise time, and other parameters were measured. The peak work rates for HPoff, HPon-, and HPon+ were 24, 42, and 50W, respectively, associated with exercise times of 293, 504, and 606 sec; VO2peak of 12.6, 12.0, and 14.6ml/kg/min; peak heart rates of 158, 147, and 148 beats/min; and mean blood pressure of 133, 143, and 122mmHg.
Conclusion: For CERx to exhaustion, a fitted prosthetic leg HP (HPon+) increased peak work rate and exercise time (~2.1-fold) compared with one-legged CERx (HPon- and HPoff). The stability of two-legged pedal cranking may be improved compared with one-leg pedal cranking. Furthermore, the exercise time for HPon- was 1.7-fold (211s) longer than for HPoff, potentially because the pelvic socket provided a more stable sitting fixation/position on the saddle, allowing stable unilateral leg pedal rotation. VO2peak was similar between HPoff and HPon-, representing equivalent limitations for one-legged working muscle metabolism to exhaustion, but the slightly higher value (+2.54ml/kg/min) for HPon+ compared with HPon- may indicate more effective utilization of working muscles via two- legged pedal cranking. This case indicates the utility of an HP for two-legged exercise program development in trans-pelvic/hip disarticulation amputees.
Keywords:Exercise performance; Oxygen consumption (V-dot O2); Hemipelvectomy amputee; Hip disarticulation; Hip prosthesis; Prosthetic leg
Introduction
Hip disarticulation due to a major ablative surgery may result in complete loss of limb functionality [1-4]. The remaining single leg may fundamentally lose two-legged walking ability, leading to further decline in exercise tolerance because of the absence of two-legged dynamic exercise such as running or bicycle exercise [5] even if a hip prosthesis (HP) can be completely utilized. In the early phase post amputation, loss of one leg with hip joint ability may initially be necessary for further improvement of the locomotive function of the pelvis, trunk, as well as activity of the healthy leg. Thus, physical therapy for a hip disarticulation amputee may initially focus on the ability to achieve one-legged standing motion and body balance before fitting an HP [6] with compensation for the complete loss of activity of the major pelvic muscle group connected to the proximal femur in the basal state [1]. The use of one-legged upright cycle ergometer exercise (CERx) may be difficult because of the lack of stability of the bottom and lower body, and such exercise may be uncomfortable/painful around the resection in a sitting/upright posture on the saddle. However, dynamic physical fitness and activity are still required for hip disarticulation amputees to prevent a reduction in aerobic capacity.
In our previous case, 44-year-old male who underwent hip disarticulation amputation because of osteosarcoma showed improvement in knee range of motion, pedaling rate, and exercise time following multiple sessions of single- leg recumbent cycle ergometer exercise at 10 W over 6 consecutive days from day 15 in the early phase post amputation [7]. This previous case clearly indicated difficulty in one-legged pedal cranking caused by interaction between the upstroke and downstroke during pedal rotation. Furthermore, one-legged CERx was not performed to achieve high exercise intensity as aerobic exercise with increased heart rate (HR). The data showed that exercise performance ended in as little as 100sec because of leg fatigue without aiming for aerobic exercise in multiple secessions of single-legged recumbent CERx.
On the other hand, hip disarticulation amputees may be able to perform two-legged pedal cranking ergometer exercise as dynamic exercise for light to moderate-aerobic exercise (>10W) if a prosthetic leg with a Canadian HP can be passively moved via pedal cranking by the sound leg. Thus, two-legged exercise may maintain physical activity with quantitative exercise tolerance in the early phase after amputation. However, previous reports have lacked clinically designed programs or case studies related to twolegged dynamic CERx in hip disarticulation or other amputees. Furthermore, it is unclear how the HP can effectively support cycling exercise activity with both legs.
This clinical case presents a middle-aged (50 years old) male after hemipelvectomy (hPV) operation due to osteosarcoma and examines whether an hPV amputee can perform two-legged CERx. The study evaluated how the HP influenced upright CERx performance including exercise tolerance, exercise time, work rate intensity, and other parameters in the early phase post-hPV to determine the effectiveness of the HP by comparing 1) onelegged pedal cranking without the HP, 2) one-legged pedal cranking with a fitted prosthetic leg HP without use of the prosthetic leg, and 3) two-legged pedal cranking with a fitted HP with use of the prosthetic leg.
Case Presentation
Subject
The case was a male amputee (age: 50 years and 3 months, height: 174.2cm, weight: 106.4-108.7kg) with left hPV due to osteosarcoma in around the femoral neck and greater trochanter. He was treated for diabetes mellitus (diagnosed at age 42 years) with a hypoglycemic medication and for hypertension. The nonamputated right leg length was 110.5cm between the anterior superior iliac spine and malleolus medialis. The lower length was 56.3cm between the knee joint space and lateral malleolus. The circumference of the thigh was 72.0cm at maximum, 63.0cm at 10cm above the patella, and 58.0cm at 5cm above the patella in the nonamputated leg, and that of the lower leg was 46.4cm at maximum at the initial hip prosthesis usage. The case study was conducted in accordance with the principles of the Declaration of Helsinki (1964) and with approval of the Institutional Ethics Committee of the authors’ institution. The participant gave written consent and was informed of the nature and purpose of the clinical case trial and publication, as well as potential risks and discomfort. The patient was informed that withdrawal from the exercise sessions included the general physical therapy in rehabilitation program was possible at any time without consequences (Figure 1).
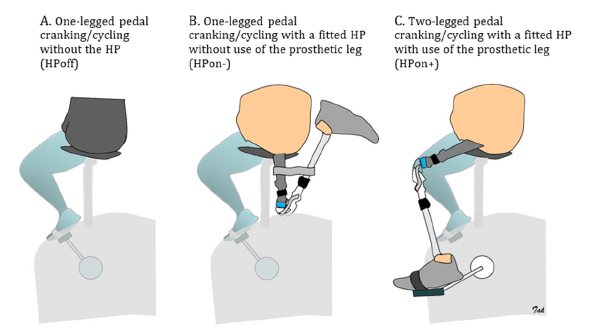
Figure 1:Schematic illustration of the three kinds of exercise model. A: One-legged pedal cranking/cycling without a hip prosthesis (HPoff), B: one-legged pedal cranking/cycling with a fitted HP without use of the prosthetic leg (HPon-), C: two-legged pedal cranking/cycling fitted HP with use of the prosthetic leg (HPon+).
Time course for treatments
Perioperative rehabilitation with physical therapy was started for muscle strength training in the right leg and both upper arms (arm ergometer exercise) at 3 months before amputation. Chemotherapy consisted of methotrexate and cisplatin/ doxorubicin hydrochloride. hPV was carried out because of primary osteosarcoma in the femur. Postoperative rehabilitation started in the intensive care unit on the third day after hPV operation, and a daily rehabilitation program targeted improvement of basic action with balance ability using one-legged standing posture as well as physical activity for the upper and lower body using forearm and/or one-legged bicycle ergometer training until the HP was ready. There were occasional occurrences of left phantom limb syndrome with pain and shaping of the separation section post-hPV. A temporary Canadian HP with hip joint (swing phase control using model nr. 7E4) configured using a rubber tension coordinated foldable floating hinge type and knee joint (polycentric knee joint with pneumatic swing phase control using model nr. 3R106) developed by Ottobock. Co., Ltd., and a prosthetic foot (J-Foot using model nr. M1170) produced by LAPOC and IMASEN Engineering Co., Ltd., was created in 8 months after hPV operation. Total weight of the HP was 4.9kg. Stability in a standing posture and during walking was used as training after fitting the HP. The K classification in the present state was K2 (ability or potential for ambulation with the ability to traverse low-level environmental barriers such as curbs, stairs, or uneven surfaces and was considered a typical community ambulator). Upright cardiopulmonary CERx testing using three different exercise models was performed from 25 days after initial use of the HP (Figure 1).
Exercise protocol
Before exercise testing, the amputee was familiarized with onelegged (without the HP or without use of the fitted prosthetic leg HP) as well as two-legged (use of a fitted prosthetic leg HP) use of the bicycle ergometer (Strength Ergo 8, BK-ERG-121, Mitsubishi Electric Engineering Co., Ltd., Tokyo, Japan) using the pace of an electric metronome at a target pedaling rate of 60 revolution per minute, with adjustment of the optimal height and tilt of the bike saddle (Figure 2). The hPV caused pain and discomfort when sitting on the bike saddle without the HP. The three different exercise models comprised: 1) one-legged pedal cranking/cycling with the sound leg without the HP (HPoff) on the first day, and consecutively 2) one-legged pedal cranking/cycling with the sound leg when fitted with the HP without use of the prosthetic leg (HPon-) on the twelfth day, and finally 3) two-legged pedal cranking/cycling when fitted with the HP with use of the prosthetic leg (HPon+) on the eighth day. After 1 min rest, the amputee started breath-bybreath cardiopulmonary upright CERx at a cranking pedal rate of 60 revolution per min without load for 3 min as a warm-up, then a work rate was applied at 5W ramping-up by 1W every 12sec, and until he reached exhaustion through leg and/or bottom fatigue. The recovery period after the end of exercise allowed enough time for potential occurrences of cardiovascular events such as arrythmia, hypotension, and/or myocardial ischemic change.
Figure 2:Picture frame of cycling ergometer exercise for three different exercise models. A: HPoff, B: HPon-, and C: HPon+. The explanations for exercise models (A-C) and the abbreviations are indicated in Figure 1. The picture frames show cycle ergometer exercise movements following pedal rotation. HPon+ shows that the left hip-knee joint in the prosthetic leg was passively extended and flexed following voluntary pedal rotation by the sound right leg.

Measurements
Pulmonary oxygen consumption (VO2) was measured using a breath-by-breath gas analyzer (Aero monitor AE-310S, MINATO Medical Science CO., Ltd., Osaka, Japan) and was determined during the pre-exercise, upright CERx, and recovery periods. In addition, parameters including carbon dioxide output (VCO2), minute ventilation (VE),ventilatory equivalent for carbon dioxide (VE/ VCO2) and oxygen (VE/VO2), respiratory exchange ratio (RER determined as VCO2/VO2), and Anaerobic Threshold (AT) point were also measured. One Metabolic Equivalent (MET) was defined as 3.5ml/kg/min. This parameter average was measured at preexercise for 1 min (basal/resting state), warming up for 3 min, AT point, and peak-exercise, respectively. The presumed maximum VO2 (VO2max) was calculated to predict maximum HR using the formula: 220-age (i.e. 170bpm in the present amputee) using the analyzed linear relationship between VO2 and HR. The age standardized value for VO2max was referenced as a minimum value of 26 ml/ kg/min (mean: 34; range: 26-45ml/kg/min) for Japanese males in their fifties from the exercise standard for healthy life 2006 from the Ministry of Health, Labour and Welfare. Electrocardiogram, arterial systolic/diastolic Blood Pressure (BP) and HR as monitoring for the cardiopulmonary exercise test (MLX-1000 system, Fukuda Denshi Co., Ltd., Tokyo, Japan) were also determined throughout testing. BP was monitored every minute using a sphygmomanometer cuff tourniquet placed on the upper part of the left arm.
Results
The parameters for three exercise models for cardiopulmonary exercise testing are shown in Table 1. The cardiovascular parameters HR, BP, and VE at pre-exercise (basal/resting state) were similar among the three exercise models. The basal metabolic state (metabolic equivalent as oxygen consumption) at pre-exercise for 1 min indicated almost 1 MET among the three exercise models. Relatively lower MET (below 1.0) was observed for both HPoff and HPon+ compared with HPon-, which may suggest slightly lower values of HR, BP, VE, and respiratory rate. During the 3-min warm-up, corresponding to pedal cranking without load, VO2 increased two times compared with the pre-exercise value. Peak exercise time/work rate achieved at exhaustion for the two-legged ergometer exercise (HPon+) was clearly longer compared with one-legged ergometer exercise (HPoff and HPon-). In particular, the peak work rate/exercise time were approximately two times greater for HPon+ compared with HPoff. Moreover, the state after HP fitting without use of the prosthetic leg (HPon-) prolonged the exercise time by 211s compared with HPoff.
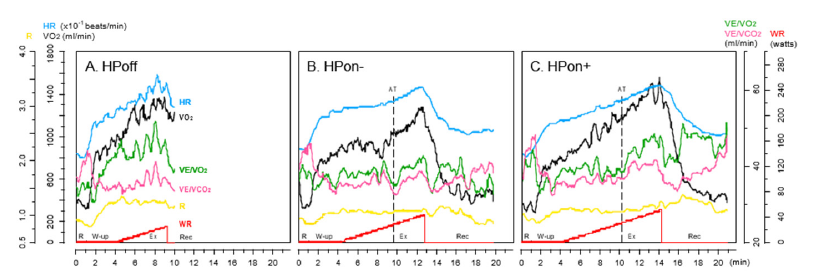
Exercise tolerance as a peak value for VO2 was higher for HPon+ than HPoff and HPon-; however, it was similar between HPoff and HPon- (Table 1 & Figure 3). One-legged cranking exercise both with HPoff and HPon- showed greater increase in BP compared with two-legged exercise (HPon+).
Table 1:The data for cardiopulmonary ergometer exercise test.
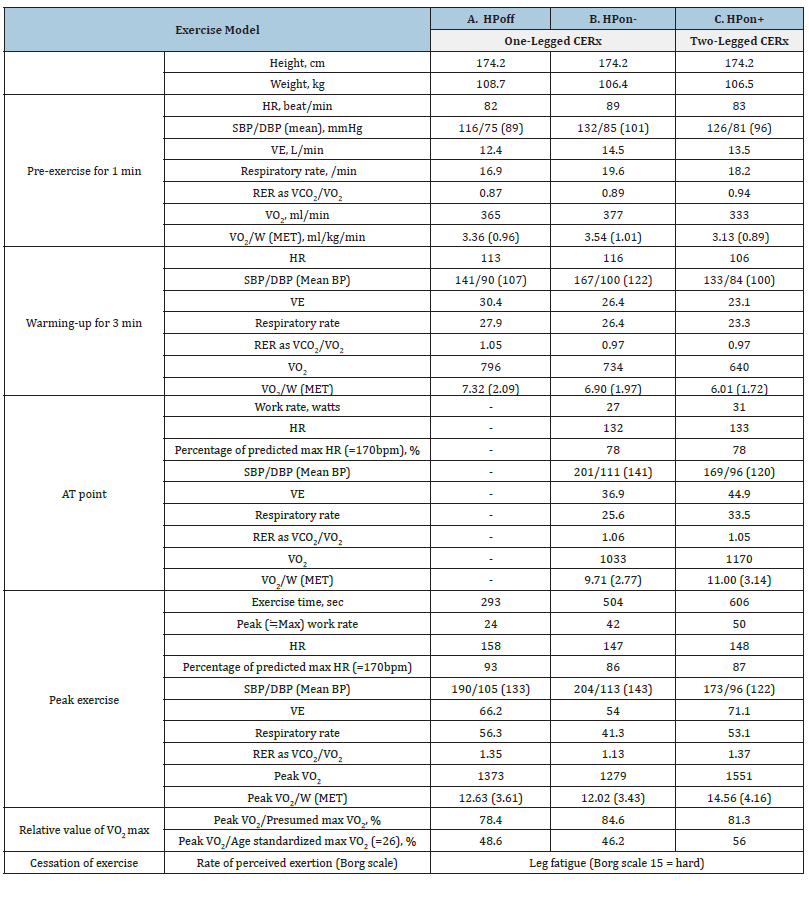
A: One-legged pedal cranking/cycle ergometer exercise (CERx) without the hip prosthesis (HPoff), B: one-legged pedal cranking/CERx with a fitted HP without use of the prosthetic leg (HPon-), C: Two-legged pedal cranking/CERx with a fitted HP with use of the prosthetic leg (HPon+), HR: Heart Rate, SBP/DBP: Systolic/Diastolic Blood Pressure, VE: Minute Ventilation, RER: Respiratory Exchange Ratio, VO2: Oxygen Consumption, VCO2: Carbon Dioxide Output, W: Weight, MET: Metabolic Equivalent, AT: Anaerobic Threshold. The AT point was not determined (indicated “-”) at HPoff. Body weight was not same among three exercise models. The capital letter “V” in the table was defined as “V-dot”.
Figure 3:Overall time course in parameters during cardiopulmonary cycle ergometer exercise tests. A: HPoff was associated with shorter exercise time compared with B: HPon- and C: HPon+. VO2 increased steeply to peak exercise. For HPoff, the AT point was not evaluated and measurements in most of the recovery phase were not recorded. A: HPoff, B: HPon-, and C: HPon+. Explanations of the exercise models (A-C) and the abbreviations are indicated in Table 1 and Figure 1. HP: hip prosthesis, R: rest (pre-exercise), W-up: warming-up, Ex: exercise, Rec: recovery. The capital letter “V” in the figure was defined as “V-dot”.
Discussion
In the present clinical case of an hPV amputee, HP fitting using a prosthetic leg for two-legged (sound and prosthetic leg) CERx allowed prolonged exercise times for upright CERx. Moreover, this study was not only unique in fitting an HP with an artificial prosthetic leg for two-legged CERx but also in comparing soundlegged CERx between fitting and non-fitting pelvic sockets to understand the effectiveness of sole pelvic socket usage. For the present amputee, exercise tolerance expressed as maximum VO2 increased by approximately 1.2 times for two-legged exercise with HPon+ compared with one-legged exercise with HPoff, with potentially increased activation of muscles in the single (right) leg and other muscle groups in the upper body because of increasing work rate during incremental ramp-up CERx. This suggested that utilization of an HP for hip disarticulation/hPV amputees may be more important when performing high intensity dynamic two-legged exercise as well as considering the initial approach for the aerobic two-legged exercise for natural body sensation. Furthermore, this work continues the findings of our previous case series, which involved estimation of the physiological and kinematic features for amputated legs with a leg exercise model focused on dynamic knee extensors [8-10] and one- legged recumbent CERx [7]. These findings are discussed below.
Considerations for differences in performance between HPon- and HPoff during one-legged ergometer exercise
The Canadian HP is utilized for amputees with hemipelvic resection, hip disarticulation, and extremely short thigh amputation. The number of cases of such HP amputees is extremely few, accounting for only 0.2% of all lower limb amputees [3,11]. Amputees with a fitted HP sometimes have discomfort due to the feeling of pressure in the socket and the weight of the prosthetic leg, instability during transfer, standing up, sitting down, and walking. During walking, the high energy requirements for hip disarticulation amputees is as much as 200% greater than those of normal subjects [12]. Furthermore, the gait with a prosthetic limb leads to higher energy consumption compared with a gait with crutches [13-16], and energy expenditure for such a gait increases by 82%, which may potentially lead to patients being confined to a wheelchair or bedridden [17,18]. For the reasons mentioned above, in most previous case reports, there are only a few reports on regaining gait with a fixed walker using an HP during the early postoperative period [19,20], one-legged recumbent CERx [7] and HP fitted biomechanical gait analysis [21], but there is only limited clinical evidence for these amputees regarding evaluation of dynamics for leg exercising using upright CERx. Notably, the present case demonstrated a 211sec prolongation of exercise time as well as an 18 W increase in peak work rate during unilateral sound leg incremental upright CERx with a fitted HP without use of a passive prosthetic leg for pedal cranking (HPon-) compared with without a fitted HP (HPoff); however, peak VO2 was similar (3.4 vs. 3.6 METs) between them (Table 1). For HPoff, peak exercise may reach a relatively high intensity such as a target HR of 93% compared with that of 87% for HPon-, although the work rate was lower for HPoff (24W) than for HPon- (42W). Moreover, there were higher values for VE and respiratory rate for HPoff compared with for HPon- (Table 1). It can be considered that single-leg exercise performance was very hard without a pelvic socket compared with when a pelvic socket was used, which can be recognized as the effectiveness of fitting a pelvic socket (Figures 1&2).
Following our previous case on a hip disarticulation amputee using recumbent CERx, rhythmical single sound- legged pedal rotation may be strengthened during the upstroke (pulling) compared with the downstroke (pushing) phase because of the lack of assistance in turning the counter leg pedal rotations [7,22]. The anterior thigh muscle mass mainly works during pushing pedaling rotation, and the posterior thigh muscle mass mainly works during pulling pedaling rotation during one-legged pedal cranking [23,24]. Therefore, in the present amputee it was hard to maintain target pedal rotation with HPoff because of instability in the sitting posture on the saddle with painful feeling of being pushed in the pelvic resection owing to loss of the ischium and pubis covering flap and wound dehiscence healing on the bottom. Moreover, increasing systolic BP approaching 200mmHg may be an indicator of the strain during exercise with both HPoff and HPon- because of increasing intrathoracic pressure when holding the breath during upstroke pedal rotation, which is a relatively low VE at peak exercise (Table 1).
It was speculated that this may lead to increasing muscle activity in the posterior more than anterior thigh through a pedal rotation even at a low exercise work rate, indicating the peak VO2 with HPoff was equal to that with HPon-. In other words, it was realized that the stability with the anatomically adaptive pelvic socket because of alignment the spine and pelvis may reduce the pain in the resected stump during one-legged pedal rotation and may prevent shaking of the trunk by the fixation of the buttocks.
The effectiveness of a fitted prosthetic leg HP for twopedal cranking
The present case clearly showed the success of two-legged upright pedal cranking in an hPV amputee. The hip- knee joint in the prosthetic leg was passively extended and flexed following voluntary pedal rotation by the sound leg (Figure 3C). This mechanically passive rotation of the prosthetic leg may help to assist the upstroke phase of the pedal rotation by the sound leg. In fact, prolongation of exercise time resulted in a twofold increase in work rate at peak exercise via two-legged pedal cranking because of the fitted HP with motion of both the prosthetic left leg and the sound right leg compared with one-legged pedal cranking without the fitted HP (Table 1 & Figure 2C). It was clear that energy consumption required to reach an exhausted state with leg fatigue (Borg scale 15, hard) in all exercise models should not be theoretically different because the active leg was only the sound right leg. It was evaluated that the passive motion of the prosthetic leg only contributed to elevating the work rate by 8W with a slight increase of 2.54 ml/kg/ min corresponding to 0.73 METs by comparison between HPon+ and HPon- (Table 1). Because the passive prosthetic leg has no metabolic activity, a slight increase in oxygen consumption was expected because increasing work levels by muscles in the sound leg as well as trunk and/or forearm. In this case, counter passive pedal cranking by the prosthetic leg accompanying pedal rotation by the sound leg may improve exercise performance. Moreover, the role of stability due to the pelvic socket during passive motion of the prosthetic leg may be beneficial for rhythmic two-pedal cranking during aerobic exercise.
Application for aerobic two-legged ergometer exercise using a fitted prosthetic leg HP for physical therapy
Aerobic exercise with endurance physical training may be benefit for the improving walking ability [25,26] and cardiovascular function and in particularly in amputees with comorbidities such as hypertensive state, dyslipidemia, and diabetes mellitus. According to a previous study in limb amputees, walking ability was lower for hip disarticulation (range:117-162m in 3 subjects) than transfemoral amputees (203m in 1 subject) as measured using a 2-min walk test [27], which was approximately half the distance that a healthy person completed. This means that gait impairment after hip disarticulation may reduce physical fitness [5], thus it is still critical issue for limitation for dynamic and endurance exercises, such as running and/or cycle ergometer exercise for hip disarticulation/ hPV amputees even if an HP was fully fitted. In previous studies, one-legged cycling tests driven by the sound limb have been useful for the determination of AT in lower limb amputees, including trans-femoral, trans-tibial, and hip disarticulation amputees [28,29]. Furthermore, in trans-femoral amputees, the effectiveness for aerobic one-legged CERx training at a target HR corresponding to an AT level for 30min per day for 3-5 days each week for 6 weeks was demonstrated with significant increases in AT of 36.5% and in VO2max of 26.0% [30]. One-legged CERx in the above-mentioned studies may be an optimal exercise model for increasing exercise tolerance with AT; however, this evaluation was only for soundleg exercise not for two-legged cycling using a prosthetic leg with natural performance with cranking exercise for both pedals although the exercises were predominantly by the sole sound leg. Thus, it is still necessary to consider what type of exercise model may be better for daily physical activity in hip disarticulation/hPV amputees.
More than 86% of the predicted maximum HR achieved at the end of exercise (Borg scale 15) was valid to estimate exercise tolerance at a relatively heavy work rate. In Table 1, the peak VO2 in the three different exercise model were in a range between 12.02 and 14.56ml/kg/min, which was similar to previously measured values from one-legged cycling in a supine position in 7 hip disarticulation amputees (age: 61-73 years, 6 female and 1 male, and VO2peak range: 13.9-20.5ml/kg/min) [16]. In addition, the percentage of presumed VO2max of between 78% and 85% in the three different exercise models was also relatively high within the individual; however, the relative value of age standardized VO2max was in a range between 46% and 56%. The changes in increasing VO2 with two-legged CERx using a fitted HP were slight compared with that for one-legged CERx with or without a fitted HP; however, with two-legged CERx it may be possible to significantly extend the exercise time. Because RER determined as VCO2/VO2 for both HPonand HPon+ was above 1.0 at peak-exercise, the AT point may also be evaluated for exercise programs for physical therapy, although the AT point was not evaluated for HPoff (Table 1 & Figure 3). Analyzing various parameters may be advantageous for presenting objective baseline data for exercise program development. The actual value of 3.14 METs achieved at the AT point in two-legged CERx (HPon+) was valuable information for the present amputee who weighed over 100kg. Because it is relatively easy to reach high energy consumption when performing steady-state CERx for as long as possible (for example more than 20 min at AT level) with less (reduced) load from the body weight in a sitting posture on a saddle instead of the HP limiting standing/walking distance and speed.
Finally, a previous study reported that the wearing rate of HP is low, and the number of people using them is less than 50% of patients who are eligible for an HP [12]. In geriatric amputees including hip disarticulation the ability to stand on one leg, motivation for walking and adequate physical fitness allowing an exercise intensity of ≥50%VO2max were good predictive factor for successful prosthetic therapy [26]. Therefore, daily habitual twolegged CERx using a fitted prosthetic leg HP may be a useful exercise model for improving the HP wearing rate via behavior modification for physical fitness to maintain exercise tolerance.
Conclusion
The present case demonstrated that pedal cranking can be a familiar exercise for HD/hPV amputees. A temporary Canadian HP and its prosthetic leg providing two-legged CERx can be used to determine exercise tolerance in cardiopulmonary exercise tests. Furthermore, the prosthetic leg passively assisted pedal rotation generated by the sound leg during CERx allowing extension of the exercise time. Use of the pelvic socket may be effective in increasing stability on the saddle during pedal rotation by the sound leg in an upright posture. Amputees have potentially large variations in walking ability, remaining physical fitness, the effects of age, muscle mass/strength in the unilateral healthy leg, instability in postural control, phantom limb, anxious mental state related the change in body image, and comorbidities related chronic metabolic, kidney, and/or cardiovascular disease and chemotherapy for progressive malignant tumors. Thus, the role of exercise therapy should be discussed in initial evaluations of physical fitness, which can provide important information for determining exercise models in rehabilitation programs for enhancement of daily and social living activity with or without an HP.
Acknowledgments
The first author acknowledges the support of the late professor emeritus Hisao Iwane (formerly Tokyo Medical College) and Bengt Saltin (CMRC in Denmark) for the initial work in environmental physiology and the current field in rehabilitation. The present case study was supported by a Scientific Research (C) general grant (No. 15K01730) and (No. 22K11431) from MEXT and JSPS (to T. Osada).
Conflicts of Interest
The author declares that there is no conflict of interest associated with this work.
References
- Sugarbaker PH, Chretien PB (1981) A surgical technique for hip disarticulation. Surgery 90(3): 546-553.
- Moura DL, Garruço A (2017) Hip disarticulation-case series analysis and literature review. Rev Bras Ortop 52(2): 154-158.
- Dénes Z, Till A (1997) Rehabilitation of patients after hip disarticulation. Arch Orthop Trauma Surg 116(8): 498- 499.
- Dillingham TR, Pezzin LE, MacKenzie EJ (2002) Limb amputation and limb deficiency: Epidemiology and recent trends in the United States. South Med J 95(8): 875-883.
- Gailledrat E, Moineau B, Seetha V, De Angelis MP, Saurel B, et al. (2013) Does the new Helix 3D hip joint improve walking of hip disarticulated amputees? Ann Phys Rehabil Med 56(5): 411-418.
- Eijk MS, Linde HV, Buijck BI, Zuidema SU, Koopmans RT (2012) Geriatric rehabilitation of lower limb amputees: A multicenter study. Disabil Rehabil 34(2): 145-150.
- Osada T, Ishiyama M, Ueno R (2022) Multiple sessions of one-legged recumbent cycle ergometer exercise improved pedaling rate and knee range of motion in a middle-aged man after hip disarticulation: A clinical case. J Phys Med Rehabil Stud Rep 4(4): 1-13.
- Osada T, Ishiyama M, Ueno R (2018) Time-course of thigh muscle contraction-induced blood flow magnitude in amputated lower limb with prosthesis during dynamic knee extensions: A case study. Phys Ther Rehabil 5: 21.
- Osada T, Ishiyama M, Ueno R (2019) Voluntary thigh muscle strength with resection stump-dependent blood flow and vasodilation in an amputated lower leg with total surface bearing prosthesis during dynamic knee extensor: A case trial. Open J Ther Rehabil 7(4): 151-169.
- Osada T, Ishiyama M, Ueno R (2021) Variations in knee range of motion during repeat knee extension with an amputated lower leg at different contraction rhythms over 8 consecutive days in a patient with severe diabetic neuropathy: A clinical study. Int J Sports Med Rehabil 4: 23.
- Wakelin SJ, Oliver CW, Kaufman MH (2004) Hip disarticulation-the evolution of a surgical technique. Injury 35(3): 299-308.
- Van der Waarde T, Michael J (1992) Prosthetic management. In: American Academy of orthopaedic surgeons. Atlas of Limb Prosthetic Surgical, Prosthetic, and Rehabilitation Principles, 2nd (edn.), Mosby-Year Book, USA, pp. 539- 552.
- Nowroozi F, Salvanelli ML, Gerber LH (1983) Energy expenditure in hip disarticulation and hemipelvectomy amputees. Arch Phys Med Rehabil 64(7): 300-303.
- Shurr DG, Cook TM, Buckwalter JA, Cooper RR (1983) Hip disarticulation: A prosthetic follow-up. J Am Orthotic Prosthet Assoc 37: 50-57.
- McAnelly RD, Refaeian M, O’Connell DG, Powell GD, Walsh NE (1998) Successful prosthetic fitting of a 73-year old hip disarticulation amputee patient with cardiopulmonary disease. Arch Phys Med Rehabil 79(5): 585-588.
- Chin T, Kuroda R, Akisue T, Iguchi T, Kurosaka M (2012) Energy consumption during prosthetic walking and physical fitness in older hip disarticulation amputees. J Rehabil Res Dev 49(8): 1255-1260.
- Zalavras CG, Rigopoulos N, Ahlmann E, Patzakis MJ (2009) Hip disarticulation for severe lower extremity infections. Clin Orthop Relat Res 467(7): 1721-1726.
- Unruh T, Fisher DF Jr, Unruh TA, Gottschalk F, Fry RE, et al. (1990) Hip disarticulation. An 11-year experience. Arch Surg 125(6): 791-793.
- Iwasa S, Uchiyama Y, Kodama N, Koyama T, Domen K (2021) Regaining gait using an early postoperative hip prosthesis: A case report of an elderly women. Prog Rehabil Med 6: 20210011.
- Yoshikawa K, Mutsuzaki H, Sano A, Kiguchi N, Shimizu Y, et al. (2019) A case of an elderly hip disarticulation amputee with rheumatoid arthritis who regained the ability to walk using a hip prosthesis. J Phys Ther Sci 31(4): 366-370.
- Kawaguchi T, Yamada T, Iwashita K (2023) Biomechanical gait analysis for a hip disarticulation prosthesis: Power source for the swing phase of a hip disarticulation prosthetic limb. J Phys Ther Sci 35(5): 361-365.
- Burns KJ, Pollock BS, LaScola P, McDaniel J (2014) Cardiovascular responses to counterweighted single-leg cycling: implications for rehabilitation. Eur J Appl Physiol 114(5): 961-968.
- Ericson MO, Nisell R, Arborelius UP, Ekholm J (1985) Muscular activity during ergometer cycling. Scand J Rehabil Med 17(2): 53-61.
- Ericson MO, Bratt A, Nisell R, Arborelius UP, Ekholm J (1986) Power output and work in different muscle groups during ergometer cycling. Eur J Appl Physiol Occup Physiol 55(3): 229-235.
- Wezenberg D, Haan A, Woude LHV, Houdijk H (2012) Feasibility and validity of a graded one-legged cycle exercise test to determine peak aerobic capacity in older people with a lower-limb amputation. Phys Ther 92(2): 329-338.
- Hamamura S, Chin T, Kuroda R, Akisue T, Iguchi T et al. (2009) Factors affecting prosthetic rehabilitation outcomes in amputees of age 60 years and over. J Int Med Res 37(6): 1921-1927.
- Moineau B, Boisgontier MP, Gailledrat E, DeAngelis MP, Olivier I, et al. (2015) Is standing postural control more impaired in young patients with hip-disarticulation than transfemoral amputation? A pilot study. Ann Phys Rehabil Med 58(6): 354-356.
- Chin T, Sawamura S, Fujita H, Nakajima S, Ojima I, et al. (1997) The efficacy of the one-leg cycling test for determining the anaerobic threshold (AT) of lower limb amputees. Prosthet Orthot Int 21(2): 141-146.
- Chin T, Oyabu H, Maeda Y, Takase I, Machida K (2009) Energy consumption during prosthetic walking and wheelchair locomotion by elderly hip disarticulation amputees. Am J Phys Med Rehabil 88(5): 399-403.
- Chin T, Sawamura S, Fujita H, Nakajima S, Ojima I, et al. (2001) Effect of endurance training program based on anaerobic threshold (AT) for lower limb amputees. J Rehabil Res Dev 38(1): 7-11.
© 2023 Takuya Osada. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






