- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
Effects of an Exercise Program on Risk Factors for Cardiovascular Diseases: Retrospective Cohort
Bruna Eibel*
Cardiology Institute of Cardiology of RS - University Foundation / IC-FUC, Brazil
*Corresponding author:Bruna Eibel, Cardiology Institute of Cardiology of RS – University Foundation / IC-FUC, Avenida Princesa Isabel - 370, Santana, 90.620.001. Porto Alegre, RS - Brazil
Submission: August 16, 2023; Published: September 28, 2023

ISSN 2637-7934 Volume4 Issue4
Abstract
Introduction: Cardiovascular diseases are the main cause of mortality worldwide and can be prevented with strategies of control for modifiable risk factors. Objective: Verify the effect of an exercise program on modifiable risk factors for cardiovascular diseases. Design: Retrospective cohort study. Setting: Cardiopulmonary and metabolic rehabilitation center. Participants: Developed through the analysis of data from medical records from 2012 to 2018. Main outcomes measures: The proposed protocol was 30 sessions of aerobic exercise on a treadmill. The behavior of blood pressure, Body Mass Index (BMI), functional capacity (Six-Minute Walk Test- 6MWT), peripheral muscle strength (Chair-Stand Test-CST), exercise capacity (distance covered on the treadmill) was extracted from the medical records pre and post program. Results: The sample consisted of 83 subjects, hypertensive stage 1 (Systolic Blood Pressure- SBP 131.96±16.41mmHg; diastolic blood pressure- DBP 80.22±12.18mmHg) and obese BMI (30.66±5.37Kg/m2). After 30 sessions of aerobic exercise, subjects decreased blood pressure values (SBP: 117.73±12.28mmHg; DBP 69.89±10.83mmHg; p≤0.00), characterized as normal. There was also a slight non-significant decrease in body weight and BMI (30.48±5.48Kg/m2). The functional capacity improved (6MWT: 473.82±87.78 meters to 516.48±82.92 meters; p≤0.00), as well as the distance covered (2.001,45±437.23 meters to 2.931,45±353.44 meters; p≤0.00) and in the CST (12.40±3.61 to 14.66±3.29; p≤0.00). Conclusion: The protocol performed in this study demonstrated efficacy in the reduction of blood pressure, improving functional capacity, peripheral resistance and exercise capacity.
Keywords:Exercise; Cardiac rehabilitation; Physical therapy
Introduction
Cardiovascular Diseases (CVDs), for the most part, can be prevented with control strategies for modifiable risk factors [1]. Among these risk factors, overweight and obesity have a negative impact on cardiac structure and function, as well as being responsible for several central and peripheral hemodynamic changes. Weight gain is related to increased total and central blood volume, insulin resistance, decreased systemic vascular resistance, increased left ventricular and pulmonary artery filling pressures [2]. As a consequence of these risk factors, Systemic Arterial Hypertension (SAH) has an association in hemodynamic changes and other systemic compensatory mechanisms. The combination of obesity and SAH, causes neuro-humoral and metabolic abnormalities that lead to remodeling and cardiac dysfunction [3]. SAH is often associated with functional and structural dysfunctions of target organs, being aggravated by other risk factors such as dyslipidemia, obesity, glucose intolerance, and Diabetes Mellitus (DM). Hypertensive patients with CVD present a high risk of mortality, maintaining a continuous relation with ischemic events [4,5]. One of the preventive measures is to treat modifiable risk factors, such as hyperglycemia, hyperlipidemia, blood pressure control, smoking, alcohol consumption, sedentary lifestyle and poor diet, which may reduce the risk of CVD [6]. It is known that physical exercise is part of non-pharmacological measures and is the main component for primary prevention CVDs [7]. Cardiac rehabilitation programs with aerobic exercises are indicated both in the prevention and treatment of hypertension (recommendation IA) [8]. However, the impact of an exercise program in a population without previous cardiovascular events and without surgical interventions is scarce. Thus, the objective of this study was to verify the effect of a cardiac rehabilitation program on hypertension, overweight and functional capacity in individuals without previous cardiovascular events.
Methods
This is a retrospective cross-sectional study conducted in a Cardiopulmonary and Metabolic Rehabilitation Center, a reference institution in Cardiology in Rio Grande do Sul, Brazil. Approved by the Human Research Ethics Committee under opinion number 2.851.078 and in accordance with the Declaration of Helsinki. The individuals were selected through the analysis of medical records, from 2012 to 2018. Considering that data collection did not involve handling, approach, or interviewing patients and was restricted only to data collection in medical records, the informed consent form was waived for the present study. The study included individuals who performed an exercise program to control risk factors in CVD and who presented complete data in medical records. These risk factors included patients with hypertension, dyslipidemia, overweight, DM, sedentary, smoker or former smokers, alcoholics or former alcoholics, as well as family history of heart disease. The medical records of individuals with a history of a previous cardiovascular event, such as acute myocardial infarction, angina pectoris, stroke, peripheral artery disease and/or heart failure, were excluded, as well as any cardiovascular surgery and/or invasive therapy with percutaneous revascularization by angioplasty.
From the analysis of the participants’ medical records, two of the modifiable risk factors for CVD were collected: Blood pressure and Body Mass Index (BMI). Blood pressure reference values were based on the American Heart Association’s new hypertension guideline, which defines hypertension as a resting systolic blood pressure (SBP) of ≥130mmHg and/or a resting diastolic blood pressure (DBP) of ≥80mmHg. Normal blood pressure is classified as SBP<120mmHg and DBP<80mmHg [6]. For the evaluation of BMI, weight and height data were collected and their reference values were related to age. For individuals between 18 and 60 years of age, it is classified as overweight when BMI between 25 and 29.9kg/m², obesity grade I from 30 to 34.9kg/m², obesity grade II from 30 to 39.9kg/m² and grade III obesity of ≥40kg/m² [9]. For those over 65 years old, BMI is considered to be between 22 and 27kg/m² and excess weight 27kg/m² [10].
We collected the data before and after Cardiopulmonary and Metabolic rehabilitation, to asses functional capacity used data of the six-minute walk test (6MWT) according to the standards proposed by the American Thoracic Society [11], and the 30 seconds Chair-Stand Test (CST) to assess lower limb muscle strength [12]. During the first and last session of the exercise program, data regarding the distance covered on the treadmill were collected. Aswell, clinical evaluation and medications were collected. The rehabilitation program consisted of aerobic exercise on a treadmill, with intensity ranging from 50% to 80% of your training heart rate. The duration of the sessions was 45 minutes, being 6 minutes of initial stretching and 6 minutes of final stretching. The training frequency was performed 3 times a week, during 30 sessions. In order for the patient to have a continuity in the rehabilitation, it was not allowed to miss 3 consecutive sessions, and if it happened the patient should be removed from the protocol. If it was necessary to recover a session, it was added to the end of the rehabilitation. The sample did not present referred osteoarthritis or functional limitations, therefore, everyone was able to perform on treadmill.
The analyses were performed using SPSS software version 25. The qualitative variables were presented as absolute number and frequency and the quantitative variables as mean and standard deviation. Normality was tested through the Shapiro-Wilk test. To compare pre- and post-intervention means, we used paired Student’s t-test for parametric measurements. The significance level adopted was 5%.
Result
A total of 150 medical records were selected consecutively, of which 83 patients were included in the study. The mean age was 63.35±10.43 years with a predominance of females and the most prevalent cardiovascular risk factor was hypertension. The most commonly used medications were simvastatin (50.6%), losartan (34.9%) and acetylsalicylic acid (34.9%). Table 1 shows the characteristics of the sample, risk factors and medications. In the initial evaluation, the individuals were classified as overweight and there was a decrease in body weight and BMI after the exercise program, but without significant difference. The values of SBP and pre-rehabilitation DBP were compatible with individuals in stage 1 hypertension, who reduced considerably after the program and changed the classification to normal stage, not hypertensive (p≤0.00), as shown in Table 2. The functional tests performed before and after rehabilitation are shown in Table 3. The participants showed an increase in the distance achieved in the 6MWT after the exercise program, suggesting improvement of functional capacity (p≤0.00), although they reached a distance greater than predicted in the first evaluation (105% of predicted). In CST, individuals also presented improvement of the strength of lower limbs demonstrated by the increase in the number of repetitions (p≤0.00).
Table 1:Clinical profile of individuals prior to cardiopulmonary and metabolic rehabilitation on exercise treadmill during 2012-2018.
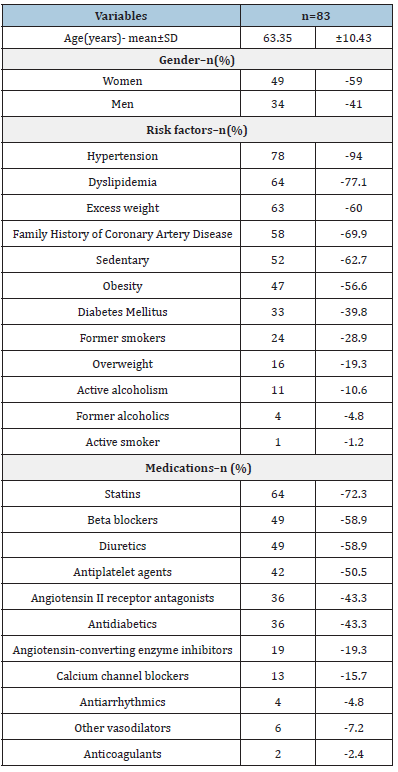
Source: Values are described as mean and Standard Deviation (SD); Absolute number and frequency (percentage).
Table 2:Risk factors pre and post cardiopulmonary and metabolic rehabilitation program using a treadmill during 2012-2018.
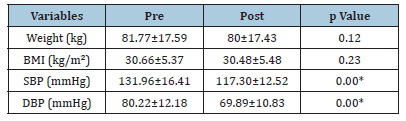
Source:BMI: Body Mass Index; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; Values are described as mean and standard deviation; *p<0.05
Table 3:Assessments and distance covered pre and post cardiopulmonary and metabolic rehabilitation program using a treadmill during 2012-2018.
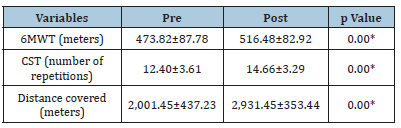
Source:6MWT: six-minute walk test; CST: Chair-Stand Test; Values are described as mean and standard deviation; *p<0.05.
In relation to the aerobic exercise program, the average distance covered in the first training session was 2,001.45 meters and in the last session showed a growth, reaching 2,931.45 meters, with significant result (p≤0.00) (Table 3). The behavior of blood pressure after aerobic exercise program was lower than the initial moment, which was demonstrated in the evaluation of the 6MWT before and after rehabilitation for SBP (p≤0.00) and DBP (p≤0.00). 6MWT 1 refers to the first walk test, before the intervention, with the respective SBP and DBP values before starting the test and after its completion. 6MWT 2 demonstrates these values after the exercise program (Table 4).
Table 4:Blood pressure behavior pre and post walk tests.
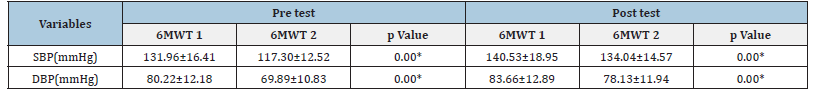
Source:6MWT 1: First 6-minute walk test; 6MWT 2: Second 6-minute walk test; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure. Values are described as mean and standard deviation; *p<0.05.
Discussion
This study evaluated the effect of an aerobic exercise program performed on a treadmill in a Reference center for cardiopulmonary and metabolic rehabilitation on modifiable risk factors for CVD. As expected, it brought reduction of SBP and DBP after 30 rehabilitation sessions. There was also a slight decrease, not significant, in weight and BMI. A high number of hypertensive individuals (94%) were observed. Data from the literature show that hypertension reaches 30% of the Brazilian adult population [13]. Hypertension combined with advanced age and other risk factors for CVD, such as atheroma plaques, may increase the risk of adverse events rather than comparing patients with hypertension alone [14,15]. In our data, there was also a high percentage of individuals with dyslipidemia (77.1%), sedentary (62.7%) and overweight (60%). The literature shows a significant relationship between sedentary behavior and higher incidence and mortality rates due to CVD. On the other hand, moderate to intense physical exercise is associated with the prevention or reduction of excessive weight gain and control of dyslipidemic levels [16,17]. Regarding the training protocol applied, it proved capable of reducing blood pressure, such results were also found in other studies that used a frequency of 3 times a week [18,19]. However, to reduce weight gain and BMI, a program with a longer follow-up period and at least 150 minutes of physical activity per week would be necessary, which may justify our sample of patients not having achieved a greater reduction [1]..
In addition to this lowering of blood pressure, individuals achieved an optimization of functional capacity with an increase in the mean distance of the 6MWT by 43 meters. This increment was also found in the study by Pérez et al. [20], who evaluated an aerobic exercise program not supervised for 4 months, with individuals with cardiovascular risk factors, resulting in an increase of 46 meters in the distance reached in the 6MWT. Studies have shown that an increase of distance in the 6MWT can be observed with a cardiac rehabilitation program, reducing risk factors, optimizing the quality of life and sensation of dyspnea in other populations [21,22].
In our results we observed an improvement of 930 meters in the distance achieved during the treadmill exercise, comparing the values of the first and last session. The study by Reich et al. [23], with a cardiac rehabilitation protocol in individuals with cardiovascular risk factors, showed in an increase in exercise capacity in the evaluation after exercise testing. Greater exercise tolerance over time is correlated with a better prognosis and few cardiac events. In relation to the results found in the CST, it was observed that the patients had a considerable increase of the muscular performance and resistance in the lower limbs. There is a large variation of the CST and its time of application [24], in our study we used an evaluation of 30 seconds, which was able to report a significant increase in pre- and post-rehabilitation measures. In a study with patients with chronic obstructive pulmonary disease, the results showed that the test with 30 seconds is reliable and presents acceptable agreement between examiners [25]. We consider the measurement bias as limitations, since we use data from medical records. In addition, a future follow-up study with a longer protocol would be necessary to verify possible changes in the BMI variable.
How can the results of this study be used in clinical practice?
Cardiopulmonary and metabolic rehabilitation can reduce risk factors for cardiovascular disease..
30 sessions of resistance exercise and treadmill training were effective to reduce blood pressure.
Cardiopulmonary and metabolic rehabilitation provided improvement functional capacity, strength and endurance in individuals at risk for cardiovascular diseases.
Conclusion
Our findings demonstrate that the protocol performed was effective in reducing SBP and DBP, increasing functional capacity verified by distance progression in the 6MWT, increasing strength of lower limbs by increasing the number of repetitions in the CST, in addition to the improvement in exercise capacity observed with the increase of the distance achieved on the treadmill. For the BMI variable, the rehabilitation protocol was not able to reduce its rates significantly.
Acknowledgment
The authors are grateful for the availability of the Rehabilitation Center for supporting.
References
- (2018) 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Department of Health and Human Services, pp. 1-779.
- Lavie CJ, Sharma A, Alpert MA, Schutter A, Lopez-Jimenez F, et al. (2016) Update on obesity and obesity paradox in heart failure. Progress in Cardiovascular Diseases 58(4): 393-400.
- Lavie CJ, Alpert MA, Ventura HO (2015) Risks and benefits of weight loss in heart failure. Heart Failure Clinics 11(1): 125-131.
- Williams B, Mancia G, Spiering W, Rosei EA, Azizi M, et al. (2018) 2018 ESC/ESH guidelines for the management of arterial hypertension. European Heart Journal 39(33): 3021-3104.
- Malachias MVB, Barbosa ECD, Martim JFV, Rosito GBA, Toledo JY, et al.(2016) 7th Brazilian guideline of arterial hypertension: Chapter 14 - hypertensive crisis. Arq Bras Cardiol 107(3): 79-83.
- Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, et al. (2018) Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of cardiology/American heart association task force on clinical practice guidelines. Hypertension 71(6): 1269-1324.
- Halewijn GV, Deckers J, Tay HY, Domburg R, Kotseva K, et al. (2017) Lessons from contemporary trials of cardiovascular prevention and rehabilitation: A systematic review and meta-analysis. International Journal of Cardiology 232: 294-303.
- Carvalho T, Milani M, Ferraz AS, Silveira AD, Herdy AH, et al. (2020Brazilian Cardiovascular Rehabilitation Guideline - 2020. Arq Bras Cardiol 114(5): 943-987.
- Brazilian Association for the Study of Obesity and Metabolic Syndrome/ABESO. Brazilian Obesity Guidelines 2016. 4th (edn.), Sao Paulo, pp. 1-188.
- Lipschitz DA (1994) Screening for nutritional status in the elderly. Prim Care 21(1): 55-67.
- American Thoracic Society (2002) ATS statement: Guidelines for the six-minute walk test. American Journal of Respiratory and Critical Care Medicine 166(1): 111-117.
- Jones CJ, Rikli RE, Beam WC (1999) A 30-s chair-stand test as a measure of lower body strength in community-residing older adults. Research Quarterly for Exercise and Sport 70(2): 113-119.
- Lima DF, Lima LA, Luiz OC (2017) Daily physical activity of Brazilian carriers of arterial hypertension: A transversal analysis. Colombia Médica 48(2): 1-6.
- Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, et al. (2014) Blood pressure and incidence of twelve cardiovascular diseases: Lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. The Lancet 383(9932): 1899-1911.
- Li W, Zhao J, Song L, Chen S, Liu X, et al. (2020) Combined effects of carotid plaques and hypertension on the risk of cardiovascular disease and all-cause mortality. Clinical Cardiology 43(7): 715-722.
- Salehi Z, Salehi K, Moeini M, Kargarfard M, Sadeghi M (2017) The effect of resistance exercise on lipid profile of coronary artery disease patients: A randomized clinical trial. Iranian Journal of Nursing and Midwifery Research 22(2): 112-116.
- Loureiro NSL, Amaral TLM, Amaral CA, Monteiro GTR, Vasconcellos MTL, et al. (2020) Relationship between anthropometric indicators and risk factors for cardiovascular disease in adults and older adults of Rio Branco, Acre. Revista de Saude Publica 54: 24-71.
- Schroeder EC, Franke WD, Sharp RL, Lee DC (2019) Comparative effectiveness of aerobic, resistance, and combined training on cardiovascular disease risk factors: A randomized controlled trial. PLoS ONE 14(1): e0210292.
- Ramos RM, Coelho-Júnior HJ, Prado RCR, Silva RS, Asano RY, et al. (2018) Moderate Aerobic training decreases blood pressure but no other cardiovascular risk factors in hypertensive overweight/obese elderly patients. Gerontology and Geriatric Medicine 4: 1-8.
- Pérez FJR, Bonafonte LF, Guerediaga DI, Belaza MPO, Peyron PU (2017) Effect of an individualised physical exercise program on lipid profile in sedentary patients with cardiovascular risk factors. Clin Investig Arterioscler 29(5): 201-208.
- Chaves GSS, Ghisi GLM, Grace SL, Oh P, Ribeiro AL, et al. (2018) Effects of comprehensive cardiac rehabilitation on functional capacity in a middle-income country: A randomised controlled trial. Heart 105(5): 406-413.
- Mohammed HG, Shabana AM (2018) Effect of cardiac rehabilitation on cardiovascular risk factors in chronic heart failure patients. Egyptian Heart Journal 70(2): 77-82.
- Reich B, Benzer W, Harpf H, Hofmann P, Mayr K, et al. (2020) Efficacy of extended, comprehensive outpatient cardiac rehabilitation on cardiovascular risk factors: A nationwide registry. European Journal of Preventive Cardiology 27(10): 1026-1033.
- Vaidya T, Chambellan A, Bisschop C (2017) Sit-to-stand tests for COPD: A literature review. Respiratory Medicine 128: 70-77.
- Hansen H, Beyer N, Frølich A, Godtfredsen N, Bieler T (2018) Intra-and inter-rater reproducibility of the 6-minute walk test and the 30-second sit-to-stand test in patients with severe and very severe COPD. International Journal of COPD 13: 3447-3457.
© 2023 Bruna Eibel. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






