- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
Inpatient-Rehabilitation in Times of the SARS-CoV2 Pandemic - Fears and Differences in Different Disease Patterns
Jonas Antek Koller1, Matthias Dreher1, Magdalena Tueg2, Juergen Koerber3, Ute Dederichs-Masius4, Thomas Wilde5 and Andreas Schwarting1,2*
1Department of Internal Medicine I, Division of Rheumatology and Clinical Immunology, University Medical Center of the Johannes Gutenberg University Mainz, Germany
2Rheumatology Center Rhineland Palatinate, Germany
3Oncological Rehabilitation, Hamm Clinic Nahetal, Germany
4Cardiology, Drei-Burgen-Clinic, Germany
5Psychosomatic Clinic, St. Franziska-Stift, Germany
*Corresponding author:Andreas Schwarting, Focus on Rheumatology and Clinical Immunology, University Medicine Mainz, Langenbeckstraße 1, 55131 Mainz, Germany
Submission: July 24, 2023; Published: August 25, 2023

ISSN 2637-7934 Volume4 Issue3
Abstract
Context: Shoulder injury is common even in asymptomatic athletes, but the estimated frequency varies between studies. Objective: To conduct a systematic review with meta-analysis to evaluate the frequency of shoulder pathologies seen on MRI in asymptomatic athletes. Methods: This systemic review was conducted in accordance to the preferred reporting items for systemic reviews and meta-analysis guidelines. Data sources: We searched three electronic databases (PubMed/MEDLINE, Web of Science, Embase) for studies reporting on frequency of asymptomatic shoulder pathology on MRI using the keywords “shoulder”, “asymptomatic”, “imaging” and “athlete” up until February 10, 2023. Study design: Meta-analysis of proportions. Level of evidence: 3 Data extraction: Data was extracted by 2 authors. Risk of bias assessment was conducted using a 12-item checklist adapted for frequency studies. Results: 19 studies with a total of 569 shoulders that underwent MRI analysis were included. The primary outcome of the study was the pooled frequency of shoulder pathology (rotator cuff, biceps, subacromial bursa, labrum, Acromioclavicular (AC) joint, humerus) on MRI. The overall pooled frequency estimate of shoulder pathology is as listed: Rotator cuff pathology at 46% (CI 26% to 67%), biceps tendon pathology at 5% (CI 1% to 19%), subacromial pathology at 53% (CI 29% to 76%), labral pathology at 29% (CI 14% to 52%), AC joint pathology at 28% (CI 14% to 48%), and humeral head pathology at 46% (CI 31% to 62%). From our random effects model subgroup analysis, athletes participating in overhead sport and elite athletes demonstrated higher frequency of shoulder pathology overall. Conclusion: Pooled summary estimates of the frequency of shoulder pathology on MRI in asymptomatic athletes ranged from 5.0% to 55.7%, with significantly higher frequency seen in higher level athletes and overhead sports. This confirms the hypothesis that there is a high frequency of asymptomatic shoulder pathology in asymptomatic athletes likely related to wear and tear on the shoulder. Registration: INPLASY (INPLASY202320108).
Keywords:Magnetic resonance; Imaging; Asymptomatic athletes; Frequency; Shoulder pathologies; Acromioclavicular; Subacromial bursa, Labrum; Swimming injuries
Introduction
Shoulder injury is common in athletes, particularly in overhead athletes. The shoulder is at high risk of overuse injury in overhead sports such as baseball, volleyball, tennis, and swimming because of the repetitive high loads and forces placed on the shoulder during sport. In baseball, 12 to 19% of injuries are located in the shoulder, and in swimmers, the frequency is as high as 23% to 38% of swimming injuries within a single year [1-3]. Because the shoulders of overhead athletes are subjected to repetitive motions and forces, the dominant shoulders of overhead athletes may be subject to more “wear and tear” than that of the nonathlete regardless of the presence of symptoms. Prior studies have discovered that athletes participating in overhead sports demonstrate structural changes that may predispose the athlete to an overuse shoulder injury [4]. Structural modifications to athletes’ shoulders as a result of participating in athletics, such as scapular position and glenohumeral rotation, have been discovered after a single season of play in Division I baseball players [5]. Overhead athletes also have a high frequency of scapular dyskinesis compared to their non-athlete cohort, which is a common risk factor associated with shoulder injury [6]. Again, findings differ by sport: baseball pitchers demonstrate a lack of scapular upward rotation, while swimmers demonstrate an increase in scapula anterior tilting [7,8]. Although many acute structural lesions that occur in the shoulder girdle resolve with time, these athletes may find themselves at risk for developing chronic shoulder pathology due to overuse and recurrent microtrauma [9-12]. However, although overhead athletes are at higher risk of shoulder injury and structural changes, not all shoulder pathology presents with shoulder pain.
MRI has been extensively utilized as part of the evaluation of shoulder pathology with great success. However, recent studies have discovered that many of the changes in pathology seen on advanced imaging correlate poorly with clinical symptoms, leading to a high false positive rate of shoulder pathology diagnosed on imaging. Prior studies evaluating MRI abnormalities in asymptomatic, nonathlete shoulders have found that up to 30 to 50% of subjects may demonstrate shoulder pathologies ranging from rotator cuff tears, labral tears, acromioclavicular joint pathology, and subdeltoid bursitis, with increasing incidence associated with age [13-16]. It is possible that in athletes with more “wear and tear” on their shoulder from participating in sports, similar rates of shoulder pathology on imaging may be seen with or without the presence of symptoms..
Unlike asymptomatic shoulder pathology diagnosed incidentally on the non-athlete, aging population, asymptomatic shoulder pathology seen in athletes has not only an identifiable exacerbating factor (“wear and tear”) but may also be indicative of an increased risk of (symptomatic) shoulder injury in the future. Although the presence of asymptomatic shoulder pathology does not necessarily suggest that an injury is inevitable, it may suggest that certain biomechanics and imbalances in the supporting muscles of the shoulder may be improved to prevent injury as an athlete continues with their sport. Therefore, the purpose of this systemic review and meta-analysis is to determine a reliable estimate of the frequency of asymptomatic shoulder pathology seen on advanced imaging (MRI) in the athlete population. The analysis will also explore if there are factors that predict an increased frequency of shoulder pathology in the athlete population.
Methods
Search strategy and selection criteria
This systemic review was conducted in accordance to the Preferred Reporting Items for Systemic Reviews and Metaanalysis (PRISMA) guidelines [17] and is registered with INPLASY (INPLASY202320108). Study investigators searched for studies reporting the frequency of MRI pathology in asymptomatic athletes’ shoulders in three electronic databases (PUBMED/ Medline, Embase, Web of Science) with various expansions (searching “baseball”, “swimming”, “tennis”, etc., in lieu of “athlete”). Articles from all dates up to February 10, 2023 were eligible for inclusion. The searches combined terms related to the shoulder, asymptomatic, MRI, pathology, sports without language restrictions and were adjusted according to database specifications.
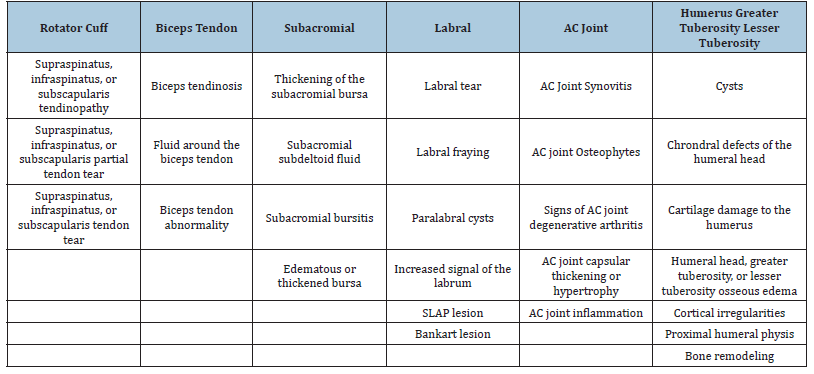
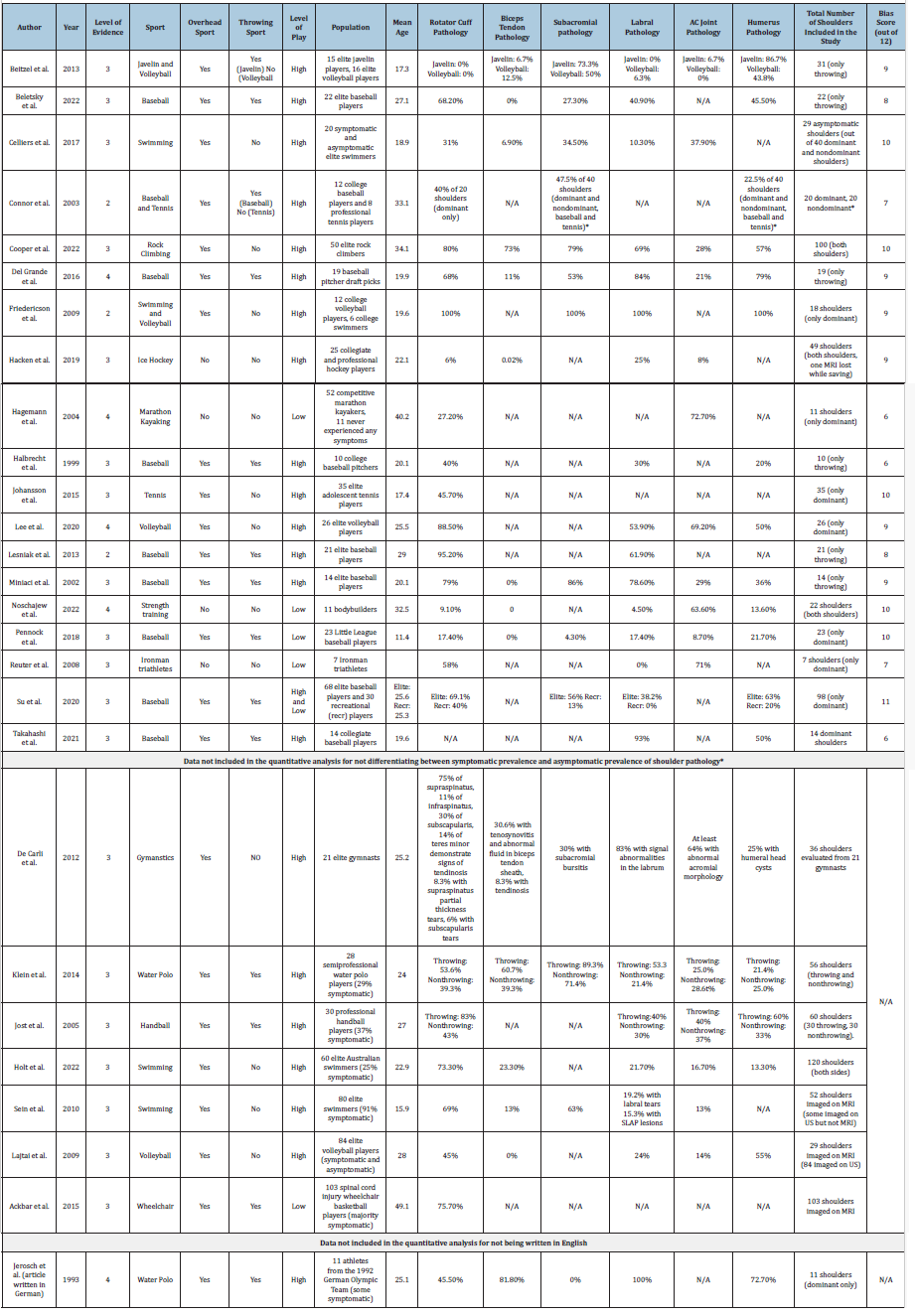
Primary outcomes were frequency of shoulder pathology seen on MRI divided into 6 categories: (i) rotator cuff pathology; (ii) biceps tendon pathology; (iii) subacromial fluid; (iv) labral pathology; (v) acromioclavicular (AC) joint pathology; (vi) humeral head or greater tuberosity pathology. We performed subgroup analysis to examine difference in frequency between level of competition (high and low) and sport (overhead or non-overhead). Two authors (CH, SS) independently assessed all titles and abstracts of identified reports for eligibility. Full texts were then reviewed for eligibility of inclusion in the study. The same authors crossreferenced and reviewed citations in the aforementioned eligible studies for additional eligible publications. Please see Table 1 for the full inclusion and exclusion criteria. Please see Table 2 for case definitions for shoulder pathology by anatomical category.
Table 1:Inclusion and exclusion criteria.
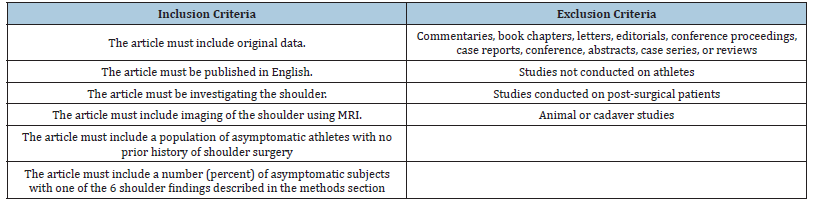
Table 2:Case definitions for shoulder pathology.
Data extraction
The following information was independently extracted from the included studies by two investigators (CH, SS): number of asymptomatic shoulders evaluated, age, sport, level of sport, and frequency of the 6 shoulder pathologies in dominant shoulder and non-dominant shoulders. In studies evaluating throwing shoulders, data from dominant shoulders was extracted while data from nondominant shoulders were excluded, as the majority of the studies evaluating asymptomatic pathology in dominant shoulders utilized the nondominant shoulder as a control. In studies where data for throwing and nonthrowing arms were not differentiated, the data was not included in order to maintain consistency. In studies evaluating nonthrowing sports (such as swimming, rock climbing, kayaking), all shoulders evaluated in the study were included in the data since both shoulders are utilized significantly in the sport and therefore, cannot be used as a control. For shoulder pathology that included multiple diagnoses that fall under the same category (for example, greater tuberosity cortical irregularities and lesser tuberosity cortical irregularities), the largest number percentage for frequency was utilized to maintain consistency between studies and avoid utilizing different pathology in the same athlete multiple times in the same category. Discrepancies were double-checked and verified by the authors (CH and SS).
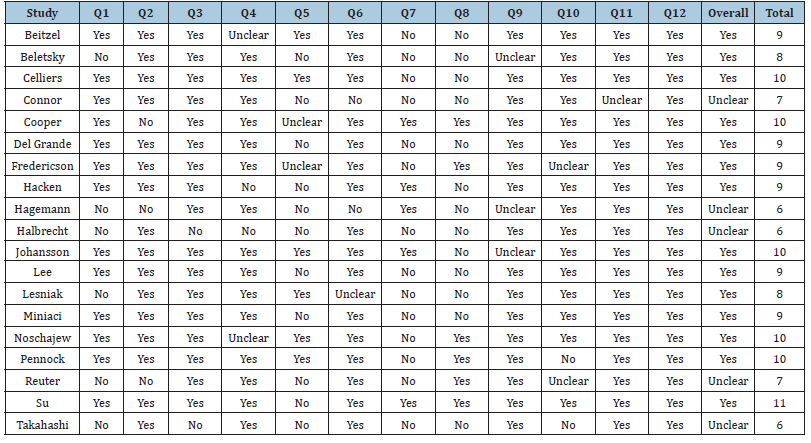
Risk of bias assessment
Three reviewers (CH, BL, KV) independently assessed risk of bias using a 12-item checklist developed specifically for this review that was adapted from Culvenor et al. [18], which was previously adapted from Downs and Black [18,19]. This 12-item checklist included assessing for duality of reporting, sample size and representation, distribution of confounders, and ascertainment of MRI diagnosis. This 12-item checklist customized using specific items from the downs and black checklist for randomized and non-randomized studies and a population-based frequency study checklist. Items related to randomization and intervention were not relevant to the current review, so were excluded from the bias study. Discrepancies were discussed with CH, BL, and KV and resolved with discussion (Table 3).
Table 3:Risk of bias summary table.
Data synthesis and analysis
The data analysis was conducted in R 4.2.2 (2022). Frequency estimates of the primary outcomes were calculated by pooling the study-specific estimates using random-effects proportion metaanalysis. Pooled binomial proportion 95% confidence interval estimates for each of the shoulder pathologies were calculated. Participation in overhead sport was split into two groups: “overhead” for participation in overhead sport and “not overhead” for participation in a non-overhead sport. Level of play was also split into 2 groups: “elite” level being collegiate and professional play, and “not elite” level being youth, recreational, and recreational competitive. All analyses had a significance threshold of p<0.05. Between study heterogeneity was evaluated for each primary outcome using the I2 statistic [20]. Tests for subgroup differences was conducted using standard chi-square (X2) tests and the I2 statistic for between group heterogeneity.
Results
Study characteristics and quality assessment
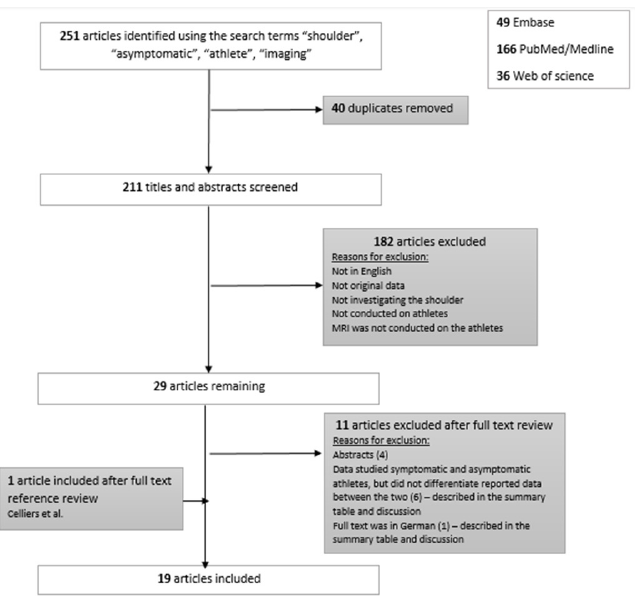
Fifteen cross-sectional studies and 4 longitudinal studies involving a total of 569 shoulders were included in this review. The mean number of shoulders evaluated per study was 43.6 (range 7 to 100 shoulders). The mean age was 25.0 (range 11.0 to 40.2). 480 shoulders included were from athletes who participated in overhead sports (84.4%). 89 shoulders came from athletes participating in non-overhead sports (15.6%). The majority (83.7%) of shoulders were from athletes studied competed at an elite level (college and profession). Out of a possible 12 points on the risk of bias scoring criteria, the mean score was 8.58. (See Table 4 for a comprehensive summary of the data) (Figure 1).
Table 4:Risk of bias analysis.
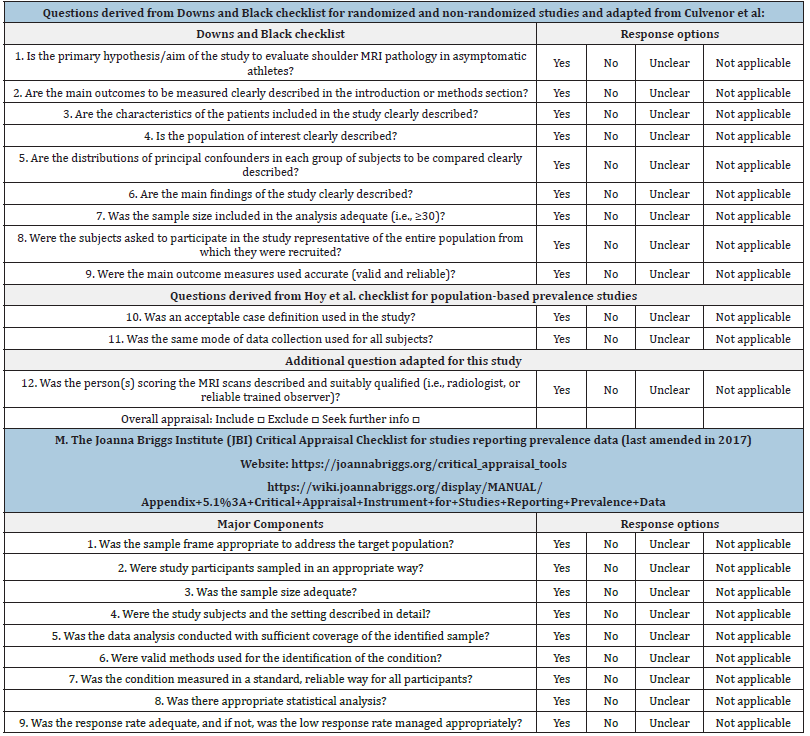
Figure 1:Flow diagram for identifying studies.
Frequency of rotator cuff pathology
Eighteen studies evaluated for frequency of rotator cuff pathology in asymptomatic athletes. Case definitions for rotator cuff pathology included rotator cuff tendinosis/tendinopathy and partial or full thickness tears (See Table 4 for complete descriptions of rotator cuff pathology seen on MRI). The overall pooled frequency estimate was 46% (95% CI 26% to 67%). A random effects model was used due to significant between study heterogeneity (I2=83%, p<0.01). Studies that included participation in overhead sport had a pooled frequency of 55% (95% CI 32% to 76%), compared to studies that included participation in non-overhead sport with a pooled frequency of 17% (95% CI 6% to 40%). Using a random effects model, there was a significant difference in frequency of rotator cuff pathology between overhead sport and non-overhead sports (X2=5.13, p<0.05) (See Figure 2). A similar analysis was conducted to compare elite athletes versus non-elite athletes, which demonstrated pooled frequency of 52.6% (95% CI 25.8% to 78.0%) and 28.3% (95% CI 15.7% to 45.6%) respectively. However, this difference was not significant (X2=2.90, p=0.09) (See Figure 3).
Figure 2:Forest plot by sport subgroup for rotator cuff pathology.
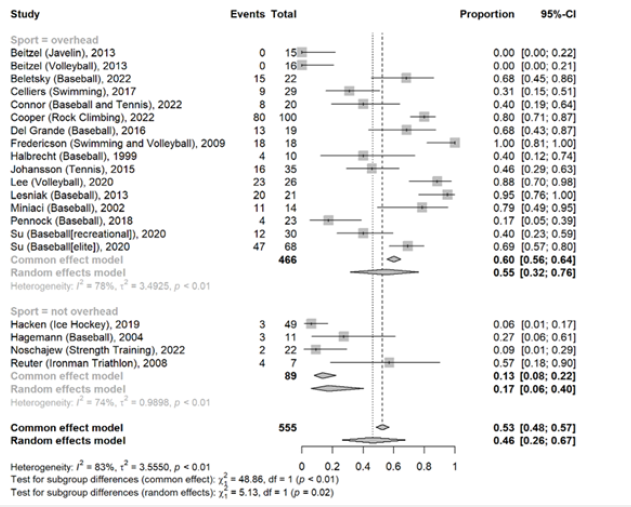
Figure 3:Forest plot by level subgroup for rotator cuff pathology.
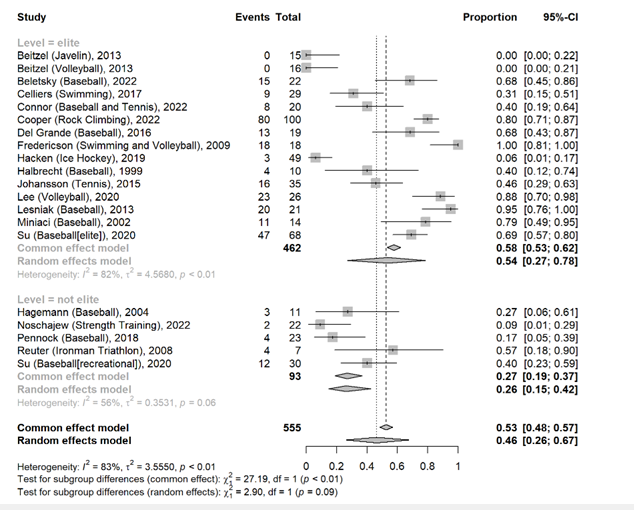
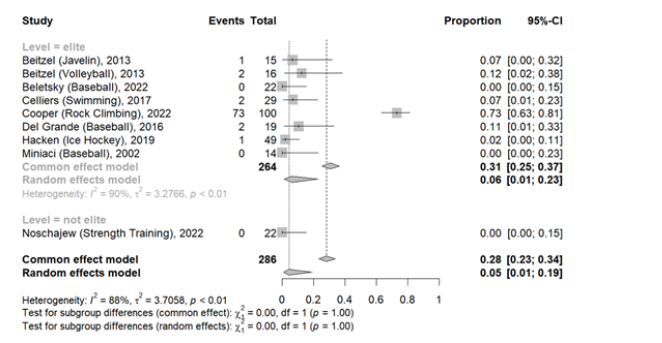
Frequency of biceps tendon pathology
Eight studies reported on the frequency of asymptomatic biceps tendon pathology. MRI analysis evaluated for evidence of biceps tendinosis/tendinopathy. The overall pooled frequency estimate for biceps tendon pathology was 5% (95% CI 1% to 19%). A random effects model was used due to significant between study heterogeneity (I2=88%, p<0.01). Studies that included participation in overhead sport had a pooled frequency of 8% (95% CI 2% to 30%), compared to studies that included participation in non-overhead sport with a pooled frequency of 1% (CI 0% to 9%). This difference was not significant (X2=1.78, p=0.18) (See Figure 4). Since there was only one study that investigated for biceps tendon pathology in non-elite athletes, a subgroup analysis by level of sport was not performed.
Figure 4:Forest plot by sport subgroup for biceps tendon pathology.
Frequency of subacromial pathology
Seven studies reported the frequency of asymptomatic subacromial bursitis on MRI. The overall pooled frequency estimate of subacromial pathology is 57% (95% CI 24% to 85%). A random effects model was used due to significant between study heterogeneity (I2=87%, p<0.01). Subgroup analysis for overhead sport was unable to be conducted, since all studies that reported frequency of asymptomatic subacromial pathology were conducted on overhead athletes. Studies that were conducted on elite athletes compared to non-elite athletes demonstrated a random effects model pooled frequency of 74% (95% CI 50% to 89%) and 9% (95% CI 4% to21%), respectively, which was significant (X2=21.53, p<.01) (See Figure 5).
Figure 5:Forest plot by level subgroup for biceps tendon pathology.
Frequency of labral pathology
Sixteen studies reported the frequency of asymptomatic labral pathology. Case definitions for labral pathology included labral signal abnormalities, tears, degeneration, and lesions (See Table 4 for complete descriptions of labral pathology seen on MRI in each study). The overall pooled frequency estimate of labral pathology is 29% (95% CI 14% to 52%). A random effects model was used due to significant between study heterogeneity (I2= 81%, p<0.01). Random effects subgroup analysis conducted on overhead athletes demonstrated a pooled frequency for labral pathology of 37% (95% CI 18%, 61%) compared to 10% (95% CI 2% to 38%). This relationship was not statistically significant (X2=2.73, p=0.10) (See Figure 6). Random effects subgroup analysis conducted on elite athletes demonstrated a pooled frequency of 38% (95% CI 21% to 59%) compared to 29% (95% CI 14% to 22%) in non-elite athletes. This relationship was statistically significant (X2=18.84, p<0.01) (See Figure 7).
Figure 6:Forest plot by level subgroup for subacromial pathology.
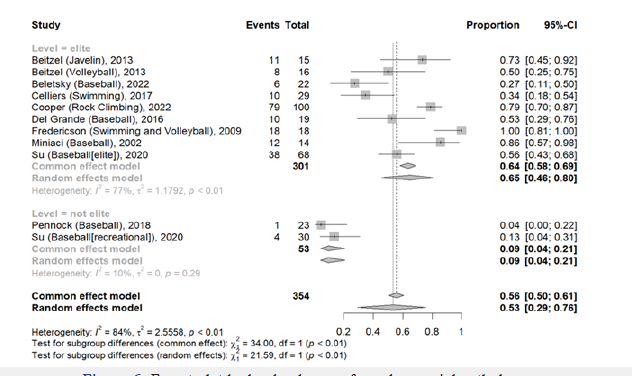
Figure 7:Forest plot by sport subgroup for labral pathology.
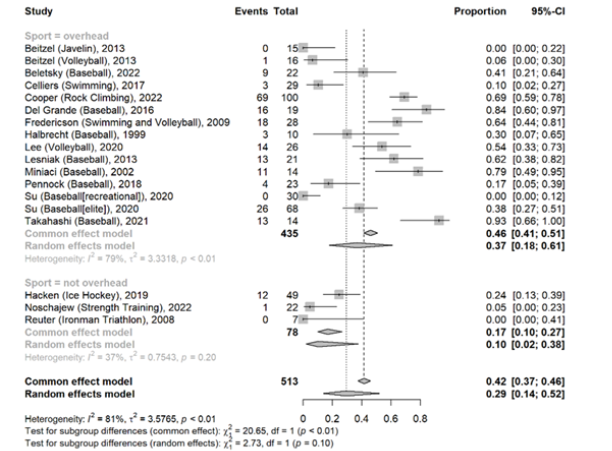
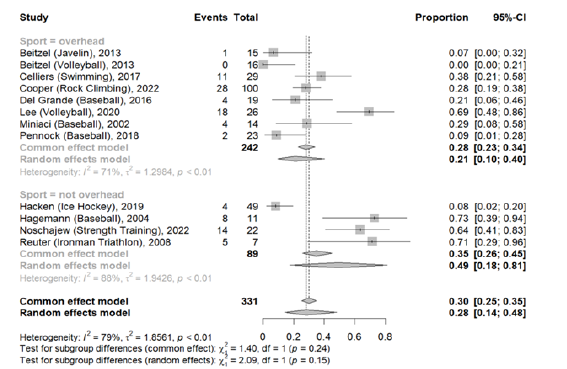
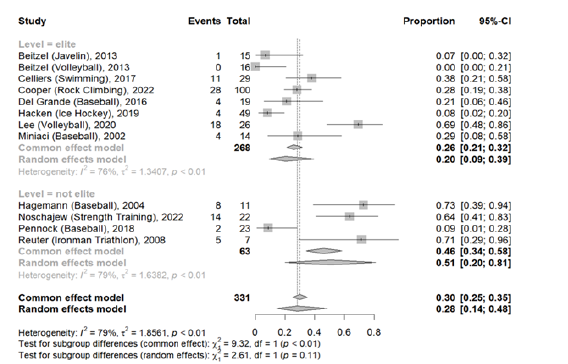
Frequency of AC joint pathology
Eleven studies reported the frequency of asymptomatic AC joint pathology. Case definitions for AC joint pathology included evidence of arthritis or arthrosis, joint hypertrophy, osteophytes, and inflammation (See Table 4 for complete descriptions of AC joint pathology seen on MRI in each study). The overall pooled frequency estimate of AC joint pathology is 28% (95% CI 14% to 48%). A random effects model was used due to significant between study heterogeneity (I2=79%, p<0.01). Random effects subgroup analysis conducted on overhead athletes demonstrated a pooled frequency of AC joint pathology of 21% (95% CI 10% to 40%) compared to 49% (95% CI 18% to 81%). This relationship was not statistically significant (X2=2.09, p=0.15) (See Figure 8). Random effects subgroup analysis conducted on elite athletes demonstrated a pooled frequency of 20% (95% CI 9% to 39%) compared to 51% (95% CI 20% to 81%) in non-elite athletes. This relationship was not statistically significant (X2=2.61, p=0.11) (See Figure 9).
Figure 8:Forest plot by level subgroup for labral pathology.
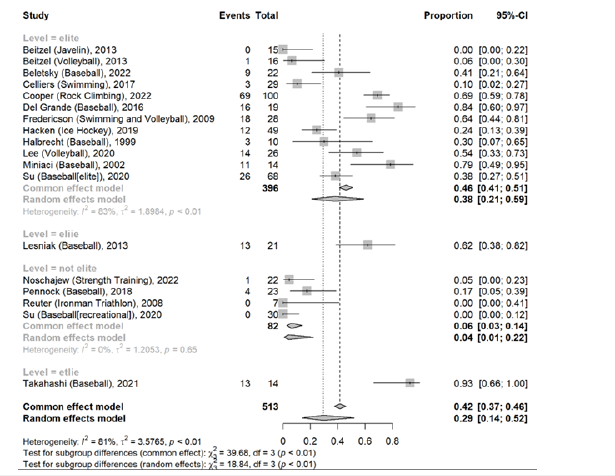
Figure 9:Forest plot by sport subgroup for ac joint pathology.
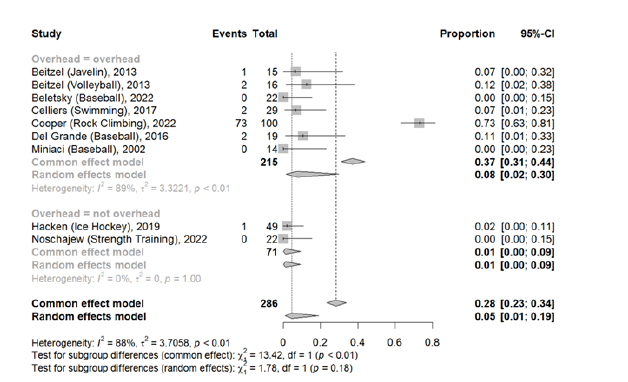
Frequency of humeral head pathology
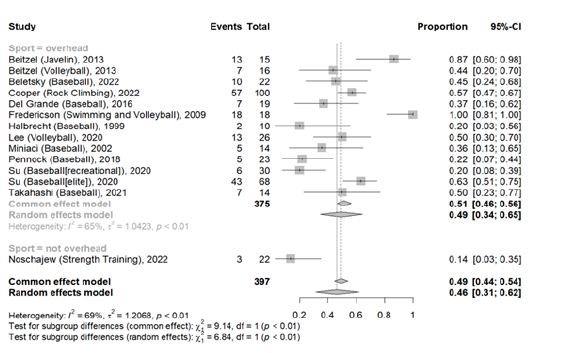
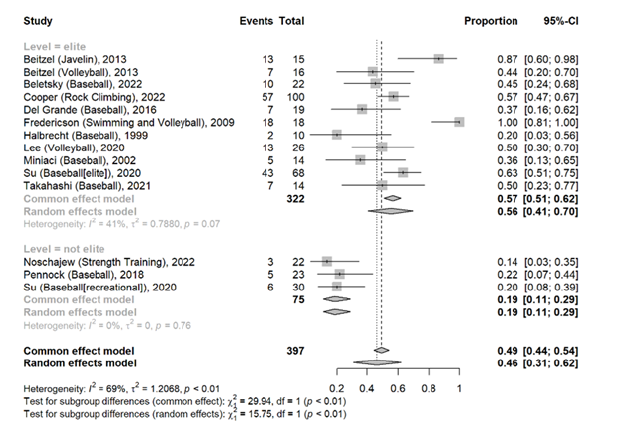
Twelve studies reported the frequency of asymptomatic humeral pathology. Case definitions for humeral head pathology included humeral head cysts, cartilage damage, osseous changes, and humeral head bone remodeling (See Table 4 for complete descriptions of humeral head pathology seen on MRI in each study). The overall pooled frequency estimate of humeral head pathology is 46% (95% CI 31% to 62%). A random effects model was used due to significant between study heterogeneity (I2=69%, p<0.01). Since there was only one study that investigated humeral head pathology in non-overhead sports, subgroup analysis conducted on overhead sports compared to non-overhead sports was not performed. Random effects subgroup analysis conducted on elite athletes demonstrated a pooled frequency of 56% (95% CI 41% to 70%) compared to 19% (95% CI 11% to 29%) in non-elite athletes. This relationship was statistically significant (X2=15.75, p<0.01) (See Figure 10).
Figure 10:Forest plot by level subgroup for ac joint pathology.
Discussion
This systematic review and meta-analysis of 19 studies involving 569 shoulders demonstrated that shoulder pathology on MRI is common in asymptomatic shoulders in athletes participating in a large variety of sports. The frequency of shoulder pathology on MRI is related to level of sport and type of sport. In elite athletes with higher training burden, the degree of wear and tear on the shoulder is expected to increase. This study’s results are consistent with this hypothesis, with the exception of pathology in the AC joint. Overhead athletes also demonstrated overall higher rates of shoulder pathology across all anatomical regions with the exception of the AC joint. Current literature notes AC joint pathology is more prevalent in strength training sports compared to overhead sports, which reflects our findings [21,22]. Overall, the data from this systematic review suggests an intensity related process of wear and tear on athletes’ shoulders. The following portion of the discussion will contain a summary breakdown of the evidence from this study, as well as similar studies in the literature that confirm this hypothesis.
Summary of evidence for shoulder pathology in asymptomatic athletes
Most of the evidence surrounding the presence of asymptomatic shoulder pathology in athletes is focused on athletes who play overhead sports. Although the studies are limited, the sports that have been investigated noted in the literature are baseball, tennis, gymnastics, volleyball, rock climbing, water polo, swimming, and strength training. In this conclusion, we summarized the findings from our systematic review and included a discussion with evidence from other similar studies that did not meet the inclusion criteria.
Baseball: Close to half of the studies included in this systematic review evaluated shoulder pathology in asymptomatic baseball players. Baseball pitchers place a particularly high level of force placed on the shoulder compared to the average athlete. The frequency of rotator cuff, subacromial, labral, and humeral pathology in baseball players was high, particularly in elite college and Major League baseball players. In addition to the data extracted on dominant shoulders of baseball players, several studies also evaluated shoulder pathology in the control, asymptomatic nondominant shoulders of baseball players to compare the frequency with that of the dominant shoulders. Miniaci et al. [23] have demonstrated a similar frequency in rotator cuff pathology between the two groups, but a significant difference between nonthrowing and throwing shoulders regarding pathology in the glenohumeral joint (like degenerative cysts of the humerus) [23]. However, this finding is not consistent between studies, since Halbrecht et al discovered that there was a significant difference in the frequency of rotator cuff pathology and labral pathology between throwing and nonthrowing arms in a study of 10 baseball players and concluded that MRI abnormalities are diagnosed at higher rates in asymptomatic throwing shoulders than in nonthrowing shoulders [24]. Pennock et al agreed with the findings discovered by Halbrecht et al; the dominant arm was 8.5 times more likely to have an abnormality on MRI compared with the nondominant arm, and 52% of players had positive findings on MRI in their throwing shoulder that were not present in their nondominant shoulder [25]. A similar study by Takahashi demonstrated that there was a high frequency of rotator cuff and subacromial pathology bilaterally, but dominant shoulders demonstrated more labral head and labral pathology [26].
One study conducted by Su et al. [27] investigated the frequency of shoulder pathology between professional baseball players compared to recreational baseball players and found that professional baseball players demonstrated increased rates of rotator cuff tears, labral lesions, subacromial/subdeltoid bursitis, and proximal humerus lesions compared to recreational players [27]. Overall, although the evidence does not completely agree on the type of shoulder pathology that is seen most commonly in baseball players, the evidence strongly supports that compared to the general population, baseball players tend to have a higher frequency of abnormalities in the labrum and humerus on MRI [23,27]. Whether or not these lesions suggest early, subclinical pathology or serve as a baseline for expected pathology in baseball players is yet to be determined.
Tennis: Tennis is an asymmetric sport that activates specific muscle patterns, particularly in the supraspinatus, infraspinatus, and teres minor muscles during the complex serving motion [28]. The studies conducted on asymptomatic tennis players are limited, but the data has demonstrated a high frequency of around 46% of rotator cuff pathology in the dominant shoulders of elite tennis players. Specifically, the major finding of the study conducted by Johansson [28] was that in their population of asymptomatic tennis players, there was a statistically significant increase in frequency of infraspinatus tendinosis in the dominant arm compared to the nondominant arm [28]. This may be because tennis players tend to develop an increase in internal rotation strength of their dominant shoulder at the expense of external rotation, which may lead to a decrease in infraspinatus strength, and subsequently, an increase in infraspinatus tendinopathy, as the primary action of the infraspinatus muscle is external rotation of the shoulder [29,30]. A different study investigated tennis and baseball players and demonstrated that rotator cuff pathology is more common in tennis players, while Bennett’s lesions were more common in baseball players, but did not differentiate between tennis players and baseball players regarding the other shoulder pathologies [31]. Therefore, it was difficult to draw conclusions specific tennis players based on data from the study [31]. However, the overall findings agree with the hypothesis that rotator cuff pathology may be more prevalent in tennis players with or without the presence of symptoms [28,31].
Swimming: Shoulder pain is the most common musculoskeletal complaint in competitive swimmers [32,33]. Competitive swimmers average a distance of 60 to 80km per week and 1.56 million overhead rotations per year [34]. The repetitive motions of the swimming overhead strokes places significant stresses on the rotator cuff and glenohumeral joint of swimmers, resulting in the “swimmer’s shoulder” [34,35]. Prior studies have demonstrated that MRI changes of the shoulder in swimmers are similar to those found on MRI of nonathlete patients with painful clinical syndromes. In one study conducted by Sein et al. that was not included in our study that was conducted on majority symptomatic swimmers (91%), 84% of the swimmers had positive impingement sign and 69% demonstrated supraspinatus tendinopathy on MRI. This group of majority symptomatic, young swimmers (average age of 15.9) also had imaging findings of labral tears, abnormalities to the biceps tendon sheath, abnormal acromion shape morphology, thickening of the subacromial bursa and fluid, and acromioclavicular degeneration [35].
Celliers et al. [36] evaluated symptomatic and asymptomatic swimmers’ shoulders, which demonstrated that 86.2% of asymptomatic shoulders had abnormal MRI changes, with findings consistent for partial supraspinatus tear (45.5% in symptomatic shoulders compared to 20.7% in asymptomatic shoulders), subacromial fluid (45.5% versus 34.5%), AC joint arthrosis (36.4% versus 34.5%), biceps tendinosis (18.2% versus 6.9%), and increased signal of the labrum/labral tears (10% versus 10.3%) [36]. A more recent study published by Holt et al. [37] that was not included in this study included a population of 45 asymptomatic swimmers and 15 symptomatic swimmers (18 out of a total 120 shoulder were symptomatic) and demonstrated supraspinatus tendinopathy in 70% of shoulders and subscapularis tendinopathy in 77% of swimmers, along with evidence of biceps tendinopathy, labral tears, AC joint changes, and humerus osseus edema [37]. The study concluded that subscapularis and supraspinatus tendinopathy was the most common tendon abnormality identified in swimmers, with a statistically significant difference between swimmers and controls in the frequency of rotator cuff tendinopathy, as well as labrum and AC joint pathology. Pathology was not found to be a predictor of current pain [37]. Overall, the data confirms that rotator cuff tendon pathology is the most common finding in elite swimmers’ shoulders and is common in both symptomatic and asymptomatic swimmers. Since the presence of shoulder pathology on imaging may present premorbidly, care must be taken for overhead athletes at risk of overuse injury to prevent the development of injury.
Volleyball: Volleyball is another sport at high risk for overhead shoulder injury. In prior studies, it has been reported that approximately 25% of all volleyball injuries involve the shoulder [38]. This is largely due to the force placed on the shoulder joint and its surrounding structures involved with the overhead hitting motion [38]. In this review, we identified a study conducted by Lee et al. [39] on 26 elite volleyball players, which demonstrated that the majority (>50%) of elite volleyball players have asymptomatic findings of rotator cuff pathology, labral pathology, AC joint pathology, or humeral pathology on advanced imaging [39]. In the study conducted by Beitzel et al [40], 16 elite, younger volleyball players demonstrated lower frequency of shoulder pathology on imaging ranging from 0% frequency of rotator cuff pathology to 50% with evidence of subacromial pathology [40]. The difference between studies may be explained by a difference in mean age of the athletes evaluated (25.5 in the Lee study compared to 17.3 in Beitzel’s study) [39,40].
A similar study not included in our review was conducted on 84 symptomatic and asymptomatic volleyball players that also demonstrated a high frequency of shoulder pathology on MRI and ultrasound, particularly in the player’s dominant hitting shoulder [41]. The study found that 24% and 45% of hitting shoulders on ultrasound and MRI, respectively, demonstrated supraspinatus tendinopathy. The study reported no difference in frequency of pathology between symptomatic and asymptomatic volleyball players. Other notable findings included infraspinatus muscle atrophy in the hitting shoulder that was largely unrecognized by the players, and a significant difference between hitting and nonhitting shoulders with regards to labral abnormalities and greater tuberosity cortical irregularities [41]. These findings support the hypothesis that elite volleyball players also demonstrate high rates of asymptomatic shoulder joint pathology that does not necessarily limit their ability to participate in sport.
Water polo: Water polo is a sport that requires repetition of overhead movements associated with swimming as well as overhead throwing motions involved with throwing a ball. Therefore, it can be hypothesized that water polo players may demonstrate changes in the shoulder in patterns similar to other overhead athletes. The first study to investigate shoulder pathology in water polo players investigated 11 dominant shoulders from 11 athletes from the 1992 German Olympic water polo team (mean age 25.4). There were 5 cases of rotator cuff pathology; in all 5 cases the supraspinatus tendon was affected, and in three cases both the supra- and infraspinatus tendon were involved. In 9 cases, there were changes in the biceps tendon. All 11 shoulders demonstrated hypertrophy of the articular capsule and pathologic changes of the anterior glenoid labrum. Finally, osseous lesions of the humeral head were in discovered in 8 athletes [42]. There was no evidence of subacromial impingement.
A different study that was not included in this study investigated 28 symptomatic and asymptomatic water polo players, along with a control group of healthy volunteers [43]. Results demonstrated significantly more MRI abnormalities in the subscapularis and infraspinatus tendons and posterior labrum of throwing shoulders compared to nonthrowing shoulders and a significant difference compared with healthy volunteers. All throwing shoulders demonstrated pathologic findings on MRI, but only 8 (29%) of the shoulders were symptomatic. Despite these findings, the classic findings seen in overhead throwing athletes [44] (supraspinatus tendinopathy) was not seen in water polo players, and neither were findings common in swimmers (shoulder instability and supraspinatus tendinopathy) [45]. However, the findings evaluated in swimmers quoted by this study were conducted on symptomatic athletes, and therefore, cannot be accurately compared to this population, which included a population of symptomatic and asymptomatic polo players. The authors concluded that abnormal MRI findings in water polo players may not be suggestive of true clinical pathology and should be interpreted with caution [43].
Javelin: Similar to baseball, javelin athletes face heavy loads resulting from the overhead throwing motion. However, as opposed to baseball, javelin athletes are throwing heavier loads that baseball players and therefore, it is suspected that the shoulders of javelin players may be subject to even heavier loads [46,47]. One study included in this study investigated that hypothesis and found that out of the 15, young elite javelin players studied, there was a high frequency of subacromial pathology and humeral pathology (73.3% and 86.7%) respectively [40]. The authors concluded that the high frequency of humeral head pathology, most significantly intraosseous cysts of the humerus, may be representative of early signs of partial lesions of the rotator cuff tendons in these young athletes that do not yet present with clinical symptoms [40] (Figure 11).
Figure 11:Forest plot by sport subgroup for humeral head pathology.
Rock climbing: Rock climbing is an increasingly popular sport, but one that has a high frequency of overuse injuries. Despite the perceived risk associated with climbing, acute injuries are relatively rare, but shoulder injuries such as tendonitis, impingement, and biceps tendonitis are very common. The one study that has evaluated asymptomatic shoulder pathology in elite rock climbers demonstrated a high frequency of rotator cuff tears (80%), biceps tendinosis (79%), subacromial bursitis (79%), labral pathology (69%), and cartilage damage of the humerus (57%) [48]. The study concluded that rotator cuff tendinosis and labral pathology were identified in rates similar to those of baseball pitchers, but tendinopathy of the biceps tendon and cartilage pathology were seen at higher frequencies than baseball pitchers, water polo players, or volleyball players [48,49] (Figure 12).
Figure 12:Forest plot by level subgroup for humeral head pathology.
Marathon kayaking: Marathon kayaking is a less well-known sport, but an important one to address nonetheless. There are a large number of overuse injuries among kayakers seen by primary care doctors, sports medicine physicians, and orthopedic surgeons [50,51]. The one study in the literature that evaluated asymptomatic shoulder pathology in competitive marathon kayakers evaluated 52 symptomatic (22) and asymptomatic (30) kayakers and screened them for abnormal pathology on MRI [52]. The most common MRI abnormalities were acromioclavicular joint hypertrophy and acromial/clavicular spurs with subacromial bursa, supraspinatus tendonitis, and biceps tendonitis. Eleven asymptomatic kayakers demonstrated pathology on MRI despite not having symptoms. Statistical analysis demonstrated that there was no significant difference in pathology between symptomatic and asymptomatic shoulders with regards to imaging pathology. The study concluded that overuse injuries to the shoulder of marathon kayakers are common, with a high incidence of rotator cuff pathology and acromioclavicular pathology with or without symptoms [52].
Handball: Handball is a sport that is similar to baseball, and also requires the athlete to place a large amount of force on their throwing shoulder [44]. One study that was not included in this study investigated the presence of abnormal MRI findings in both symptomatic and asymptomatic throwing shoulders of 30 competitive professional handball players and 20 dominant shoulders of asymptomatic volunteers. The results demonstrated a higher frequency of abnormal MRI findings in throwing shoulders compared to nonthrowing and control shoulders. Although 93% of throwing shoulder had abnormal imaging findings, only 37% were symptomatic. Partial rotator cuff tears, most commonly in the supraspinatus tendon, and superolateral osteochrondral defects of the humeral head were identified as common throwing lesions. The study also discovered that symptoms correlated poorly with the abnormalities seen on MRI. The study concluded that athlete’s throwing shoulders do tend to have more imaging pathology, however, the correlation with symptoms is poor [44].
Gymnastics: Competitive gymnasts demonstrate a high frequency of shoulder injuries [53]. Unlike other overhead sports, gymnastics related injuries involve bilateral weight bearing [53]. A university-based study that was not included in our study evaluated 21 elite symptomatic and asymptomatic gymnasts along with a control group of 10 age-matched and randomly selected healthy non-athletic population [54]. The study revealed signal abnormalities in 100% of the gymnasts’ shoulders and in 4/20 (20%) of the controls. 16 of 36 (44.4%) had findings consistent with SLAP tears. There were labral lesions in 10 (27.7%) of shoulders compared to none (0%) in the controls. In addition, while none of the controls had partial or full thickness tears of the rotator cuffs, 8/36 (22%) of the gymnasts demonstrated rotator cuff tears. There was no difference between the frequency of shoulder pathology between symptomatic and asymptomatic shoulders, but there was a large, significant difference between gymnasts and healthy controls. The study concluded that gymnasts’ shoulders are significantly different than the general population and tend to have similar rates of shoulder pathology in symptomatic and asymptomatic shoulders [54].
Strength training: Strength training and weightlifting involves placing large forces on the joints of the body. However, the consequences of weight-lifting on the joints has not been well studied. Prior studies have suggested that strength training, particularly weightlifting places an athlete at risk for AC joint pathology in particular [21]. The one study conducted by Noschajew et al. [54] confirmed that hypothesis; out of the eleven asymptomatic bodybuilders evaluated using MRI scans, AC joint hypertrophy (63.6%) and AC joint inflammation (45.5%) had the highest rates of abnormal pathology. Compared to overhead sports, there was a lower frequency of rotator cuff tendinopathy (9.1%) and labral changes (4.5%) overall. The study concluded that strength training is associated with MRI-documented AC joint pathology, even in the absence of symptoms [55].
Ice hockey: Ice Hockey is not an overhead sport, however, given the high frequency of labral tears in professional ice hockey athletes [56] and the high frequency of shoulder pathology on MRI in many other sports, Hacken et al. [56] hypothesized that ice hockey players would have similarly high frequency of shoulder pathology. The results demonstrated that while professional ice hockey players had a 25% frequency of labral pathology, the other locations of shoulder pathology had low rates of diagnosed pathology (<8%), particularly in comparison to other overhead sports such as baseball [57].
Ironman triathletes: Triathletes compete in running, biking, and swimming. Reuter et al. [57] hypothesized that due to the repetitive “arm swimming” associated with running, the stress on the shoulders while holding handle bars in biking, and the repetitive motion of the swimming crawl, Ironman triathletes may demonstrate abnormalities on MRI from activity-related repetitive stress. 7 asymptomatic triathletes and 16 symptomatic triathletes participated in the study conducted by Reuter et al. [57] Results demonstrated that 29% of asymptomatic athletes had rotator cuff tendinopathy compared to 50% of symptomatic athletes, although this finding was not statistically significant [58]. AC joint pathology was found at slightly higher rates in asymptomatic athletes compared to symptomatic athletes (71% to 62%), which was also not a significant finding. The study concluded that there is a high frequency of incidental findings in asymptomatic triathletes that does not necessarily correlate with the presence of symptoms [58].
Wheelchair athletes: Patients who are paraplegic as a result of spinal cord injury are at high risk of shoulder injury due to repetitive motions, over-the-head reaching from a wheelchair position, and overuse [59-60]. Therefore, Akbar et al hypothesized that athletes with paraplegia are at even higher risk for developing pathologic changes in their shoulders when active in sports. The study investigated 103 patients who were participating in overhead sports on a regular basis and 193 subjects that were not involved in sports activity. The study determined that 76% of the overhead sports population had evidence of rotator cuff pathology on MRI compared to 36% of the no sports population [12]. The rotator cuff tears were symptomatic in 93% of the population. The study reported that there was a statistically significant relative risk (RR=2.09, p<0.05) for developing rotator cuff tears in the overhead athlete group compared to the no sports group, with a large amount of the cohort demonstrating shoulder pain. The authors concluded that it is important to develop rehabilitation strategies to encourage physical activity in patients with SCI without increasing the incidence of shoulder pathology in patients with paraplegia that may affect their long-term function [12] (Table 5).
Table 5:Comprehensive table of studies discussed in this article. *not included in quantitative meta-analysis.
Limitations
There are several limitations of this systematic review. First, as described in the conclusion, there were a few studies evaluating asymptomatic shoulder pathology in athletes that were not included in the review because the data reported in the studies did not differentiate reporting asymptomatic shoulder pathology from that of symptomatic shoulder pathology. Several of these studies had a large proportion of asymptomatic shoulders compared to symptomatic shoulders, but since it was unclear how many of the abnormal findings on MRI were discovered in symptomatic versus asymptomatic shoulders, we were unable to extract the data for the primary outcome of frequency of asymptomatic shoulder pathology. In addition, there are unexplained factors that cannot be controlled for, such as the subjectivity of the radiologist read of grading MRI scans for shoulder pathology. Furthermore, in the case where multiple pathologies were noted in one region of the shoulder (for example, the rotator cuff), only the highest number was extracted, which does not account for severity of injury (rotator cuff tendinopathy versus rotator cuff tear). Several shoulder diagnoses are best diagnosed through an alternative imaging modality. This includes labral tears, which are best diagnosed on MRI arthrogram. Finally, the majority of the studies were conducted on high level athletes (college or elite), which suggests a higher frequency of shoulder pathology than the average recreational athletes, so the data we analyzed may not be as generalizable to the general population of athletes.
Conclusion
In this systematic review, pooled summary estimates of the frequency of shoulder pathology on MRI in asymptomatic athletes ranged from 5% to 53%, with significantly higher frequency seen in higher level athletes and overhead sports. This confirms the hypothesis that there is a high frequency of asymptomatic shoulder pathology in athletes, which is likely largely related to wear and tear on the shoulder. Further studies may be required to elucidate the significance of these findings in the context of injury risk and prevention in these athletes.
References
- Shanley E, Kissenberth MJ, Thigpen CA, Bailey LB, Hawkins RJ, et al. (2015) Preseason shoulder range of motion screening as a predictor of injury among youth and adolescent baseball pitchers. J Shoulder Elbow Surg 24(7): 1005-1013.
- Walker H, Gabbe B, Wajswelner H, Blanch P, Bennell K (2012) Shoulder pain in swimmers: A 12-month prospective cohort study of incidence and risk factors. Phys Ther Sport 13(4): 243-249.
- Chase KI, Caine DJ, Goodwin BJ, Whitehead JR, Romanick MA (2013) A prospective study of injury affecting competitive collegiate swimmers. Res Sports Med 21(2): 111-123.
- Tooth C, Gofflot A, Schwartz C, Croisier J, Beaudart C, et al. (2020) Risk factors of overuse shoulder injuries in overhead athletes: A systematic review. Sports Health: A Multidisciplinary Approach 12(5): 478-487.
- Thomas SJ, Swanik CB, Swanik K, Kelly JD (2013) Change in glenohumeral rotation and scapular position after a division i collegiate baseball season. J Sport Rehabil 22(2): 115-121.
- Burn MB, McCulloch PC, Lintner DM, Liberman SR, Harris JD (2016) Prevalence of scapular dyskinesis in overhead and nonoverhead athletes: A systematic review. Orthop J Sports Med 4(2).
- Laudner KG, Lynall R, Meister K (2013) Shoulder adaptations among pitchers and position players over the course of a competitive baseball season. Clin J Sport Med 23(3): 184-189.
- Hibberd EE, Laudner KG, Kucera KL, Berkoff DJ, Yu B, et al. (2016) Effect of swim training on the physical characteristics of competitive adolescent swimmers. Am J Sports Med 44(11): 2813-2819.
- Doyscher R, Kraus K, Finke B, Scheibel M (2014) Acute injuries and overuse injuries to the shoulder in sports. Orthopade 43(3): 202-208.
- Burkhart SS, Morgan CD, Kibler WB (2003) The disabled throwing shoulder: Spectrum of pathology Part II: Evaluation and treatment of SLAP lesions in throwers. Arthroscopy: The Journal of Arthroscopic & Related Surgery 19(5): 531-539.
- Burkhart SS, Morgan CD, Kibler WB (2003) The disabled throwing shoulder: Spectrum of pathology part I: Pathoanatomy and biomechanics. Arthroscopy 19(4): 404-420.
- Akbar M, Brunner M, Ewerbeck V, Wiedenhöfer B, Grieser T, et al. (2015) Do overhead sports increase risk for rotator cuff tears in wheelchair users? Arch Phys Med Rehabil 96(3): 484-488.
- Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB (1995) Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am 77(1): 10-15.
- Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, et al. (2004) Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am 86(4): 708-716.
- Gill TK, Shanahan EM, Allison D, Alcorn D, Hill CL (2014) Frequency of abnormalities on shoulder MRI in symptomatic and asymptomatic older adults. Int J Rheum Dis 17(8): 863-871.
- Chandnani V, Ho C, Gerharter J, Neumann C, Kursunoglu-Brahme S, et al. (1992) MR findings in asymptomatic shoulders: A blind analysis using symptomatic shoulders as controls. Clin Imaging 16(1): 25-30.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et al. (2021) The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372: n71.
- Culvenor AG, Øiestad BE, Hart HF, Stefanik JJ, Guermazi A, et al. (2019) Frequency of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: A systematic review and meta-analysis. Br J Sports Med 53(20): 1268-1278.
- Downs SH, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52(6): 377-384.
- Higgins JPT (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414): 557-560.
- Cahill BR (1992) Atraumatic osteolysis of the distal clavicle. Sports Medicine 13(3): 214-222.
- Noschajew E, Azesberger A, Rittenschober F, Windischbauer A, Gruber MS, et al. (2022) The effect of strength training on undetected shoulder pathology in asymptomatic athletes: An MRI observational study. Sports 10(12): 210.
- Miniaci A, Mascia AT, Salonen DC, Becker EJ (2002) Magnetic resonance imaging of the shoulder in asymptomatic professional baseball pitchers. Am J Sports Med 30(1): 66-73.
- Halbrecht JL, Tirman P, Atkin D (1999) Internal impingement of the shoulder: Comparison of findings between the throwing and nonthrowing shoulders of college baseball players. Arthroscopy: The Journal of Arthroscopic & Related Surgery 15(3): 253-258.
- Pennock AT, Dwek J, Levy E, Stearns P, Manning J, et al. (2018) Shoulder MRI abnormalities in asymptomatic little league baseball players. Orthop J Sports Med 6(2):
- Takahashi M, Iwamoto K, Monma M, Mutsuzaki H, Mizukami M (2021) The area of impingement in the throwing versus nonthrowing shoulder of collegiate baseball players: An MRI study of the simulated late-cocking phase of throwing. Orthop J Sports Med 9(3):
- Su BY, Yeh WC, Lee YC, Chen JH, Yeh LR (2020) Internal derangement of the shoulder joint in asymptomatic professional baseball players. Acad Radiol 27(4): 582-590.
- Johansson FR, Skillgate E, Adolfsson A, Jenner G, DeBri E, et al. (2015) Asymptomatic elite adolescent tennis players’ signs of tendinosis in their dominant shoulder compared with their nondominant shoulder. J Athl Train 50(12): 1299-1305.
- Bigliani LU, Codd TP, Connor PM, Levine WN, Littlefield MA, et al. (1997) Shoulder motion and laxity in the professional baseball player. Am J Sports Med 25(5): 609-613.
- Kvitne RS, Jobe FW (1993) The diagnosis and treatment of anterior instability in the throwing athlete. Clin Orthop Relat Res (291): 107-123.
- Connor PM, Banks DM, Tyson AB, Coumas JS, D’Alessandro DF (2003) Magnetic resonance imaging of the asymptomatic shoulder of overhead athletes. Am J Sports Med 31(5): 724-727.
- Bak K (2010) The practical management of swimmer’s painful shoulder: Etiology, diagnosis, and treatment. Clinical Journal of Sport Medicine 20(5): 386-390.
- Fredericson M, Ho C, Waite B, Jennings F, Peterson J, et al. (2009) Magnetic resonance imaging abnormalities in the shoulder and wrist joints of asymptomatic elite athletes. PM & R 1(2): 107-116.
- Heinlein SA, Cosgarea AJ (2010) Biomechanical considerations in the competitive swimmer’s shoulder. sports health: A multidisciplinary approach. Sports Health 2(6): 519-525.
- Sein ML, Walton J, Linklater J, Appleyard R, Kirkbride B, et al. (2010) Shoulder pain in elite swimmers: Primarily due to swim-volume-induced supraspinatus tendinopathy. Br J Sports Med 44(2): 105-113.
- Celliers A, Gebremariam F, Joubert G, Mweli T, Sayanvala H, et al. (2017) Clinically relevant Magnetic Resonance Imaging (MRI) findings in elite swimmers’ shoulders. South African Journal of Radiology 21(1):
- Holt K, Delbridge A, Josey L, Dhupelia S, Livingston GC, et al. (2022) Subscapularis tendinopathy is highly prevalent in elite swimmer’s shoulders: An MRI study. J Sci Med Sport 25(9): 720-725.
- Escamilla RF, Andrews JR (2009) Shoulder muscle recruitment patterns and related biomechanics during upper extremity sports. Sports Medicine 39(7): 569-590.
- Lee CS, Goldhaber NH, Davis SM, Dilley ML, Brock A, et al. (2020) Shoulder MRI in asymptomatic elite volleyball athletes shows extensive pathology. Journal of ISAKOS 5(1): 10-14.
- Beitzel K, Beitzel KI, Zandt JF, Buchmann S, Schwirtz A, et al. (2013) Premature cystic lesions in shoulders of elite junior javelin and volleyball athletes: A comparative evaluation using 3.0 Tesla MRI. J Shoulder Elbow Surg 22(6): 792-799.
- Lajtai G, Pfirrmann CWA, Aitzetmüller G, Pirkl C, Gerber C, et al. (2009) The shoulders of professional beach volleyball players: high frequency of infraspinatus muscle atrophy. Am J Sports Med 37(7): 1375-1383.
- Jerosch J, Castro WHM, Drescher H, Assheuer J (1993) Magnetic resonance morphological changes in the shoulder joints of world-class water polo players. Sportverletzung Sportschaden 7(03): 109-114.
- Klein M, Tarantino I, Warschkow R, Berger CJ, Zdravkovic V, et al. (2014) Specific shoulder pathoanatomy in semiprofessional water polo players. Orthop J Sports Med 2(5).
- Jost B, Zumstein M, Pfirrmann CWA, Zanetti M, Gerber C (2005) MRI findings in throwing shoulders. Clin Orthop Relat Res (434): 130-137.
- McMaster WC, Roberts A, Stoddard T (1998) A correlation between shoulder laxity and interfering pain in competitive swimmers. Am J Sports Med 26(1): 83-86.
- Schmitt H, Hansmann HJ, Brocai DR, Loew M (2001) Long term changes of the throwing arm of former elite javelin throwers. Int J Sports Med 22(4): 275-279.
- Kunz H, Kaufmann DA (1983) Cinematographical analysis of javelin throwing techniques of decathletes. Br J Sports Med 17(3): 200-204.
- Cooper JD, Seiter MN, Ruzbarsky JJ, Poulton R, Dornan GJ, et al. (2022) Shoulder Pathology on magnetic resonance imaging in asymptomatic elite-level rock climbers. Orthop J Sports Med 10(2).
- Cooper JD, Seiter MN, Ruzbarsky JJ, Poulton R, Dornan GJ, et al. (2022) Shoulder pathology on magnetic resonance imaging in asymptomatic elite-level rock climbers. Orthop J Sports Med 10(2):
- Hagemann G, Rijke AM, Mars M (2004) Shoulder pathoanatomy in marathon kayakers. Br J Sports Med 38(4): 413-417.
- Kizer KW (1987) Medical aspects of white-water kayaking. Phys Sportsmed 15(7): 128-137.
- Gerhardt C, Doyscher R, Boschert HP, Scheibel M (2014) The gymnast shoulder. The Orthopedics 43(3): 230-235.
- Carli A, Mossa L, Larciprete M, Ferretti M, Argento G, et al. (2012) The gymnast’s shoulder MRI and clinical findings. J Sports Med Phys Fitness 52(1): 71-79.
- Noschajew E, Azesberger A, Rittenschober F, Windischbauer A, Gruber MS, et al. (2022) The Effect of strength training on undetected shoulder pathology in asymptomatic athletes: An MRI observational study. Sports 10(12): 210.
- Silvis ML, Mosher TJ, Smetana BS, Chinchilli VM, Flemming DJ, et al. (2011) High frequency of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players. Am J Sports Med 39(4): 715-721.
- Hacken B, Onks C, Flemming D, Mosher T, Silvis M, et al. (2019) Frequency of MRI shoulder abnormalities in asymptomatic professional and collegiate ice hockey athletes. Orthop J Sports Med 7(10):
- Reuter RM, Hiller WD, Ainge GR, Brown DW, Dierenfield L, et al. (2008) Ironman triathletes: MRI assessment of the shoulder. Skeletal Radiol 37(8): 737-741.
- Subbarao JV, Klopfstein J, Turpin R (1995) Prevalence and impact of wrist and shoulder pain in patients with spinal cord injury. J Spinal Cord Med 18(1): 9-13.
- Kulig K, Rao SS, Mulroy SJ, Newsam CJ, Gronley JK, et al. (1998) Shoulder joint kinetics during the push phase of wheelchair propulsion. Clin Orthop Relat Res (354): 132-143.
- Akbar M, Balean G, Brunner M, Seyler TM, Bruckner T, et al. (2010) Prevalence of rotator cuff tear in paraplegic patients compared with controls. The Journal of Bone and Joint Surgery-American 92(1): 23-30.
© 2023 Connie Hsu. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






