- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
Inpatient-Rehabilitation in Times of the SARS-CoV2 Pandemic - Fears and Differences in Different Disease Patterns
Jonas Antek Koller1, Matthias Dreher1, Magdalena Tueg2, Juergen Koerber3, Ute Dederichs-Masius4, Thomas Wilde5 and Andreas Schwarting1,2*
1Department of Internal Medicine I, Division of Rheumatology and Clinical Immunology, University Medical Center of the Johannes Gutenberg University Mainz, Germany
2Rheumatology Center Rhineland Palatinate, Germany
3Oncological Rehabilitation, Hamm Clinic Nahetal, Germany
4Cardiology, Drei-Burgen-Clinic, Germany
5Psychosomatic Clinic, St. Franziska-Stift, Germany
*Corresponding author:Andreas Schwarting, Focus on Rheumatology and Clinical Immunology, University Medicine Mainz, Langenbeckstraße 1, 55131 Mainz, Germany
Submission: July 24, 2023; Published: August 25, 2023

ISSN 2637-7934 Volume4 Issue3
Abstract
Objective: Analysing rehabilitation- and mental health related information and sociodemographic features of patients in inpatient rehabilitation during the COVID-19 pandemic to identify factors influencing the fear of SARS-CoV-2. Patients admitted to inpatient rheumatological, orthopaedic, cardiological, oncological or psychosomatic rehabilitation settings. Materials and methods: Cross-sectional questionnaire study of patients in five different rehabilitation settings in Rhineland-Palatinate, Germany between May and August 2021 during the third SARSCoV- 2 wave. The survey included 653 patients and used a self-reported paper & pencil questionnaire. The collected data was described for each rehabilitation facility and subjected to analyses of variance, correlation and linear regression to investigate associations between the score of the Fear of the Coronavirus Questionnaire (FCQ) and additional data were performed. Result: Differences of fear concerning the coronavirus between the rehabilitation subgroups were found (η=0.172, p<0.05), with highest fear scores in orthopaedic participants (MFCQ=28.65, SD=5.79). The fear examined correlated positively with age (r=0.223, p<0.001). Negative correlations exist with the absence of depressive symptoms (rWHO-5=-0.122, p<0.05), less pain (rIRES-24 Dimension Pain=-0.19, p<0.001), better rated personal somatic and mental health (rself assessed somatic health=-0.187, p<0.001; rself assessed mental health=-0.108, p<0.05) and with everyday functionality (rIRES-24 Dimension Functionality=-0.329, p<0.001). Conclusion: The study identified predictors for virus-related fear. Using those can help to recognize vulnerable groups in times of a pandemic and improve rehabilitation processes.
Keywords:Anxiety; Coronavirus; COVID-19; SARS-CoV-2; Depression; Fear; Rehabilitation; Wellbeing; Physical activity
Introduction
The expiring COVID-19 pandemic put the somatic and mental health of the population to the test. Besides the virus-associated hazards for health, people reported to have suffered from psychological distress. Exemplary factors of psychological distress were social isolation, financial and professional uncertainty or worries about oneself or people close getting infected [1-3]. People with pre-existing somatic or mental conditions as well as the general population stated a decrease in well-being [4]. The phenomenon of fear as an important factor of the population’s mental health in the context of spreading infectious diseases is recognized and received enhanced attention during the current pandemic. Fear itself is a universal human emotion with a cognitive, behavioural and biological dimension [5,6]. If fear is adapted adequately to the potential or actual threat, its physically and mentally arousing character is protective although unpleasant. Fear experienced inappropriately in intensity, frequency or duration therefore causes a decrease in well-being can become pathological [7]. Knowing that people with pre-existing medical conditions are more likely to suffer severe outcomes of a SARS-CoV-2-infection can be an additional stressor for affected persons [8]. Self-evidently rehabilitants already reported worries about physical symptoms, a decrease in mental well-being or social support before the pandemic [9]. Mental and physical health is a predictor for successful rehabilitation outcomes, and both were at risk during the pandemic [10].
Rehabilitants as patients with mostly chronic diseases are therefore assumingly additionally burdened with psychological distress and fear. Depending on age, marital status and the clinical picture, the anxiety seems to be pronounced differently. For example, psychosomatic patients seem to have a high level of anxiety [11]. This survey was conducted to investigate these circumstances by finding predictors for virus-related fear in inpatient rehabilitants during the pandemic. Statistical analyses were performed to analyse associations of fear of the coronavirus, measured by the Fear of the Coronavirus Questionnaire (FCQ), with obtained sociodemographic, health and rehabilitation related data [12]. The results of the investigation shall help to prevent and treat people suffering from psychological distress during a crisis like the COVID-19 pandemic by identifying vulnerable groups and improve therapeutic approaches. Addressing fears by e.g., therapeutic education is known to decrease anxiety and fear-avoidance belief, especially beneficial in orthopaedic rehabilitation and improve patient’s functionality [13]. The inevitability of future epidemics and the probability of them occurring in shorter intervals will require appropriate measures in health services to support the psychological burdened [14].
Material and Methods
Between May and August 2021 (during the third SARSCoV- 2 period in Germany) the survey was conducted in inpatient rehabilitation centers in Rhineland-Palatinate with five different specialties. These are cardiological, psychosomatic, orthopaedic, rheumatological, oncological rehabilitation. A self-reported questionnaire was distributed to every patient according to general rehabilitation information during check in. The patients were informed about their anonymity and voluntary participation. To increase the level of anonymity of the survey, the collection of personal data was reduced to a minimum. The patients were pleased to return the questionnaires in a locked box. After the survey phase, the questionnaires were read in by the Center for Quality Assurance and Development (ZQ) of the Hochschulevaluierungsverbund Suedwest e.V. at the Johannes Gutenberg University in Mainz and transmitted to the authors.
The focus of the study is addressing emotional well-being in the face of the COVID-19 pandemic. Beside sociodemographic parameters, data of mental and somatic health and rehabilitationrelated information about the subjects were obtained. In addition, the WHO-5 Questionnaire for general well-being, the Center for Epidemiologic Studies Depression Scale (CES-D), the Work Ability Index Questionnaire, which assesses subjective work ability, the Indicators of Rehabilitation Status Questionnaire, which evaluates physical activity, the International Physical Activity Questionnaire (IPAQ), and the Fear of the Coronavirus Questionnaire (FCQ) were inquired [12,15-19]. The FCQ was developed by Mertens et al. to operationalize and quantify virus-related fear and consists of eight items, each of them corresponding to known predictors of fear, like psychological vulnerability, personal relevance, and media consumption concerning the pandemic [12]. The questionnaire uses a five-point likert scale to measure the degree of agreement with each statement, from “strongly disagree” (equals one point) to “strongly agree” (equals five points (pts)). From all items the scores are added to a total score. A higher total score indicates more coronavirus related fear. Items are for example: “I am taking precautions to prevent infection” or “I am constantly following all news updates regarding the virus” [12]. A German Version of the FCQ was developed and approved during the study based on three times translation and re-translation by medical experts. The used 24-item short form of the IRES-24 consists of four dimensions and generates scores for each dimension separately. It categorizes the sum of pts collected in one dimension into classes of burden (“unremarkable”, “remarkable” and “grave”) [17]. Higher scores are associated with less burden. The CES-D asks the interviewee in 20 items about the frequency of depressive symptoms in the last week. Higher scores are associated with a higher probability of being clinically depressive [15]. The shown parameter “Total Metabolic Equivalent of Task-minutes per week” (MET-min/week) is calculated from information delivered by the IPAQ and expresses the activity level of the last month [18].
The main aim of this survey was to identify factors influencing the fear of coronavirus-measured by the FCQ. For this purpose, the sample was separately described by rehabilitation institution/ indication. The mean values, of the scores achieved in the FCQ were compared between the rehabilitation indications by means of single factor analyses of variance. Subsequently, correlation analyses were performed to investigate associations of the FCQ score with surveyed parameters of interest. Depending on the scaling of the data, this was realized by means of calculating the Pearson, Spearman, Kendall-Tau, and Eta correlation coefficients. The calculated correlations were tested for significance. For a detailed description the significant correlations determined, the corresponding data were subjected to regression analyses. The resulting p-values were considered nominally significant at p<0.05. Statistical analyses were calculated with SPSS PASW27 Statistics (IBM Corp., Somers, NY).
Result and Discussion
Data of 653 individuals in inpatient rehabilitation was collected in the five-month long collection period of this survey. 1000 questionnaires were handed out to patients; therefore, the response rate was 65.3%. Due to participants not answering every item of the questionnaire, missing data were noted, concerning the evaluable results. Sociodemographic features and self-reported information about health issues divided by subgroup of rehabilitation are summarized in Table 1. As shown, most of the surveyed patients were situated in orthopaedic rehabilitation (n=140, 21.4%), while the minority participated was situated in cardiologic rehabilitation (n=83, 12.7%). Overall, more women participated in this study (n=375, 57.4%). Participants of the study indicated their age by assigning themselves to one of 18 groups. Except for the group of 18 to 19-year-olds, each group represented a five-year span from 20 to 104 years. The median (Q2) of age in the whole sample was 55 to 59 years (Q2: n=174, 26.6%) with an interquartile range from 50 to 54 years (Q1: n=114, 17.5%) to 60 to 64 years (Q3: n=141, 21.6%). The quartiles of the psychosomatic rehabilitants (Q2=50-54 years, nQ2=17, 13.2%; Q1=40-44 years, nQ1=7, 5.4%; Q3=55-59 years, nQ3=26, 20.2%) showed lower values indicating a lower age on average. As presented in Table 1 the rehabilitation subgroups also differed in the percentage of smokers, the average BMI respectively the share of people with overweight relationship status and professional qualification. Due to its purpose of operationalizing COVID-19-related fear, the FCQ functioned as the central instrument of this examination. The analysis of reliability showed a good internal consistency of the generated German version of The FCQ (Cronbach’s alpha=0.80).
Table 1:Descriptive statistics of the study population: Sociodemographic features and self-reported information about health issues of the participants, n=589.
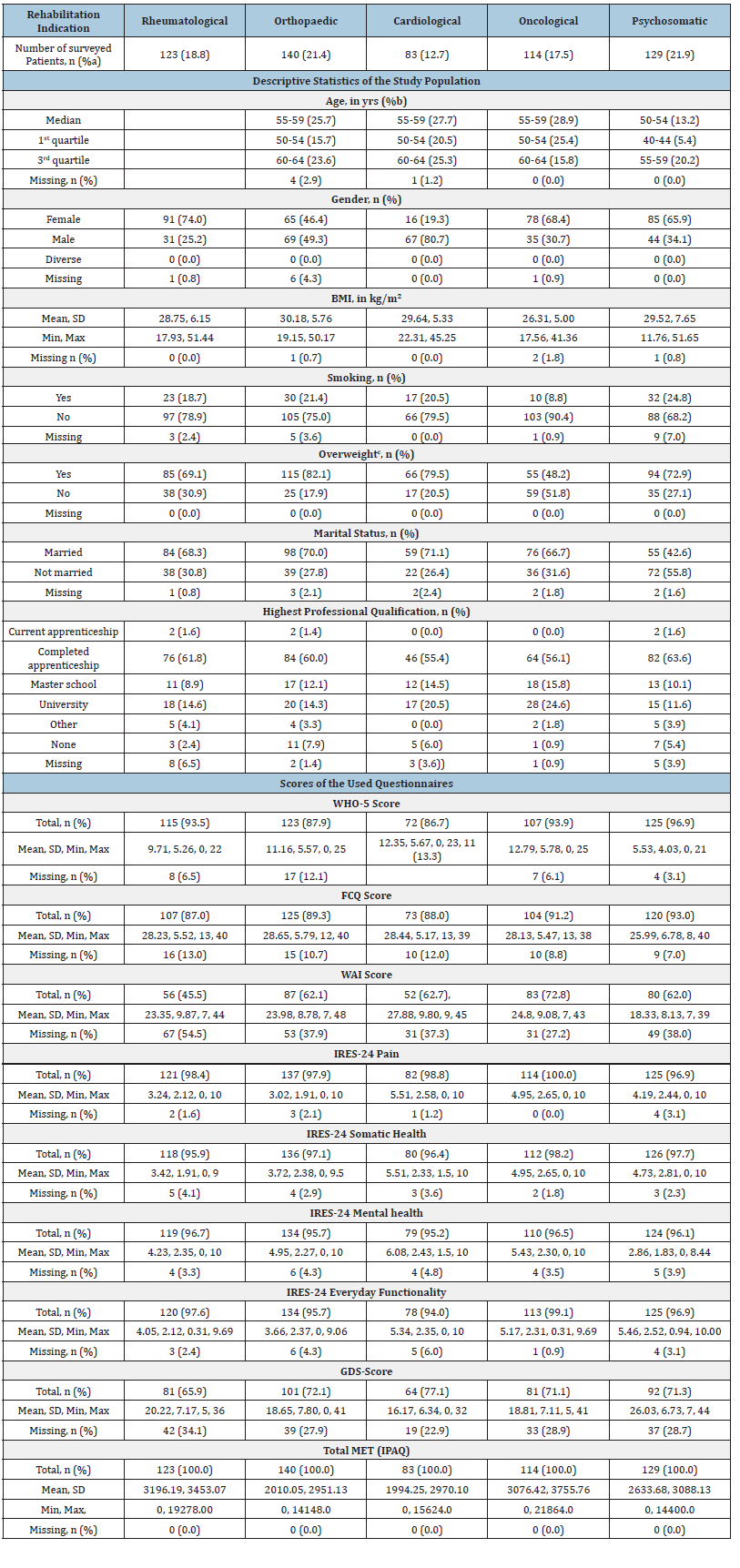
BMI: Body Mass Index; SD: Standard Deviation, Min: Minimum, max: Maximum aRefers to the percentage of the of all participants in this study reporting the rehabilitation facility bRefers to the percentage of participants belonging to the particular age group of all participants included in the rehabilitation subgroup cOverweight defined by the World Health Organization as having a BMI≥25 kg/m² *More than one modus. The smallest value is shown.
The FCQ showed a mean value of the total score across the rehabilitation subgroups of 27.69 pts (n=581, 89%; SD=5.95pts). The highest mean value of the FCQ score was reached by orthopaedic patients (n=125, 89.3%; M=28.65pts; SD=5.79pts) opposed by the psychosomatic patients with the lowest mean values of the FCQ score (n=120, 93%; M=25.99pts; SD=6.78). The mean values of other groups remained in between, all reaching values over 28 pts (with SDs between 5.17 and 5.52 pts). The poorest wellbeing referring to the mean value of the WHO-5 was clearly to be found in the psychosomatic subgroup (n=125, 96.9%; M=5.53pts; SD=4.03pts). Corresponding to the poor assessment of their wellbeing, psychosomatic patients also reported the lowest work ability (n=80, 62%; M=18.33pts; SD=8.13pts), measured by the mean value of the WAI score. The average WAI score of all participants was 23.55 pts (n=385, 69.6%; SD=9.36pts).
The first dimension of the IRES-24 addresses the lately experienced pain and revealed the group of cardiologic rehabilitants as the group with lesser burden referring to pain (n=82, 98.8%; M=5.51pts; SD=2.55pts). Orthopaedic rehabilitants became apparent as the subgroup with the most pain associated burden (n=137, 97.9%; M=3.02pts; SD=1.91pts) referring to the IRES-24. Taken together the surveyed patients reported an average score for pain of 4.13 pts (n=640; SD=2.49pts). Dimension 2 of the IRES-24 evaluated the somatic health of the interviewees. It showed that in the surveyed population the group of rheumatologic patients with its lowest mean value of the scores (n=118; M=3.42pts; SD=1.91pts) were more burdened with pain than the other subgroups. Over all subgroups the average score was 4.32pts (n=632, 96.8%; SD=2.52pts). The score of dimensions 3 of the IRES-24 is associated with the mental condition. The cardiologic rehabilitants showed the highest mean value of the scores (n=79; 95.2%; M=6.08pts; SD=2.43pts), while the psychosomatic subgroup expressed the lowest mental health (n=124, 96.1%; M=2.86pts; SD=1.83pts) according to the IRES-24. The average score of all participants was 4.6pts (n=628, 96.2%; SD=2.45pts). The fourth dimension of the IRES-24 addresses the functionality regarding the execution of everyday tasks. The psychosomatic subgroup reported the best everyday functionality (n=125, 96.9%; M=5.46pts; SD=2.52pts). Least functioning according to the IRES-24 were participants in orthopaedic rehabilitation (n=134, 95.7%; M=3.66pts; SD=2.37pts). For the study population, a mean value of 4.66 pts was observed (n=629, 96.3%; SD=2.43pts).
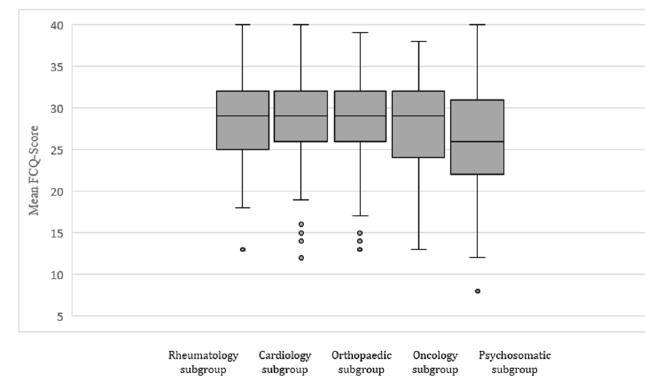
Results of the CES-D showed a mean value of 20.08 pts in the scores of all participants (n=450, 68.9%; SD=7.64pts). With a mean value of 26.03pts the psychosomatic rehabilitants (n=92, 71.3%; SD=6.73pts) achieved the highest mean score. The cardiologic subgroup reported least depressive symptoms as shown by a mean value of 16.17 pts (n=64, 77.1%; SD=6.34pts). Concerning the activity level of participants, in the undivided population an average of 2610.6 MET was measured (n=653; SD=3276.08). The most active subgroup according to their total MET week was the rheumatologic collective (n=123; 100%; M=3196.19; SD=3453.07). The lowest average total MET was reported by the cardiologic rehabilitants (n=83, 100%; M=1994.25; SD=2970.10). The conducted one-way Analysis of Variance (ANOVA) showed a statistically significant difference in levels of pandemic-related fear (measured by the FCQ) for the different rehabilitation subgroups, F (4, 524)=3.99, p<0.05. The boxplots displaying the measures of location of the mean FCQ scores of each rehabilitation subgroup are shown in Figure 1.
Figure 1:Analysis of variance displayed as boxplot of mean FCQ scores of each rehabilitation subgroup. F(4, 524)=3.99, p<0.05. Rheumatology subgroup: n=107, M=28.23, SD=5.52. Cardiology subgroup: n=73, M=28.44, SD=5.17. Orthopaedic subgroup: n=125, M=28.65, SD=5.79. Oncology subgroup: n=104, M=28.13, SD=5.47. Psychosomatic subgroup: n=120, M=25.99, SD=6.78.
The linear relationship between the FCQ score and other obtained variables was, depending on the scaling, assessed by correlation analyses, using the Pearson- and Spearman-coefficients (Table 2) as well as the Eta coefficient (Table 3). Positive correlations could be shown between the FCQ score and the CES-D score (n=569, r=0.329, p<0.05) as well as for the age of surveyed participants (n=575; ρ=0.223, p<0.001; τb=0.167, p<0.01). Statistically significant negative correlations between the FCQ score and the WHO-5 score (n=542, r=-0.122, p<0.05), the IRES-24 dimension of pain (n=575, r=-0.190, p<0.001), somatic health (n=571, r=-0.242, p<0.01), mental condition (n=568, r=-0.119, p <0.001) and everyday functionality (n=571, r=-0.329, p<0.001), the self-assessment of health (n=574; ρ=-0.187, p<0.001; τb=-0.136, p<0.05), the selfassessment of mental health (n=568; ρ=-0.108, p<0.05; τb=-.078, p<0.05) as well as for the level of activity expressed by the total MET minutes per week (n=581, r=-0.092, p<0.05) were found. The linear relationship towards the BMI (n=578, r=0.041, p=0.32) was not statistically significant.
Table 2:Pearson and spearman correlation analyses between the FCQ-Score and metrically scaled collected data of interest.
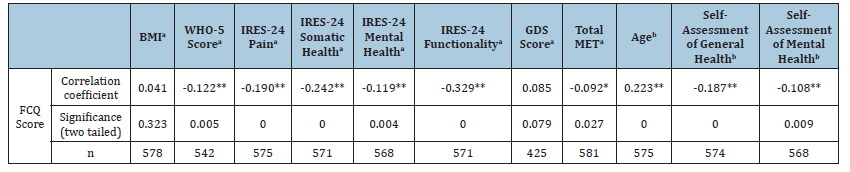
**Correlation is significant at the 0.01 level (two tailed). *Correlation is significant at the 0.05 level (two tailed). aPearson correlation. bSpearman correlation.
Table 3:Eta correlation analysis between the FCQ Score and nominally scaled collected data of interest.
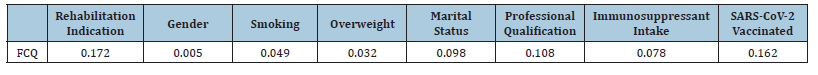
Following Cohen’s classification most of the correlations shown above are to be called rather weak. Cohen stated Pearson and Spearman coefficients equaling 0.1 are associated with a weak association, those equaling 0.3 with a moderate and those equaling 0.5 with a strong correlation [20]. Non-linear associations between nominally scaled variables of interest and the FCQ score were examined using the eta coefficient (η). The results of the eta correlation are summarized in Table 3. To investigate the significance of the results a univariate analysis of variance was carried out subsequently. The computation revealed a statistically significant positive correlation between the FCQ score and four of the eight examined variables. Those were the rehabilitation indication (n=529, η=0.172, p<0.05), the smoking status (n=563, η=0.049, p<0.05), receiving at least one SARS-CoV-2 vaccination (n=568, η=0.162, p<0.05) and the marital status (n=570, η=0.098, p<0.05). The other variables consisting of gender, overweight, immunosuppressant intake and professional qualification were not significantly associated to the FCQ score. The regression analysis of the FCQ score using the rehabilitation indications as independent variables (Table 4) indicated the orthopaedic subgroup (ß=0.185 (95% CI 1.27 to 4.08), p<0.05) to have the highest FCQ scores referring to the psychosomatic subgroup. In reference to the unvaccinated participants the regression analysis using the vaccination status as independent variable, showed that unvaccinated participants reported more fears concerning the new coronavirus (ß=0.154 (95% CI 1.00 to 3.21), p<0.05). Smoking and marital status had no significant impact on the examined variance.
On basis of the regression analysis with age as independent variable it can be stated that older participants declared to have more fears in comparison to younger participants (ß=0.224 (95% CI 0.417 to 0.881), p<0.05). Referring to the regression analysis between the FCQ score and the subjective assessment of the personal health the values in subjective personal health are opposingly associated with the score of fear of SARS-CoV-2 (ß=- 0.194 (95% CI -0.72 to -0.30), p<0.05). The subjective assessment of the personal mental health also impacted the FCQ score in an opposing way (ß=-0.110 (95% CI -0.41 to -0.059), p<0.01). The regression analysis using the WHO-5 score as predictor indicated that an estimated lower well-being of patients increases fears of the new coronavirus (ß=-0.110 (95% CI -0.41 to -0.059), p<0.01). The same effect applied to the WAI score. Lower scores in the WAI questionnaire increased the FCQ score, therefore a lower work ability is associated with a higher fear of the SARS-CoV-2 (ß=-0.110 (95% CI -0.41 to -0.059), p<0.05). The regression analyses of all dimensions of the IRES-24 showed negative associations between the scores of each dimension and the FCQ score. Note that the height of the IRES-24 scores is affiliated with a decreasing burden. Accordingly higher values in the dimension pain are interpreted as less burdensome and were associated with lower FCQ scores (ß=-0.451 (95% CI -0.64 to -0.26), p<0.05). Poorer somatic health, measured by dimension 2 of the IRES-24, was connected to more fear (ß=-0.242 (95% CI -0.767 to -0.386), p<0.05). Similar effects were found for the dimensions of mental health (ß=-0.288 (95% CI -0.49 to -0.10), p<0.05) and everyday functionality (ß=-0.329 (95% CI -0.987 to -0.609), p<0.05). As the regression analysis between the FCQ score and the total MET minutes per week show, the activity level, operationalized through the IPAQ and measured in MET minutes per week, had no impact on the FCQ score (ß=0.000 (95% CI 0.00 to 0.00), p<0.05).
To explain the variance of the FCQ score a linear regression analysis of the corresponding data was performed (Table 4). Due to some variables being nominally scaled, this was partially done by using dummy variables and reference categories. The results showed the FCQ score’s variance is rather marginally explained by the factors surveyed. The variables and proportions of the explained variance were the everyday functionality according to IRES-24 contributing 10.8%, the WAI score contributing 6.3%, somatic health according to IRES-24 contributing 5.9%, age contributing 5%, the self-assessment of health contributing 3.8%, pain according to IRES-24 contributing 3.6%, the rehabilitation indication contributing 3%, the SARS-CoV-2 vaccination status contributing 2.4%, the WHO-5 score contributing 1.5%, mental health according to IRES-24 contributing 1.4% and the selfassessment of mental health contributing 1.2%. MET minutes per week and could explain less than 1% of the FCQ score’s variance.
Table 4:Linear regression analysis between the dependent variable “FCQ Score” and obtained data.
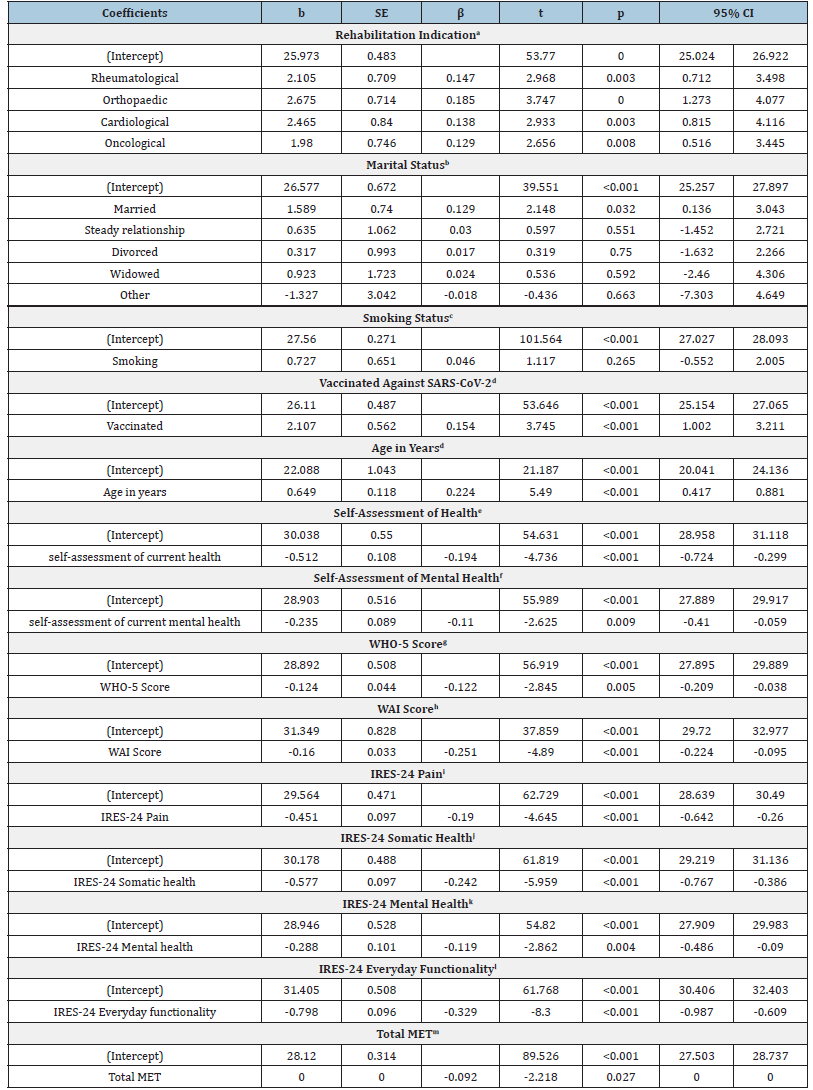
aNote. N=581; R²=0.030; adjusted R²=0.023; F(4, 576)=4.479: p=0.00143; regression analysis using dummy variables with reference category “psychosomatic rehabilitation” bNote. N=581; R²=0.013; adjusted R²=0.004; F(5, 575)=1.465; p=0.19957; regression analysis using dummy variables with reference category “single” cNote. N=581; R²=0.002; adjusted R²=0; F(1, 579)=1.247; p=0.26464; regression analysis using dummy variables with reference category “non-smoking” dNote. N=581; R²=0.024; adjusted R²=0.022; F(1, 579)=14.026; p<0.001; regression analysis using dummy variables with reference category “not vaccinated against SARS-CoV-2” dNote. N=575; R²=0.05; adjusted. R²=0.048; F(1, 573)=30.138; p<0.001 eNote. N=574; R²=0.038; adjusted R²=0.036; F(1, 572)=22.432; p<0.001 fNote. N=568; R²=0.012; adjusted R²=0.01; F(1, 566)=6.889; p=0.00891 gNote. N=542; R²=0.015; adjusted R²=0.013; F(1, 540)=8.093; p=0.00461 hNote. N=359; R²=0.063; adjusted R²=0.06; F(1, 357)=23.916; p<0.001 iNote. N=575; R²=0.036; adjusted R²=0.035; F(1, 573)=21.575; p<0.001 jNote. N=571; R²=0.059; adjusted R²=0.057; F(1, 569)=35.506; p<0.001 kNote. N=568; R²=0.014; adjusted R²=0.013; F(1, 566)=8.192; p=0.00436 lNote. N=571; R²=0.108; adjusted R²=0.106; F(1, 569)=68.885; p<0.001 mNote. N=581; R²=0.008; adjusted R²=0.007; F(1, 579)=4.921; p=0.02692.
Discussion
The results of this study affirmed the hypothesis that pandemic-related fears are associated with somatic and mental health. Participants reporting more impairments in the surveyed dimensions overall stated to be more fearsome concerning the COVID-19 pandemic. The mean FCQ score over all subgroups of rehabilitants was higher than the mean score of a sample of the general public examined in original study of Mertens et al. [12] (27.69 vs. 25.85pts) [12]. As the analysis of internal consistency of the translated FCQ (Cronbach’s alpha=0.80) showed, the computed value of Cronbach’s alpha was good, and therefore slightly higher than the Cronbach’s alpha of the original english questionnaire (Cronbach’s alpha=0.77) [12]. The study population examined by us, was older (Mertens et al. [12]: 47.9% of the participants were between 21 and 30 years old), included a larger percentage of male participants (Mertens et al. [12]: 69.9% of the participants were female) and consisted of lesser people with a university degree (Mertens et al. [12]: 63.1% of the participants had a master’s degree) [12]. Patients in inpatient rehabilitation can be assumed to have pre-existing health conditions and the results thereby contribute to the assumption that people with pre-existing health issues are at greater risk for a decrease in mental health in times of a pandemic [21].
According to literature, psychosomatic patients are more likely to suffer from increasing anxiety and depressive symptoms compared to the general population during COVID-19 [11]. This circumstance let us to expect, that psychosomatic rehabilitants are especially fearsome concerning the pandemic amongst the rehabilitation subgroups. Contrary to our expectations, the psychosomatic subgroup reported the least virus-related fear. Taking the multifactoriality of fear in account, the fact, that psychosomatic rehabilitants declared the lowest fear score may be relatively explainable by the younger age of this subgroup. Further research and statistic procedures are necessary to clarify this circumstance. In order to reduce fear of pandemics, rehabilitation services may require early diagnosis of neuropsychiatric conditions of patients to provide adequate nutritional interventions to stabilize these mental disorders [22]. It should be mentioned, that even though the measured difference in pandemic-related fear between the subgroups according to the FCQ score was significant, the relevance for practical aspects could be considered as marginal, due to the small range of the mean FCQ scores across the groups (25.99 pts to 28.65pts). We revealed increasing age to be a predictor of virusrelated- fears, although in other studies older age was associated with less fear of an infection [23,24]. Other sociodemographic data associated with the FCQ value was the marital status, identifying married people as the most fearsome followed by singles. Other studies also found the marital status to be a significant predictor, while amongst stated that singles seem to be more fearsome [25]..
In the surveyed population smokers communicated more virusrelated fears than non-smokers. This could be explained by the perception of the risks for health in persons affected, due to them recognizing the new coronavirus heightens the risk of a severe outcome in case of a SARS-CoV-2 infection [26]. Being vaccinated against SARS-CoV-2 at least once was associated with less fears concerning the pandemic, according to our results. This might be the result of people being vaccinated feeling safer and therefore less fearsome concerning a SARS-CoV-2 infection. As was shown by Mertens et al. [27] fears measured by the FCQ value counts as factors predicting the willingness of people to get vaccinated [27]. Our analyses showed no significant influence and the BMI/ being overweight, gender, intake of immunosuppressants and the highest professional qualification on coronavirus related fears of participants. Obtained health-related information also included the introduced questionnaires. The analyses of the overall wellbeing expressed through the WHO-5, the work ability measured by WAI and pain, mental and somatic health as well as everyday functionality examined by the different dimensions of the IRES-24 revealed that the more impairments are reported the more virusrelated- fears are declared. For the general public the significant global decrease in mental well-being in times of the pandemic, as measured by the WHO-5, has been described by Wilke et al. [28]. Regarding people with rheumatic diseases within the study population we, as well as Garrido-Cumbrera et al. [29] noted, that the majority declared poor-wellbeing, according to the WHO-5 [29].
The two-sided negative correlation between the FCQ and the WAI scores also allows the assumption, that the higher the pandemic-related fear, the less likely patients will be to succeed rehabilitation with a satisfying return to work. In the field of rehabilitation medicine, the WAI, as measuring instrument for work ability, is rather little used compared to its use in occupational medicine. Findings regarding the ability to work during the COVID-19 pandemic, indicate e.g., good physical activity, having fewer medical conditions and ongoing therapeutic assistance in case of illness to be beneficial [30]. Other studies examining the physical activity during the pandemic, using the IPAQ, also showed a significant decrease in physical activity during the pandemic and showed an association of inactivity with a decreasing healthrelated quality of life [31]. In a Brazilian sample Cardoso et al. [32] showed fear of COVID-19 to have a negative effect on the physical activity [32]. Physical activity is known to be important to improve functionality in rehabilitants, while on current occasion inactivity is shown to be a risk factor for severe COVID-19 outcomes [32,33]. Therefore, physical and mental support is highly profitable for patients in rehabilitation.
To differentiate the interpretation of the results, the time of the elicitation of data is to be considered. The study was conducted during the third wave of the pandemic in Germany, where at the time the vaccination campaign had started, governmental ordinances restricted for example social life and implemented hygiene measures while the media was extensively reporting about the virus and its effects [34-36]. These circumstances are among others known to influence the personal perception of the risk and therefore of mental well-being [1,35]. The number of COVID-19 cases and deaths in Germany rose till the end of April and afterwards sank to a minimum. This lasted till the beginning of the fourth wave in August (“summer plateau 2021”) [37,38]. The probability of future pandemics, especially of zoonotic origin, is assumed to be growing [14]. This circumstance and the experiences of the ending SARS-CoV-2 pandemic call for measures to react efficiently in pandemics concerning the health of the population. The requirements of “pandemic preparedness” projects to identify, observe and manage public health hazards, like the international exchange of epidemiological data or create additional resources, are currently debated and for example addressed by international organizations like the EU and the WHO [39]. These actions selfevidently also concern the prevention of spreading infectious diseases. Those measures are to be acted out on governmental level as well as by any health professional, who is dealing with potential vulnerable patients.
Conclusion
Rehabilitation services are intensely needed and must be provided in critical situations to maintain the well-being of people with pre-existing conditions, like rehabilitants. Those are known to have suffered from the reduced access to rehabilitation services [40]. Given the potential for further pandemics such as SARSCoV- 2, it is important to provide education and training within the inpatient rehabilitation setting to reduce the fear of pandemics, to raise awareness and finally to improve rehabilitation outcome.
Data Availability
The German version of the FCQ is available from the corresponding author on request. The data sets used and/ or analysed during the current study are available from the corresponding author on reasonable request.
References
- Horstman C, Lewis C (2022) More COVID-19 fallout: Social isolation associated with poor health and emotional distress. Area of Focus Improving Health Care Quality.
- Dragano N, Reuter M, Berger K, Peters A, Engels M, et al. (2022) Increase in mental disorders during the COVID-19 pandemic-The role of occupational and financial strains. Dtsch Arztebl Int 119(11): 179-187.
- Spatafora F, Fialho PMM, Busse H, Helmer SM, Zeeb H, et al. (2022) Fear of infection and depressive symptoms among German University students during the COVID-19 pandemic: Results of COVID-19 international student well-being study. Int J Environ Res Public Health 19(3): 1659.
- Vindegaard N, Benros ME (2020) COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun 89: 531-542.
- Öhman A (1993) Fear and anxiety as emotional phenomena: Clinical phenomenology, evolutionary perspectives, and information-processing mechanisms. In: Lewis M, Haviland JM (Eds.), Handbook of emotions. The Guilford Press, USA, pp. 511-536.
- Adolphs R (2013) The biology of fear. Curr Biol 23(2): R79-R93.
- Baumann U, Perrez M, (Eds.), (1998) Textbook clinical psychology - psychotherapy. 2nd (edn.), Göttingen, Germany.
- St Sauver JL, Lopes GS, Rocca WA, Prasad K, Majerus MR, et al. (2021) Factors associated with severe COVID-19 infection among persons of different ages living in a defined Midwestern US Population. Mayo Clin Proc 96(10): 2528-2539.
- Mehnert A, Koch U, Sundermann C, Dinkel A (2013) Predictors of fear of recurrence in patients one year after cancer rehabilitation: A prospective study. Acta Oncol 52(6): 1102-1109.
- Salzwedel A, Völler H (2021) Cardiac rehabilitation: Patient-reported outcomes are decisive for success. Dtsch Arztebl Int 118(29-30): 505-506.
- Keller FM, Dahmen A, Derksen C, Kötting L, Lippke S (2021) Psychosomatic rehabilitation patients and the general population during COVID-19: Online cross-sectional and longitudinal study of digital trainings and rehabilitation effects. JMIR Ment Health 8(8): e30610.
- Mertens G, Gerritsen L, Duijndam S, Salemink E, Engelhard IM (2020) Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. J Anxiety Disord 74: 102258.
- Rim M, Leila R, Aicha BT, Olfa S, Meriem H, et al. (2022) Efficiency of Associating therapeutic patient education with rehabilitation in the management of chronic low back pain: A randomized controlled trial. Korean J Fam Med 43(6): 367-373.
- Marani M, Katul GG, Pan WK, Parolari AJ (2021) Intensity and frequency of extreme novel epidemics. Proc Natl Acad Sci U S A 118(35): e2105482118.
- Bailer M, Hautzinger M, Hofmeister D, Keller F (2012) Allagemain Depressions (ADS). 2nd (edn.), Hogrefe Publishers, Germany.
- Hasselhorn HM, Freude G (2007) The work ability index: A guide. Federal Institute for Occupational Safety and Health, S87, pp. 1-55.
- Frey C, Bührlen B, Gerdes N, Jäckel W (2007) IRES-3 handbook: Rehabilitation status indicators, version 3 with IRES-24 (short version). (Rehabilitation Sciences, Rehabilitation Psychology, Rehabilitation Medicine, Roderer, Regensburg, Germany 13:
- Hagströmer M, Oja P, Sjöström M (2006) The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutrition 9(6): 755-762.
- WHO Regional Office for Europe (1998) Wellbeing measures in primary health care/the DEPCARE project: Report on a WHO meeting. Sweden, World Health Organization. Regional Office for Europe, pp. 1-39.
- Cohen J (1988) Statistical Power Analysis for the Behavioral Sciences. 2nd (edn), USA, pp. 1-579.
- Buneviciene I, Bunevicius R, Bagdonas S, Bunevicius A (2022) The impact of pre-existing conditions and perceived health status on mental health during the COVID-19 pandemic. J Public Health 44(1): e88-e95.
- Martins IJ (2018) Early diagnosis and nutritional treatment stabilizes neuropsychiatric disorders. GJMR 18(A1): 1-7.
- Quadros S, Garg S, Ranjan R, Vijayasarathi G, Mamun MA (2021) Fear of COVID 19 infection across different cohorts: A scoping review. Front Psychiatry 12: 708430.
- Kontodimopoulos N, Poulaki E, Fanourgiakis J, Talias MA (2022) The association between fear of COVID-19 and health-related quality of life: A cross-sectional study in the Greek general population. J Pers Med 12(11): 708430.
- Nkire N, Nwachukwu I, Shalaby R, Hrabok M, Vuong W, et al. (2021) COVID-19 pandemic: Influence of relationship status on stress, anxiety, and depression in Canada. Ir J Psychol Med 39(4): 351-362.
- Poudel R, Daniels LB, Filippis AP, Hamburg NM, Khan Y, et al. (2022) Smoking is associated with increased risk of cardiovascular events, disease severity, and mortality among patients hospitalized for SARS-CoV-2 infections. PLoS One 17(7): e0270763.
- Mertens G, Lodder P, Smeets T, Duijndam S (2022) Fear of COVID-19 predicts vaccination willingness 14 months later. J Anxiety Disord 88: 102574.
- Wilke J, Hollander K, Mohr L, Edouard P, Fossati C, et al. (2021) Drastic reductions in mental well-being observed globally during the COVID-19 pandemic: Results from the ASAP survey. Front Med 8: 578959.
- Garrido-Cumbrera M, Marzo-Ortega H, Christen L, Plazuelo-Ramos P, Webb D, et al. (2021) Assessment of impact of the COVID-19 pandemic from the perspective of patients with rheumatic and musculoskeletal diseases in Europe: Results from the REUMAVID study (phase 1). RMD Open 7(1): e001546.
- Hunter JR, Meiring RM, Cripps A, Suppiah HT, Vicendese D, et al. (2021) Relationships between physical activity, work ability, absenteeism and presenteeism in Australian and New Zealand adults during COVID-19. Int J Environ Res Public Health 18(23): 12563.
- Schmidt T, Heuer AK, Weisser B (2021) Effects of COVID-19 confinement on physical activity and health-related quality of life in rehabilitation patients. Dtsch Z Sportmed 72(5): 230-235.
- Martínez VN, Cadore EL, Casas HÁ, Idoate SF, Izquierdo M (2016) Physical activity and early rehabilitation in hospitalized elderly medical patients: Systematic review of randomized clinical trials. J Nutr Health Aging 20(7): 738-751.
- Sallis R, Young DR, Tartof SY, Sallis JF, Sall J, et al. (2021) Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients. Br J Sports Med 55(19): 1099-1105.
- Ulrike Illner (2023) Corona in the media. PMG Presse-Monitor.
- Lippke S, Keller FM, Derksen C, Kötting L, Dahmen A (2022) Hygiene behaviors and SARS-CoV-2-preventive behaviors in the face of the COVID-19 Pandemic: Self-reported compliance and associations with fear, SARS-CoV-2 risk, and mental health in a general population vs. a psychosomatic patients sample in Germany. Hygiene 2(1): 28-43.
- (2021) COVID-19: Timeline of EU action in 2021. Current European Parliament.
- Tolksdorf K, Loenenbach A, Buda S (2022) Third update Dare "Retrospective fasinaintailung dare Covid-19-Pandemi in Germany". Robert Koch Institute, Germany.
- (2023) WHO Coronavirus (COVID-19) Dashboard.
- Samarasekera U (2021) New EU health programme comes into force. Lancet 397(10281): 1252-1253.
- Boldrini P, Garcea M, Brichetto G, Reale N, Tonolo S, et al. (2020) Living with a disability during the pandemic. "Instant paper from the field" on rehabilitation answers to the COVID-19 emergency. Eur J Phys Rehabil Med 56(3): 331-334.
© 2023 Andreas Schwarting. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






