- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
Effectiveness of the Health Service Responds in Andalusia during the State of Health Alert by Covid-19
Martínez MF1*, Martos SS1, Donaire LO1, Martínez CF1 and Carrasco MP2
1Department of Nursing, Spain
2University of Seville, Spain
*Corresponding author:María Fernández Martínez, University of Jaen, Spain
Submission: December 10, 2022; Published: May 05, 2023

ISSN 2637-7934 Volume4 Issue2
Abstract
Objectives: To determine the effectiveness of the Salud Responde service during the pre-pandemic,
pandemic and post-pandemic periods, as well as the evolution of the service between both periods.
Methodology: A descriptive cross-sectional study was carried out based on calls received at the reference
telephone number in Andalusia for health care during three specific time periods: January 1, 2019 -
December 31, 2019, March 14, 2020-June 21, 2020, and January 1, 2021-December 31, 2021.
Result: The results show a clear increase in management during the pandemic period, as well as a change
in the use of portfolios and the resolution of portfolios. A clear upward trend is evident in the number of
calls and consequently time in queues, as well as total call time.
Conclusion: The extensive experience in telephone care and health services management places Salud
Responde as an ideal medium to continue implementing new telemedicine projects, in addition to
continuing to execute its broad portfolio of services.
Keywords:Telemedicine; COVID; Health system; Health care; Pandemic
Introduction
The SARS-CoV-2 pandemic forced the reorganization of traditional healthcare in all countries of the world to create an epidemiological safety framework to prevent infection of both users and healthcare personnel. Its impact led to the collapse of healthcare and highlighted the misuse of the emergency system by users [1]. A health emergency was declared, and protective measures were adopted, causing important changes at the economic, social and public health levels. Lack of knowledge, fear and scarce information about the virus were sufficient reasons for the health service to become chaotic and unsustainable. Health centers collapsed because by the pandemic situation, both for appointments and emergencies. Many sectors have seen the need to reinvent themselves and turn to innovation to move forward with their routines and commitments, and the healthcare sector is no exception. As Yuval Noah Harari points out: „All emergencies accelerate processes that were already underway”; and, according to political scientist Robert Kaplan [2]: „Crises, like wars, make history move faster. In order to control this pandemic worldwide, a series of measures were adopted, such as home confinement, the use of masks and social distancing. The result of these preventive interventions has generated, at the same time, changes at the economic, social and public health levels. Psycho-emotional and occupational problems have increased, directly affecting the population in general but specifically patients diagnosed with chronic diseases due to the reduction of controls and medical visits. Different studies show that the pandemic has caused multiple consequences for the population [3-8]. Mental health has been affected in such a way that the demand for antidepressant drugs and sleep inducers has increased; numerous young people have developed mental problems during this period suffering from tiredness, sadness, insomnia, anxiety, depression, loss of appetite and difficulty concentrating; and feelings of uncertainty, fear and insecurity have been experienced by the majority of the population. Providing health care while respecting social distancing has been a very difficult task. In Spain, following the declaration of a state of alarm on March 14, 2020, many face-to-face medical consultations were replaced by telephone consultations in order to limit healthcare contact and thus slow the spread of the virus. Telephone consultations represent a small part of a broader concept known as telemedicine. The World Health Organization (WHO) defines telemedicine as „the provision of health care services by all health professionals using information and communication technologies when distance is an important factor”. Tele-consultations are a safe and effective way to assess suspected cases and guide patient diagnosis and treatment, minimizing the risk of disease transmission. These teleconsultations have allowed many of the clinical services to continue to operate on a regular basis [9-11].
The Ministry of Health of the Regional Government of Andalusia launched the information and services center „Salud Responde” in 2003 with the aim of approaching health care to citizens from an integral perspective and in an innovative way, since it allows access to the services and benefits of the Andalusian Public Health System, from any point in the Andalusian community. Salud Responde is the reference service for citizen care in Andalusia, responding to more than eight million people, improving access to Andalusian public health, rationalizing and optimizing health services, reducing waiting times, avoiding unnecessary trips to users, responding to the needs of information, health and administrative management of citizens and health professionals 24 hours a day, 365 days a year [12,13]. It has a wide range of services, among which the following are worth mentioning: Appointments with family doctors, pediatricians and nurses, health advice, management of health campaigns in Andalusia, free choice of hospital, access to the Registry of Advance Vital Wills in Andalusia, processing of second medical opinion, free choice of hospital, information on the Decree of guarantee of response time in health care processes, monitoring of hospital discharges during weekends of patients at special risk, Andalusian plan for prevention against the effects of heat, linguistic translation service, tobacco information telephone number, sexual and reproductive health information telephone number, telecontinuity of palliative care, vaccination campaigns... Currently, and after nineteen years of experience, Salud Responde has made it possible to improve the population’s access to the Andalusian Public Health System, rationalize and optimize health, economic and technological services, reduce waiting times and avoid unnecessary trips for users. During the course of the SARS-CoV2 pandemic, the Salud Responde telephone has been the reference telephone number for public attention in Andalusia [14-16].
Materials and Methods
descriptive cross-sectional study is carried out based on calls
received at the reference telephone number in Andalusia for health
care during three specific
a) Time periods:
January 1, 2019 - December 31, 2019
March 14, 2020- June 21, 2020
January 1, 2021 - 31 December 2021
b) Inclusion criteria: Patients and/or family members who
have used the Salud Responde service in Andalusia during the
periods under study.
c) Exclusion criteria: Interruption of the call prevents
complete data collection.
The study guarantees the confidentiality of the data according to Regulation (EU) No. 2016/679 General Data Protection Regulation (RGPD; and Organic Law 3/2018, of December 5, on Personal Data Protection and guarantee of digital rights. The authors declare no conflicts of interest. Se realizó un análisis descriptivo previo con variables cualitativas y variables cuantitativas (es decir, medidas de tendencia central y dispersión) [17]. In turn, an exploratory analysis of all data was performed to identify the distribution of variables and a comparison between groups was performed (i.e., a bivariate analysis of qualitative variables with the chi-square test, and of quantitative variables using the ANOVA test after checking for normality). The Kruskal-Walli’s test was applied when necessary. In the case of a comparison between two quantitative variables, Pearson’s test was used for parametric samples and Spearman’s test if the variable had nonparametric behavior. All analyses were performed with SPSS® version 24.0. A value of p<0.05 was established as statistically significant. The G Power 3.1.9.4® program was used to calculate the sample size, introducing an alpha error of 0.05, a power of 99% and an effect size of 0.5. The result was 127 people for each group. Finally, the universal sample was chosen for the analysis periods. This sample far exceeded the minimum requirements [18].
Result and Discussion
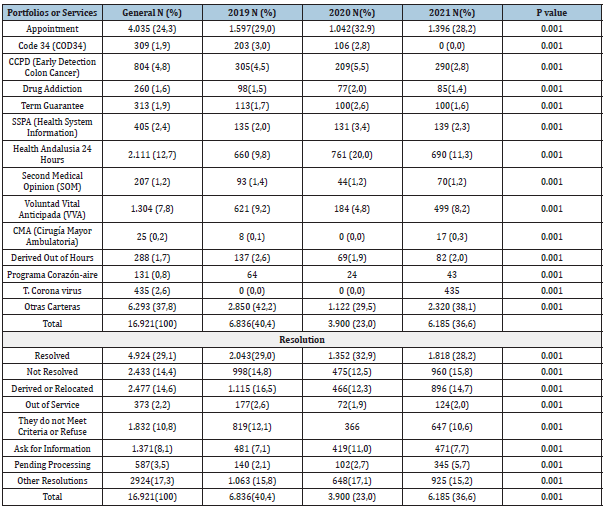
The total sample of observations was constituted by 16,921, being by years 6,836 in the year 2019, 3,900 in the year 2020 and finally 6,185 in the year 2021 [19]. An overall evaluation of the data was made with respect to the number of calls: answered calls, unanswered calls, time in queue and call time. Adema was broken down by year between the periods from March 14, 2019, to June 20, 2019, March 14, 2020 to June 20, 2020 and March 14, 2021 to June 20, 2020 (Table 1). There was an exponential increase in the number of calls, answered and unanswered calls in the pandemic period compared to the pre-pandemic period. Regarding the service portfolios, 41 were identified for this work, although they were grouped into 14 types for a better global vision. On the other hand, 135 types of resolutions were distinguished with respect to the calls attended, being unified into a total of 8 types for better data processing (Table 2). Significant differences are observed in the evolution of both the portfolios of services and their resolution. The demand for some service portfolios decreases during the pandemic period, such as DPCC, drug dependence, Heart-Air program... However, a considerable increase in other service portfolios is observed during this period, such as T. Coronavirus, Salud Andalucía 24h and previous appointment. With respect to resolution, a drop is observed in 2020, which coincides with the peak period of the pandemic [20].
Table 1: Descriptive analysis of the pre-pandemic, pandemic and post-pandemic period of the calls received at the Health Responds service.
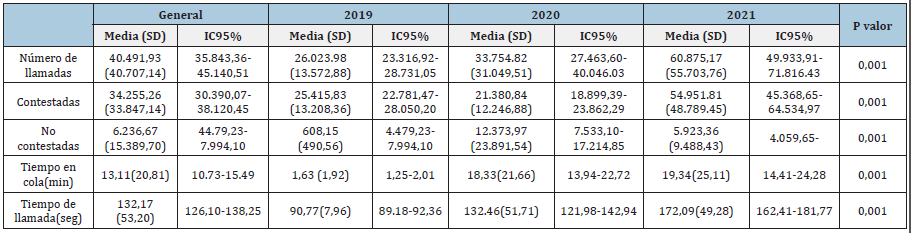
Notes: SD=Standard deviation; 95% CI=95% Confidence Intervals. Min=Minutes.
Table 2: Portfolio analysis and resolution of calls received during the pre-pandemic and post-pandemic period.
Inferential analysis
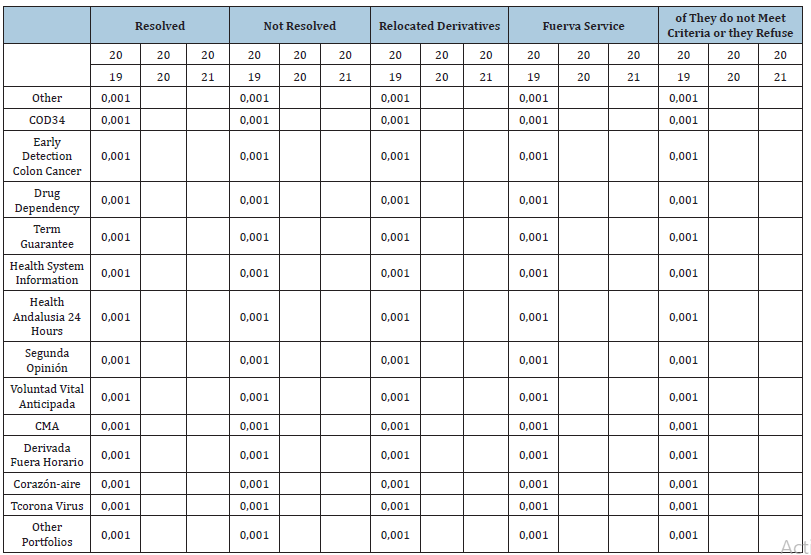
An analysis was performed to assess the relationship between the type of resolution of greatest interest and the portfolios under study by years of study (Table 3). Significant differences are evident in all portfolios with respect to resolved, unresolved, referred, and non-criteria interventions compared to pre-pandemic and pandemic years [21]. Finally, the correlation between the number of calls and waiting time or latency was evaluated, as well as the number of calls and whether or not they were answered. This correlation was evaluated independently by year. A direct correlation was observed in practically all items during the prepandemic and pandemic years, except for call time, which was only significant with a medium-high correlation in the year 2021, where demand was highest. There are strong correlations between the number of calls answered calls, unanswered calls and queue time in all the years evaluated [22,23].
Table 3: Portfolios of services most in demand by years of study.
Conclusion
The results show a clear increase in management during the pandemic period, as well as a change in the use of portfolios and portfolio resolution. There is a clear upward trend in the number of calls and consequently in queue time, as well as in total call time. During the pandemic, face-to-face consultation has been avoided on most occasions, giving priority to telephone advice or telephone medical appointments. Telephone appointments have been implemented on a permanent basis and many users now prefer a telephone appointment with their doctor rather than a face-to -face visit to the center. There are portfolios of services that during the pandemic period have had very low or virtually no activity. At certain times during the pandemic, the Salud Responde service has been overwhelmed and because of this, work has been prioritized [24]. If we analyze these data in detail, it can be seen how the DPCC, drug dependence, SOM, VVA and Corazón-Aire service portfolio have seen a considerable decrease in their activity, however, Salud Andalucía 24h and coronavirus triage and prior appointment have increased their activity considerably. Regarding the number of calls, a considerable increase is observed since 2019, experiencing a peak in 2021. With respect to the number of unanswered calls, a maximum increase is observed in 2020 coinciding with the period of full pandemic and gradually decreasing as the year 2021 progresses. User waiting time has shown a maximum peak in the year 2021 being about 19 minutes. Many patients with chronic diseases suffered problems in the management of their pathology (patients with arterial hypertension or diabetes) during the pandemic period. Tejera et al. conducted a retrospective observational study which showed that most of the diabetic participants experienced problems in the management of diabetes during the pandemic and through telemedicine services most of them were able to acquire better control of their diabetes [25-27]. Telemedicine has been of great benefit to these patients since, due to the restrictions caused by the pandemic, there was little or no access to health care services for the management of patients with chronic conditions.
Similarly, Allyson Myers piloted a randomized clinical trial from which it was found that the results achieved through telephone consultations and video consultations were similar. Seventy-five percent of the patients who completed the study indicated a high level of satisfaction with the use of telemedicine in the follow-up and control of their chronic pathology. Yogini et al. conducted a retrospective observational study involving healthcare professionals. The results showed that 80% of the healthcare professionals switched to telephone consultations during the pandemic and 6% by video consultations, while only 14% continued to make their consultations in person at the healthcare center. Thirty-eight percent stated that diabetes was the chronic disease most affected by the reduction in health care resources due to Covid-19, followed by chronic obstructive pulmonary disease with 9%. 71.3% acknowledged that the resources provided during the pandemic for chronic disease management were insufficient [28].
Ranjit Mohan carried out a retrospective observational study in which the following results were obtained: only 15% of the participants managed to consult their physician during confinement, the main reason for consultation being the review of the treatment of a chronic pathology with 84.6%. Of those who tried to consult, 78.6% were unable to go to the clinic due to the restrictions established during the pandemic. Of the total sample that made use of telemedicine, 82% were satisfied and interested in continuing telemedicine services after the pandemic. Nancy Samir designed a cross-sectional study whose results showed that 16.7% of the healthcare professionals who participated in the study had face-to- face consultations, while the majority of the professionals only offered remote consultations. Among the remote consultations, telephone consultations (32%) and by video call (18%) stood out. For patients with new-onset diabetes, 38% of the health professionals stated that they had offered a first face-to-face consultation using the appropriate personal protective equipment and subsequently follow-up continued to be carried out remotely (telephone or video consultation) [29].
References
- Bellón JA (1993) Consultation of the family doctor: How to organize the work consultation on demand. In: Gallo FJ (Ed.), Community and family medicine resident's manual, Spain, pp. 275-286.
- Rosekrans J, Limbo D, Kaplan D (1981) Telephone consultations in pediatrics. Patient Care Publications, USA.
- Black KL, Caufield C (2007) Standardization of telephone tri-age in pediatric oncology. J Pediatric Oncol Nurs 24(4): 190-199.
- Light PA, Hupcey JE, Clark MB (2005) Nursing telephone triage and its influence on parents’ choice of care for febrile children. J Pediatr Nurs 20(6): 424-429.
- Schroeder K, Chan WS, Fahey T (2011) Recognizing red flags in general practice. InnovAiT 4(3): 171-176.
- Galen LSV, Car J (2018) Telephone consultations. BMJ 360: 1047.
- Gupta SG (2013) Tips for telephone and electronic medical consultation. Indian J Pediatr 80(11): 944-948.
- Shah K, Kamrai D, Mekala H, Mann B, Desai K, et al. (2020) Focus on mental health during the coronavirus (COVID-19) pandemic: Applying learnings from the past outbreaks. Cureus 12(3): e7405.
- Famina S, Farooqui AA, Caudill RL (2020) Early use of tele-psychotherapy in resident continuity clinics-our experience and a review of literature. Mhealth 6: 1.
- Varela MZ, Sierra AG, Ledo PR (2011) Quantification and nature of reasons for consultation in family medicine. SEMG 136: 86-91.
- Seewon R (2009) Telemedicine: Opportunities and developments in member states: Report on the second global survey on eHealth 2009. Healthc Inform Res 18(2): 153-155.
- (2021) Consumption and social welfare: Quality plan for the national health system. Ministry of Health, India.
- (2020) Strategy for early detection, surveillance and control of COVID-19. Ministry of Health, India.
- (2021) International council of nurses update on COVID-19. International Council of Nurses (ICN), Switzerland.
- Sotos JR, Martínez IP, Hidalgo JLT, Pretel FA, Bravo BN (2011) Information technologies and telecommunications: Telemedicine. Clinical Journal of Family Medicine 4(1): 42-48.
- Hjelm NM (2005) Benefits and drawbacks of telemedicine. J Telemed Telecare 11(2): 60-70.
- Blanca J, Muñoz R, Caraballo M, Expósito M, Sáez R, et al. (2008) Privacy in the hospital, the experience of patients, their families and nurses. Index Sick 17(2): 106-10.
- Spanish Collegiate Medical Organization (2001) Bulletin nº70, Guidelines of the standing committee of European physicians for doctor/patient electronic correspondence, Spain.
- Spanish Collegiate Medical Organization (2003) Bulletin nº100, ’EU quality criteria for health-related websites, Spain.
- Spanish Collegiate Medical Organization (2013) Bulletin nº390, Legal framework applicable to telemedicine in the EU, Spain.
- (2022) Ministry of Health and Consumption. Health Answer, Andalusian Health Service, Spain.
- (2022) Ministry of Health and Consumption. Know us, Andalusian Health Service, Spain.
- Consumption and social welfare: Quality plan for the national health system. Ministry of Health, India.
- Toni S (2020) A virtual nurse practitioner led clinic during COVID-19. ANMJ, Australia.
- (2020) Europa Press, Spain.
- Cortes N (2020) Digital health: Telemedicine takes center stage in times of covid-19.
- Yusta C (2020) Controlling diabetes in times of pandemic: The importance of telemedicine. The Spanish, Spain.
- Organic Law (2018) Protection of personal data and guarantee of digital rights. Official state gazette, India.
- Pacheco A, Chacon K (2018) Teleconsultation effectiveness; Follow-up of patients after receiving teleconsultation in a program in public hospitals: Chihuahua Mexico. Latin Am J telehealth 5(3): 304-312.
© 2023 Martínez MF. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






