- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
Determining Intervention Strategy for Stroke: Literature Review, Risk Analysis Tool, and Risk Management
Lisa Marie Portugal*
Health and Wellness Education, American College of Education, USA
*Corresponding author:Lisa Marie Portugal, Health and Wellness Education, American College of Education, USA
Submission: November 29, 2022; Published: January 05, 2023

ISSN 2637-7934 Volume3 Issue5
Abstract
A risk analysis tool can aid in helping to ensure an appropriate level of healthcare intervention for target populations in need. Efficient risk analysis assists healthcare practitioners in making decisions in targeting essential health resources for communities and individuals. This discussion includes a literature review for stroke focusing on detection, surveillance, and holistic natural best practices for stroke prevention and health management. Themes, trends, and areas for future study regarding stroke management and prevention are examined. Focus on the development of a risk analysis tool to address public health concerns related to stroke is discussed. The stroke risk analysis tool contains eight categories of stroke related factors that can be identified and mitigated by the public and healthcare practitioners to change negative behavioral choices into positive lifestyle actions. Supporting research is evaluated to examine stroke identification, intervention, and prevention strategies to assist healthcare practitioners and the public with this chronic health condition that can be managed in a holistic manner via proactive and comprehensive education.
Keywords:Stroke detection and surveillance; Hemorrhagic and ischemic stroke; Stroke management; Risk factors; Cardiovascular disorders; Physical inactivity; Dyslipidemia; Obesity; Diabetes and hypertension; Risk analysis tool; Risk management; Lifestyle changes
Introduction
Stroke surveillance and detection measures can aid healthcare practitioners in planning, preventing, and forecasting appropriate actions. Sociopolitical influences, global communications, and technology improvements result in a swiftly transforming epidemiologic environment. Healthcare professionals should be involved in understanding and reviewing relevant surveillance and detection practices to effectively address stroke in public health. Stroke is a main cause of disability and the second leading contributor of death globally with ischemic stroke being the most common form [1]. According to Ayaka et al. [2], a significant connection was detected between narrower retinal venular caliber and higher intakes of potassium, vitamin C, and A. Systemic diseases such as cardiac or renal diseases, stroke, diabetes, and hypertension have an association with retinal vasculature changes [3]. Retinal vessel caliber is affected by determinants such as pathological [smoking, dyslipidemia, atherosclerosis] and physiological [body mass index, blood glucose, blood pressure, race, sex, and age] [3]. Assessing retinal vessels provides data about the pathophysiology of multiple diseases and can be used as a screening method to predict health risks and disease occurrence [2,3]. Multiple studies discovered vitamins C and A, with antioxidant properties, contribute to minimizing the risk of stroke and coronary heart disease [2,3].
Ayaka et al. [2] disclosed that a diet abundant in high-quality vegetables and fruits can be attributed to narrower retinal venular caliber and improved retinal microvascular health. Potassium, vitamin C, and vitamin A can be ingested via vegetables and fruits and findings of the Ayaka et al. [2] study indicated consistency with improved retinal microvascular health and higher intakes from these natural dietary nutrients. The study is the first time that a connection has been demonstrated between the dietary intake of potassium, vitamin C, and A with retinal vascular status, therefore, additional studies in this area should be conducted to assess evidence consistency [2]. Herpich & Rincon [4] collected professional guidelines on stroke management within the last 10 years, observational studies, current clinical trials, and landmark studies in a review of acute ischemic stroke management practices. Findings indicated that the management of ischemic stroke goes well beyond hospital admission and involves a multidisciplinary approach to reduce morbidity and mortality [4]. A notable trend in the United States is the rising number of patients with stroke risk factors such as hyperlipidemia, hypertension, and diabetes [4]. Future stroke management should involve a shift toward patient prevention and education to minimize the occurrence of stroke leading to death and severe disability [4].
According to Kleindorfer et al. [5], guidelines for secondary
stroke prevention should involve lifestyle, nutrition, and diet
changes with high consumption of fiber, vegetables, fruits, and the
Mediterranean diet. A 39% increased risk of stroke was evident
in individuals adhering to a Southern diet that included sugarsweetened
beverages, processed meats, fried foods, and high in
added fats [5]. Lower stroke rates are evident with high potassium
consumption [5]. Educational interventions involving moderate
to vigorous physical activity can be delivered in lifestyle-based
multimodal programs to reduce stroke occurrence [5]. Specific
areas for future research and knowledge gaps included the
following:
a) Actions for managing social determinants of health
amongst survivors of stroke.
b) Amongst populations at most risk for inequities,
identifying approaches for improving control over risk factors.
c) Developing distinctions of understanding regarding
inequity in risk factor control following stroke, in addition to
social determinants of health.
d) Developing comprehensive understanding of communities
experiencing inequity in risk factor control following stroke [5].
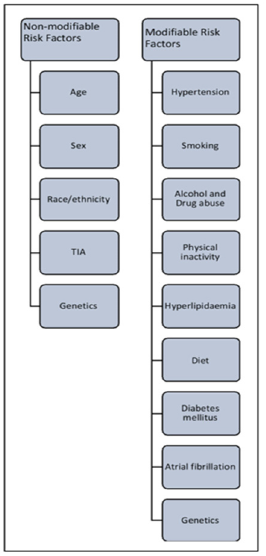
Additional research is necessary to discover best practices and approaches for minimizing inequity in risk factor control following stroke [5]. Stroke management relies on treating pathophysiology while stroke prevention involves modifying risk factors within individuals or populations [1]. Significant challenges faced by stroke researchers involve defining essential mechanisms underlying therapeutics, generating reproducible data, performing pre-clinical multi-center trials, and increasing translational value of data before undertaking clinical studies [1]. The following figure lists non-modifiable and modifiable stroke risk factors (Figure 1). Li et al. [6] evaluated the safety and efficacy of Ginkgo biloba extract on patients with acute ischaemic stroke, in addition to its impact on vascular events recurring. In combination with aspirin treatment, findings by Li et al. [6] reported that Ginkgo biloba extract relieved neurological and cognitive deficits following acute ischaemic stroke without rising occurrence of vascular events. Findings indicated that stroke patients receiving Ginkgo biloba extract experienced improved neurological functions, executive functions, and memory function in daily life [6]. Ginkgo biloba extract may be a promising medication for dementia and Alzheimer’s [6].
Figure 1:Stroke risk factors - non-modifiable and modifiable [1].
Determining Intervention Strategy, Analysis Tool, and Risk Management
A commonly known cerebrovascular disease is hemorrhagic and ischemic stroke that can occur by non-modifiable and modifiable risk factors. Typical non-modifiable stroke risk factors are race and age. However, cardiovascular disorders, physical inactivity, dyslipidemia, obesity, diabetes, and hypertension are significant modifiable risk factors [7]. Health practitioners working with the public and stroke survivors should understand molecular mechanisms mediating these risk factors to aid in significantly contributing to the development of effective treatments, enhancing rehabilitation, preventing neural damage, and lowering stroke risk [7]. The most typical mechanisms culpable for stroke occurrence involve altered activities/expression of many channels and signaling proteins, excitotoxicity, impaired synaptic transmission, apoptosis and inflammation, neural oxidative stress, reduced cerebral blood flow, atherosclerosis, vasoconstriction, thrombosis, abnormal condition in blood vessels, and abnormalities in the blood-brain barrier [7]. Hemorrhagic and ischemic stroke is associated with many clinical disabilities and manifestations that can develop early in life or much later [7]. Lowering stroke burden requires identifying underlying risk factors and developing targeted educational programs and potential holistic therapies. Early identification of modifiable stroke risk factors is crucial in significantly aiding the reduction of stroke with immediate diagnosis and intervention [7]. Stroke education, monitoring, tracking, and engagement activities can be developed for the public by knowledgeable healthcare practitioners with the understanding of stroke risk factors and mitigating holistic therapeutics.
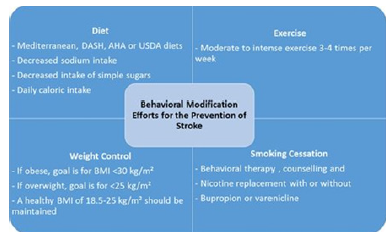
Figure 2:Behavior modification for stroke [9].
In a trial study conducted by Guillaumier et al. [8], the efficacy of a behavioral change intervention via an online platform to aid in the prevention of a second stroke was evaluated. The program was administered to stroke survivors to aid in improving quality of life. The study findings indicated that an online platform can be effectively used to manage and improve stroke survivors’ selfreported scores related to health improvements and can provide a helpful tool to support and engage some survivors of stroke [8]. Users of the stroke survivors’ health monitoring tool were asked to set goals and document progress throughout 6 important areas which included blood pressure, mood and feelings, nutrition, activity, alcohol, and smoking [8]. The randomized controlled trial included the participation of adult stroke survivors who were given access to the online health tracking and documentation program over a twelve-week period. The control group was given a list of websites with generic health information. The participating stroke survivors completed a survey at 6 months after the first initial survey was given in the beginning of the trail study [8]. The stroke survivor participants with access to the online health monitoring tool scored overall wellbeing and health, on average, 5 points higher over the controlled group that were only given a list of websites with generic health information [8]. Thus, a conclusion can be drawn that when stroke survivors are given access to actively participate and engage in an online stroke prevention program, health and wellbeing may be effectively changed and monitored in a positive manner.
The following graphic highlights various behavioral medication strategies for stroke risk factors (Figure 2 & Table 1).
Table 1: Stroke risk analysis tool.
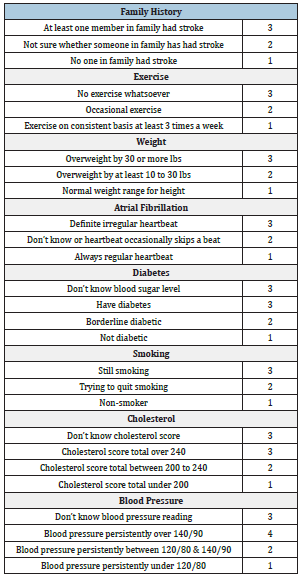
Scoring mechanism
Use the following scoring categories to understand which areas need to be addressed to understand stroke risk factors. From the eight categories listed, only family history is uncontrollable. However, mitigating stroke risk can be accomplished through holistic healthcare education and positive behavioral lifestyle changes that enhance and promote wellbeing in any population.
Risk is high - 20 to 24: According to the American Stroke Association [10], 80% of strokes are preventable A comprehensive and holistic action plan can aid in addressing behavioral and lifestyle changes to reduce stroke risk.
Risk is elevated- 16 to 19:Work with holistic healthcare practitioners to develop a comprehensive action plan to address reducing stroke risks. When individuals score two or more in the high blood pressure category, concentrate on this area as this is the number one factor related to stroke.
Risk is moderate - 12 to 15:When individuals fall into this category, a higher probability of stroke is prevalent and action should be taken to minimize these scores. When scoring three for not knowing one’s blood sugar level, cholesterol score, or blood pressure reading, individuals should visit with a qualified holistic healthcare practitioner to examine these important risk factors related to the occurrence of stroke.
Risk is low - 8 to 11:Eight is the lowest possible score as everyone can have some risk level for stroke. If individuals score three for not knowing blood sugar level, cholesterol score, or blood pressure reading, one should be proactive in visiting with a holistic naturopathy doctor, functional medicine MD, functional medicine chiropractor, Traditional Chinese Medicine doctor, and/or Ayurveda practitioner to determine stroke risk factors.
Individuals can choose the other seven categories to start taking proactive and positive steps in lowering scores. When this is achieved in one category, individuals can work on maintaining low score levels while addressing negative lifestyle risk factors in other categories that can be controlled through behavioral changes and consciously making positive choices. Helping the public understand risk for stroke can aid in helping individuals begin the process of making choices to lower risk (Figure 3).
Figure 3:Hippocrates.

Conclusion
Stroke surveillance and detection measures can aid healthcare practitioners in planning, preventing, and forecasting appropriate actions. Healthcare professionals should be involved in understanding and reviewing relevant surveillance and detection practices to effectively address stroke in public health. Stroke continues to be the fourth leading cause of death worldwide [9]. A stroke risk analysis tool for tracking, monitoring, and health education engagement can aid in minimizing stroke occurrence as well as assisting stroke survivors in mitigating second stroke occurrence. Recent research in non-modifiable and modifiable stroke risk factors has enabled healthcare practitioners and the public to identify how to prevent, mitigate, and educate individuals with high stroke risk factors. Furthermore, identifying strategies to target at-risk populations can be designed to prevent stroke and provide targeted holistic therapeutics. Targeted lifestyle modification health education programs can be developed by healthcare practitioners to help the public reduce stroke occurrence with diet, exercise, weight control, smoking cessation, and reduced alcohol consumption. Finally, teaching self-advocacy skills in healthy living and healthy lifestyle choices is critical.
References
- Kuriakose D, Xiao Z (2020) Pathophysiology and treatment of stroke: Present status and future perspectives. International Journal of Molecular Sciences 21(20): 7609.
- Ayaka E, Gemala ID, Kazuyuki H, Rie T, Irfan KM, et al. (2022) Dietary vitamins A, C, and potassium intake is associated with narrower retinal venular caliber. Frontiers in Medicine 9: 818139.
- Dumitrescu AG, Voinea L, Badarau IA, Paun VA, Schowe M, et al. (2017) Update on retinal vascular caliber. Romanian Journal of Ophthalmology 61(3): 171-180.
- Herpich F, Rincon F (2020) Management of acute ischemic stroke. Critical Care Medicine 48(11): 1654-1663.
- Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, et al. (2021) 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline from the American Heart Association/American Stroke Association. Stroke 52(7): e364-e467.
- Li S, Zhang X, Fang Q, Zhou J, Zhang M, et al. (2017) Ginkgo biloba extract improved cognitive and neurological functions of acute ischaemic stroke: A randomised controlled trial. Stroke and Vascular Neurology 2(4): 189-197.
- Alkahtani R (2022) Molecular mechanisms underlying some major common risk factors of stroke. Heliyon 8(8): e10218.
- Guillaumier A, Spratt NJ, Pollack M, Baker A, Magin P, et al. (2022) Evaluation of an online intervention for improving stroke survivors’ health-related quality of life: A randomised controlled trial. Plos Medicine 19(4): e1003966.
- Boehme AK, Esenwa C, Elkind MS (2017) Stroke risk factors, genetics, and prevention. Circulation Research 120(3): 472-495.
- (2022) American Stroke Association.
© 2023 Lisa Marie Portugal. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






