- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
Dislocation Following Total Knee Arthroplasty-A Case Report of an Impactful Entity
André Varandas-Borges1, Ana Teixeira-Vaz2, Rodrigo Correia1, Miguel Correia1 and Ismael Carneiro1
1North Rehabilitation Center, Vila Nova de Gaia, Portugal
2São João University Hospital Center, Portugal
*Corresponding author: André Varandas-Borges, North Rehabilitation Center, Vila Nova de Gaia, Avenida Infante Sagres, 22, Valadares, Portugal
Submission: October 23, 2022; Published: November 18, 2022

ISSN 2637-7934 Volume3 Issue5
Abstract
Total Knee Arthroplasty (TKA) is one of the most performed orthopedic procedures. However, it is not hassle-free. Posterior dislocation is an infrequent complication, although it has multiple clinical and functional implications. We present this case highlighting the importance of this diagnosis in Physical Medicine and Rehabilitation (PMR) clinical practice. A 72-year-old woman with disabling left knee pain and gait unsteadiness was diagnosed with severe osteoarthritis and proposed to TKA. There was no report of complications during or immediately after the surgery. Three weeks later, the patient was admitted to a Rehabilitation Center (RC) to ensure proper functionality reestablishment. On the fourth day at the RC, a sudden irreducible 90-degree left knee flexion position was stated, together with significant knee deformity. After clinical and imaging testing, a posterior TKA dislocation was diagnosed. Surgical revision, with TKA replacement, was performed. TKA posterior dislocation is an uncommon complication after TKA. Nevertheless, the high clinical and functional burden requires special care from the clinician. Traumatic events, low-energy falls, and forced knee hyperflexion are described as the main mechanisms of injury. Besides, it is thought that obesity, knee varus or valgus deformity, flexion contracture, and either peripheral or central neurological impairments play a significant predictive role in this TKA complication. We report a patient whose main risk factors were obesity and knee varus deformity, even though no precise mechanism of injury was depicted.
Keywords: Total knee arthroplasty; Prosthesis dislocation; Orthopedics complications; Rehabilitation
Introduction
Total Knee Arthroplasty (TKA) is one of the most performed orthopedic procedures, with demonstrated successfulness and cost-effectiveness [1,2] and a 3-4% increase per year of patients submitted to this surgery is estimated until 2030 [3]. Similarly, to other medical and surgical procedures, TKA is not hassle-free, with the possibility of being associated with complications. Delayed healing of the surgical wound, soft tissue or joint infection, deep venous thrombosis, post-surgical joint stiffness, perioperative fractures, changes in patellar tracking, osteolysis, aseptic unfastening of the prosthesis, instability, and polyethylene wear are the most frequent complications [4,5]. TKA dislocation is a rare complication, and its frequency is estimated to be between 0.15% to 0.5% [1]. This complication may occur due to a failure of the locking mechanism in knee extension, which may be associated with surgical technique, trauma, or even medical device failure [6-8].
Case Presentation
We present the case of a 72-year-old female with hypertension, previous right TKA and unicompartmental left knee arthroplasty. The patient was observed on an orthopaedic outpatient appointment due to persistent left knee pain, with gait unsteadiness, in relation to severe osteoarthritis, despite the previous surgery. These complaints impacted autonomy, precluding hygiene, dressing, mobility, and participation, leading to social isolation and quality of life loss. The conversion of the unicompartmental prosthesis to a TKA was performed, and no peri or early post-operative complications were reported. After three weeks, the patient was admitted to a Rehabilitation Center (RC) to ensure the best rehabilitation outcomes. At admission, the patient had significant pain (8/10, accessed through the Numerical Scale of Pain), characterized as mechanical, with no irradiation nor factors of improvement or worsening. She had a globous knee, with a varus deformity, with a slight increase in temperature compared to the contralateral side, and a limited knee range of motion (ROM) was depicted (0° extension and 90° flexion with pain in the extreme ROM). The scar had no complications or significant alterations, and the sensitive-motor assessment was normal. Functionally, the patient scored 90 in the Functional Independence Measurement, requiring little help in transfers, verticalization, and orthostatism; gait was possible for less than 50m, using two crutches and supervision. As such, a multimodal rehabilitation program was prescribed to ensure pain control, ROM recovery, balance normalization, and gait independence with one or none assistive devices.
The patient was at an early stage of rehabilitation, so ROM restoration was limited between 0 to 60-90 degrees. Transcutaneous electrical nerve stimulation was used to control pain (C type, 100Hz). Muscle strengthening was performed mainly with bedside exercises, focusing on ankle pumps, quadriceps sets (isometric), gluteal max sets (isometric), and heel slides. Initially, gait training was performed with an appropriate assistive device (150 meters with a rolling walker). Transfer and mobility training (bed mobility, toilet transfer, rolling walker instruction, sit-to-stand) was supervised by the nursing and physical therapy team. On the fourth day at the RC yard, a sudden 90-degree flexion deformity of the left knee was depicted, with anterior dislocation of the femoral condyles (Figure 1). The patient reported an enhancement of the pain severity (scoring, at this time, 10 out of 10 on the Numerical Scale of Pain), accompanied by significant functional disability. Due to these clinical manifestations, the patient was transferred to a tertiary-care center. An etiological study was performed with eco-Doppler, excluding a significant vascular injury and knee radiographs (Figure 2), that confirmed posterior TKA dislocation. The patient underwent replacement of the TKA, which was uneventful (Figure 3).
Figure 1:Knee dislocation.
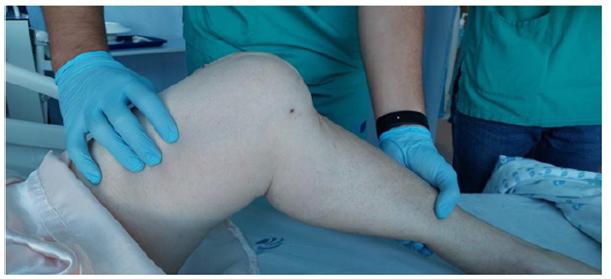
Figure 2:Dislocated primary prosthesis cruciate-retaining arthroplasty.
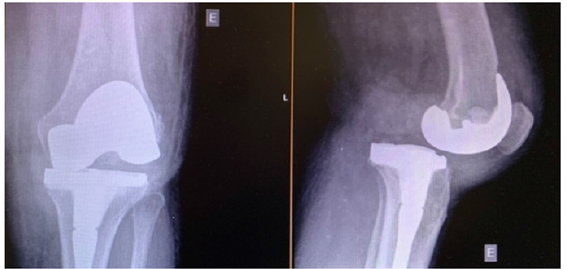
Figure 3:Revision prosthesis with constrictive knee arthroplasty with femoral and tibial discharge rods.

Discussion
We report the case of a rare, although clinically significant, TKA complication: The posterior dislocation. As aforementioned, this clinical condition presents with knee pain, joint deformity, and functional disability, requiring urgent referral, diagnosis, and etiological study. In most cases, surgical management is needed to restore normal knee function. Regarding posterior TKA dislocations, up to 80% occur with posterior dislocation of the tibia relative to the femur, as stated in Rouquette et al. [9] systematic review [9]. Nevertheless, regardless of dislocation direction, we highlight the rareness of this complication, being present in <1% of post-TKA patients [1]. Despite the absence of definitive data regarding the dislocation mechanism, it is thought that it often occurs due to traumatic events, low-energy falls, or knee hyperflexion [9]. Moreover, several risk factors are thought to play a role on TKA dislocation, namely obesity, varus or valgus knee deformity, peripheral or central neurological pathology, and psychiatric pathology [9,10]. Other predictive factors have also been described, such as an overlap injury to the knee collateral ligaments, destabilization of the extensor apparatus, excessive release of soft tissues, or poor placement of prosthetic components [10].
In the reported case, the patient had excess weight and varus knee deformity as top predictors for this complication. The patient was submitted to a tailored and intensive rehabilitation program, prescribed with clear objectives, adapted to the patient’s characteristics and to the time after surgery and adapted to the clinical and functional evolution. Therefore, we believe the program was not a risk factor for this complication. Besides, we could not find a single case of TKA dislocation related to the fragilities of the rehabilitation program. Once the dislocation occurred during the night, it would be essential to supervise and assist in the first moments of mobility in bed. After the surgical correction, we kept the initial rehabilitation plan established. However, the nursing team added greater patient proximity, caution, and monitoring in bed mobility. Nonetheless, the mechanism of injury needed to be accurately depicted. The remaining factors are intrinsic and unmodifiable in the short-term (obesity and varus knee deformity).
Conclusion
Total Knee Arthroplasty (TKA) dislocation is an uncommon complication. Nevertheless, it is an impactful diagnosis, both in clinical and functional spheres, requiring special attention from physicians. PM&R is of utmost importance in the clinical approach to these patients, assuring a proper rehabilitation program and awareness of TKA complications, such as posterior dislocation. These physicians should be aware of the risk and predictive factors for these events, as well as the diagnosis routine and proper approach, assuring the maximum restoration of functionality.
References
- Scuderi GR (2012) Complications after total knee arthroplasty: How to manage patients with osteolysis. Instr Course Lect 93(22): 2127-2135.
- Vasconcelos JW, Leite LM, Sousa JCA, Sousa JOM, Santos MFS (2013) Mid-term evaluation of total knee arthroplasty without patellar replacement. Brazilian Journal of Orthopedics 48(3): 251-256.
- Porter M, Armstrong R, Howard P, Porteous M, Wilkinson JM (2019) Orthopaedic registries-The UK view (National Joint Registry): Impact on practice. EFORT Open Rev 4(6): 377-390.
- Souza GGA, Ramalho RSC, Pires ARS, Barretto JM, Chaves RSM, et al. (2020) Higher risk of complications after total knee arthroplasty in octogenarians. Acta Ortop Bras 28(4): 177-181.
- Wright RC, Crouch A, Yacoubian SV, Ravan RB, Falkinstein Y, et al. (2011) Nontraumatic, spontaneous dislocation of polyethylene tibial insert 1 year after TKA. Orthopedics 34(12): 933-935.
- Villanueva M, Ríos-Luna A, Pereiro J, Fahandez-Saddi H, Pérez-Caballer A (2010) Dislocation following total knee arthroplasty: A report of six cases. Indian J Orthop 44(4): 438-443.
- Conti A, Camarda L, Mannino S, Milici L, D’Arienzo M (2015) Anterior dislocation in a total knee arthroplasty: A case report and literature review. J Orthop 12(1): 130-132.
- Arnout N, Vandenneucker H, Bellemans J (2011) Posterior dislocation in total knee replacement: A price for deep flexion? Knee Surgery, Sport Traumatol Arthrosc 19(6): 911-913.
- Rouquette L, Erivan R, Pereira B, Boisgard S, Descamps S, et al. (2019) Tibiofemoral dislocation after primary total knee arthroplasty: A systematic review. International Orthopaedics 43(7): 1599-1609.
- Erceg M, Maričević A (2000) Recurrent posterior dislocation following primary posterior-stabilized total knee arthroplasty. Croat Med J 41(2): 207-209.
© 2022 André Varandas-Borges. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






