- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
Agrarian Population’s Occupational Health Risks and After Effects
Ajay Pal Natt*, Ramanjit Kaur, Amandeep Singh and Paramvir Singh
Department of Sports Science, India
*Corresponding author: Ajay Pal Natt, Department of Sports Science, India
Submission: March 26, 2021; Published: April 09, 2021

ISSN 2637-7934 Volume3 Issue2
Abstract
Agriculture is the prime occupation in India and many other developing countries. In the modern era, agricultural workers are confronted with many hazards include chemical hazards, biological hazards, ergonomic hazards, psychosocial hazards and physical hazards. Hence, the agriculture sector is associated with a variety of occupational injuries and illnesses. Compared with some other industries, agricultural workers are relatively facing higher risk of accidents than other workers. This sector of activity being most unorganized, suffer from certain specific health hazards due to extensive use of fertilizers, insecticides and pesticides and mechanization [1]. The method used in this study was a review and analysis of past data. The study classified the number and rate of occupational fatalities for workers in the agriculture sector. This paper presents the results of a literature review undertaken to determine [2] the health risks faced by the agrarian population worldwide and their aftereffects. It was concluded that the negligence toward health hazards of the farmers is costing their quality of life, which they are totally unaware, and it is the need of an hour to give proper training to farmers from time to time so that they are properly educated about the components of their work and that would further prevent the precarious effects on their health in future.
Keywords: Farmers; Agriculture; Occupational health hazards; Pesticide exposure
Introduction
India is primarily an agrarian economy as farming is one of the most important occupations in the country [3]. Agriculture is the basic strength of Indian economy and maximum of population depends for their livelihood on agriculture only [4]. In the context of occupational safety and health, the term ‘agriculture’ is generally used in a broad sense including all activities directly related to cultivating, growing, harvesting and primary processing of agricultural products, animal and livestock breeding including aquaculture, and agroforestry. Agricultural work is dangerous; workers in this industry have among the highest rates of fatalities (BLS, 2014 and Liabman et al. 2013) [5]. It is one of the most precarious sector in regard to health worldwide, hence possesses various attributes that causes risk for health. These are:
A. Exposure to the weather.
B. Close contact with animals and plants.
C. Extensive use of chemical and biological products.
D. Difficult working postures and lengthy hours .
E. Use of hazardous agricultural tools and machinery [6].
F. The hazardous working conditions in agriculture can increase the risk of occupational
accidents adapted from (Forastieri [7]), include open air work, seasonal work, a variety
of tasks, variation in working postures, contact with animals and plants, contact with
chemicals, utilization of machines, isolated work, limited provision of emergency services,
home embedded in the farm, etc.
G. Machineries used in in agriculture, such as tractors and harvesters have the highest
frequency and fatality rates of injury (Yiha and Kumie 2010).
H. On the other hand, exposure to pesticides and other agrochemicals can cause
poisoning and in certain cases, lead to work-related cancer and death.
I. Besides, there are also other hazards caused by multiple
contacts with poisonous and wild animals, plants and biological
agents which may give raise to allergies, respiratory disorders
stress and psychological disorders [8].
Occupational risk factors include increased morbidity and mortality from accidents, zoonoses, climatic exposure, respiratory disease caused by dust and organic matter, chemical toxicity and ergonomic hazards [9]. The commercialization of agriculture in Punjab through the Green Revolution led to the effects, which were far‐reaching and irreversible. The Green Revolution replaced indigenous agriculture with modern agriculture that led to the use of high yielding seed varieties leading to a loss of indigenous varieties of various crops; the contamination of soils and water systems from the use of pesticides, chemical fertilizers, modern irrigation systems and dependency on modern machinery and technology [10].
Methodology
This study aimed at compiling all long-term reports on the risk filled working conditions in agriculture and the occupational health hazards inculcated in them available through different literature databases. In that impact, we performed a search on the online web of literature database using keywords (agriculture), (occupational health hazards), (pesticide exposure) and (farmers) which resulted in plethora of publications. Some experimental and survey-based literature were selected that included all the issues faced by farmers worldwide. The review covered 15 articles on occupational health hazards, use of pesticides and their health impact on farmers all over the world.
Farmworker health factsheets [11]
Pesticide exposure:
A. Today, farmworkers are exposed to “nonpersistent”
pesticides which are metabolized by the body within days. They
may enter the body through ingestion and inhalation, but they
are primarily absorbed through the skin.
B. During the daily work, farmworkers are often exposed to
pesticides, which include substances that prevent, destroy or
repel pests. Because some pests have systems similar to the
human system, some pesticides also can harm or kill humans.
The term pesticide also encompasses herbicides, fungicides,
and various other substances used to control pests.
C. Farmworkers frequently encounter pesticides through
direct contact with the chemicals, contact with pesticide
residue on treated crops or equipment, and drift of pesticides
into untreated areas.10© NCFH, March 2013
D. Several studies also prove that entire families are at risk
to pesticide exposure because of drift from nearby areas, not
providing enough hand-washing or bathroom facilities, and
brining home clothes that have been contaminated.
E. The Pesticide Safety Education Program out of Cornell
University states that mild symptoms of poisoning include
headache, fatigue, dizziness, nervousness, perspiration, loss of appetite, thirst, eye irritation and irritation of the nose and
throat. Severe poisoning symptoms include fever, intense thirst,
vomiting, muscle twitches, convulsions, inability to breathe and
unconsciousness.
F. The Florida Department of Health webpage lists several
chronic effects from long-term exposure to pesticides:
G. Birth defects
H. Cancers
I. Blood disorders
J. Neurological problems
K. Reproductive effects
L. Exposure to large doses of a pesticide can lead to severe
effects such as loss of consciousness, coma and even death.
M. Pesticide Safety regulations that exist include:
1. The Worker Protection Standard, which states that field
workers must be trained on pesticide use, and
2. The Occupation Safety and Health Act, which requires
employers with 11 or more employees to provide drinking,
toilet and washing facilities for farmworkers while they work in
the fields.
N. A study conducted in eastern North Carolina polled 300
farmworkers regarding pesticide safety and training. They
reported the following:
1. 75.3% had water available for hand-washing, but only
44.3% were provided soap,
2. 51.3% were told when it was safe to enter fields after
applying,
3. 51% were told when pesticides were applied,
4. 34.8% reported being provided pesticide safety
instruction by a supervisor,
5. 28% per cent worked in areas adjacent to fields where
pesticides were being applied,
6. 25.2% were asked to enter fields before it was safe to do
so,
7. 16% worked in fields while pesticides were being applied,
and
8. 14.8% were provided with pesticide safety equipment.
O. Another pesticide danger for farmworkers is the limited
information they are provided about the pesticides they are
being exposed to. They are not told what types of pesticides
are being used at any given time, they have little control over
exposure, and they are often live-in grower-provided housing
and do not know the severity of exposure in these dwellings.
P. One other challenge is that growers rarely speak the
same languages as workers. Growers often do not recognize
or understand how linguistic, cultural and power differences
create barriers for farmworker pesticide safety.
Hazardous tools and machinery
In this modern era, agriculture sector had evolved to the level
that farmers use heavy machinery and dangerous tools in fields
rather than working manually. Hence, where these equipment
and machinery had assisted the farmers in their work, they had
also affected them adversely. Physical activity has reduced as
majorly work is done by machines and tools, there are risks of mis
happenings and accidents while using such hazardous equipment
which could even prove to be fatal [12-14].
According to the Bureau of Labour Statistic 2011 data, the
following was reported of fatalities within the industry of crop
production:
A. 132 fatal incidents involving transportation, which
includes injuries resulting from being struck by a vehicle, and
B. 45 fatal incidents from contact with objects and
equipment.
C. As for non-fatal injuries in agriculture, machinery was the
leading source, with 99,402 reported injuries. In 2011 there
were:
D. 41,777 injuries from hand tools, and
E. 24,590 injuries from tractors.
Infectious diseases
Infectious diseases among the farmworker population are caused by poor sanitation and crowded conditions at work and housing sites, including inadequate washing and drinking water [15].
A. A study conducted in 2010 in assessed the water quality
of 181 farmworker camps. Thirty-four (34) per cent of samples
were found unsafe for human consumption.
B. A 2006 study of farmworkers in North Carolina found that
46 per cent of farmworkers lived in very crowded and unsanitary
conditions. Conditions such as these increase farmworkers’
exposure to environmental toxins and communicable diseases
Although recent figures do not exist for tuberculosis rates, one
study determined that 44 per cent of migrants had a positive PPD
(tuberculin) skin test.
Musculoskeletal injuries
Because farm labour consists of constant bending, twisting, carrying heavy items, and repetitive motions during long work hours, farmworkers often experience musculoskeletal injuries. Furthermore, workers are often paid piece-rate, which provides an incentive to work at high speed and to skip recommended breaks. One study that interviewed 150 farmworkers reported that musculoskeletal injuries were very common as a result of the nature of farm work [16-18]. The following is a breakdown of the frequency of injuries that resulted:
A. Backache occurred in 46 incidents © NCFH, March 2013.
B. Shoulder pain occurred in11 incidents.
C. Sprains occurred in 9 incidents.
D. Fractures occurred in 5 incidents and
E. Pain/numbness of the hand occurred in 4 incidents.
A 2008 report recorded that about 20 per cent of farmworkers
suffer from musculoskeletal injuries.
Respiratory illnesses
Because agricultural work takes place in rural areas, farmworkers are exposed to organic and mineral dusts, animal and plant dusts, toxic gases, mould and other respiratory irritants. All of these have been associated with respiratory illnesses, such as asthma and chronic bronchitis. Another chronic respiratory illness of concern is Farmer’s Lung, a non-infectious allergic disease caused by inhaling mould spores. These mould spores accumulate and settle in the lower lungs, which interferes with their ability to exchange gas. As a last defence, the body develops an allergic reaction that causes cold or pneumonia symptoms. Farmworkers have a significantly higher death rate for a number of respiratory conditions, including hypersensitivity pneumonitis (proportionate mortality more than 10 times higher than expected), asthma, bronchitis, histoplasmosis, tuberculosis, pneumonia, and influenza [19-22].
Farmworkers who work in the following tasks are at increased risk of respiratory illnesses:
A. Dusty fields and buildings.
B. Handling of hay.
C. Feeding or working with feedstuffs.
D. Working in corn silage.
E. Cleaning silos or grain bins.
F. Working around bird droppings or dust from animal hair,
fur, or feathers.
G. Working around fishmeal and
H. Applying agricultural chemicals such as fertilizers and
pesticides.
Skin disorders
Farmworkers are exposed to many occupational and environmental risk factors that result in skin disease: weather, mechanical devices, chemicals, plants, organic and inorganic dust and fungi. A study conducted in North Carolina which interviewed 304 Latino farmworkers on skin conditions concluded that although skin conditions were observed, farmworkers turn to self-treatment as opposed to health care visits. The study reported that 63 percent used non-prescription preparations, 9 percent used prescription products and 6 percent used home remedies to cure skin ailments.
Another study conducted in North Carolina recorded the most commonly occurring skin problems and symptoms. The following, along with their frequency, was reported:
A. Skin fungus had a rate of 58.6 percent.
B. Sunburn had a rate of 58.6 percent.
C. Bumps, pimples, or acne had a rate of 48.4 percent.
D. Calluses had a rate of48.4 percent.
E. Itching had a rate of 46.1 percent.
F. Rash had a rate of 42.8 percent.
Eye injuries
Agricultural work, by its nature, poses specific risks for eye injury. Some of these include different chemicals (pesticides, growth enhancers and fertilizers, tools and machinery. Likewise, environmental factors also pose a risk due to exposure to hazards such as ultraviolet light, airborne soil, particulates, pollen, humidity and plant components. These environmental objects are known to cause infections, allergic reactions, eye irritations, and corneal and other eye trauma. Chronic irritation and sun can cause cataracts, a clouding of the eye lens, and pterygium, a growth that obstructs the cornea. Agricultural workers experience eye injuries and illness at a rate of 8.7 per 10,000 workers. This is more than two times higher than the rate of 3.8 per 10,000 for general workers in the U.S.
Heat and sun exposure
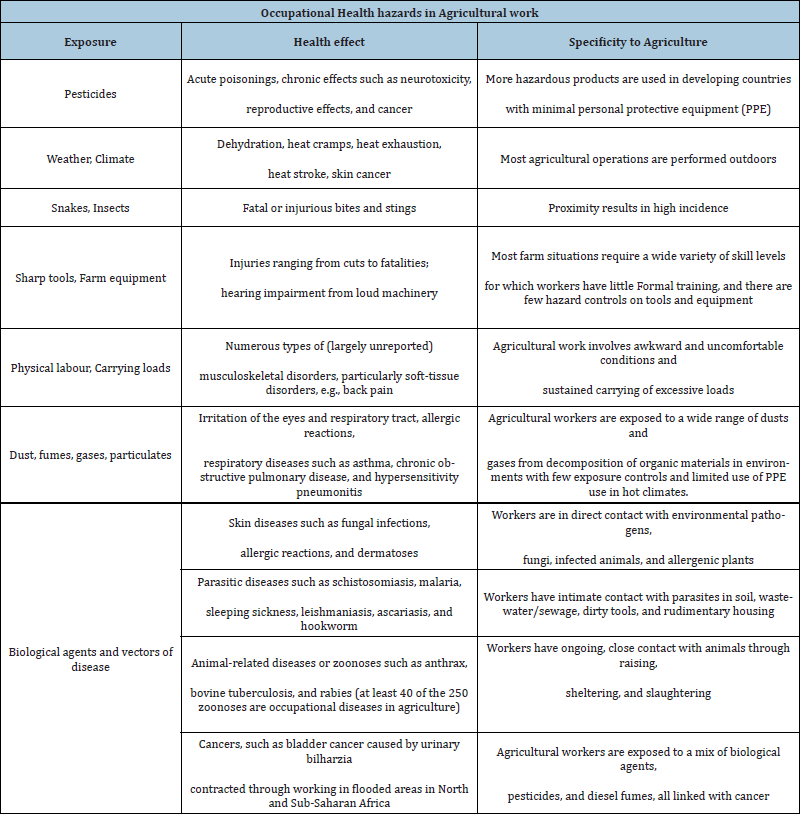
Farmworkers are at increased risk for heat injury and illness due to the nature of farm work: they work outdoors in direct sunlight, humidity levels are often higher in the fields, they generate large amounts of body heat, and they often use heavy work clothing and equipment. Heat stress occurs when body heat builds up from both external and internal sources. This condition can lead to dehydration, electrolyte imbalance, neurological impairment, multi-organ failure, and death. According to the Centre for Disease Control and Prevention, the signs and symptoms of heat exhaustion include heavy sweating, cold/pale/clammy skin, a fast, weak pulse, nausea and vomiting and fainting. Meanwhile signs of stroke include a high body temperature above 103 degrees F, hot, red, dry or moist skin, rapid and strong pulse and sometimes unconsciousness. Heat stroke is considered a medical emergency. A study published in 2008 found that in the previous 15-year period, 423 workers in agriculture and non-agricultural industries died from heat exposure. Results indicated that 67 per cent of those fatalities were crop workers employed in the crop production or support activities for crop production sectors. In a study conducted with 300 farmworkers in North Carolina, 94 per cent of respondents reported that they work in extreme heat, and 40 per cent reported having had symptoms of heat illness. An added danger for farmworkers is that pesticides are absorbed through hot, sweaty skin more quickly than through cool skin (Table 1).
Table 1:
Discussion
The present study is the predictive call for the farmers worldwide
about the crisis that they are going to face in the upcoming years
especially by the future generations due to the occupational health
hazards and excessive use of chemical pesticides. Data from the
studies appear to suggest a considerable burden of morbidity and
a high prevalence of risk factors for chronic illness and disability
among farm workers in the region. Alcohol abuse, head injury
and chronic under-nutrition, animal attacks stand out as the most
striking of the findings, although a wide range of adverse health
states were identified [8]. The highest frequency and fatality rates
of injury or mortality caused by farm machinery or non-chemical
occupational accidents have still been rising in the industrialized
and developing countries (ILO, 2002). There are many risks to
health present in agriculture sector. Statistics from SOCSO shows
2,997 reported cases of occupational diseases in 2014 in Malaysia.
The main cause agents of occupational disease are physical
agents with 1,277 cases (43%) and occupational Musculo-skeletal
disorders with 675 cases (23%). Disability due to musculoskeletal
injuries and diseases incurred during their working years affect the
workforce in agriculture sector more frequently and more severely
than any other safety and health problem during the rest of their
working years [4].
Another aspect is increased incidence of work-related skin
neoplasia in agricultural workers as well as several conditions
that affect their ability to work, specifically MSD, asthma, allergic
alveolitis and infections specific to farming. In contrast, there is a
reduced incidence of work-related mental ill-health. Last but not the
least , the use of pesticides inappropriately, without the knowledge
of the procedure, the amount and the precautions related to the
usage, had lead the agrarian population towards the health hazards
that prove to be fatal to them as well as to the environment on the
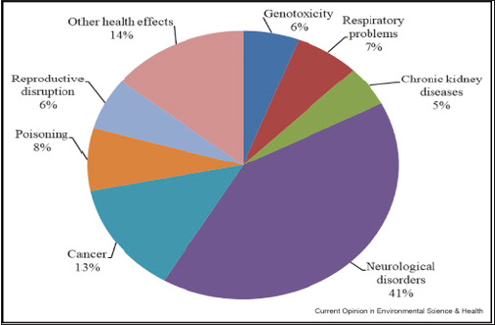
whole (Figure 1).
Figure 1:
Conclusion
Farming is done in every part of the world, and farmers work tirelessly irrespective of time and weather which further affects their health hazardously. They use more and more pesticides, heavy machinery today to do farming, due to which their body is affected and at the same time it also affects the environment like air, water, land. On one hand it becomes very important for the farmers to be aware of the occupational health hazards they encounter during their work and how to manage them and get rid of them effectively. They need to know about how to handle pesticides with their minimal adverse effects on them and use of the safety equipment to protect themselves. On the other hand, it becomes the responsibility of the governing bodies to analyze the causes and effects of agricultural hazards and the steps to be taken to counter them. By reviewing literature can be concluded that the farmers are not conscious of the toll that their occupation is taking on their health in the current scenario as they do not follow appropriate procedures and safety precautions. It is need of an hour to give proper training to farmers from time to time so that they are properly educated about the components of their work and that would further prevent the precarious effects on their health in future. Farmers needs to be encouraged to reduce, if not eliminate, the use of pesticides, with the introduction of incentives to help them shift from synthetic pesticides to bio-pesticides and organic farming and the major part of this change could be brought by the governments by making laws and rules that safeguard the rights and interests of the farmers to the best of their capacity, to take measures to educate the farmers so that safety precautions could be undertaken in any work that would prove hazardous or even fatal.
References
- Sangamithra A, Arun KP (2017) A study on occupation related health problems among agriculture workers in Theni district. Shan lax International Journal of Arts, Science and Humanities 4(4).
- Surabhi SRA (2010) Ergonomic intervention for preventing musculoskeletal disorders among farm women. Journal of Agricultural Sciences 1(2): 61-71.
- Gupta, Tarique (2013) Prevalence of musculoskeletal disorders in farmers of Kanpur-rural. India J Community Med Health Educ 3: 7.
- Vyas, Rekha (2006) Occupational health hazards among agricultural workers and developing educational aids for creating awareness, Maharana Pratap university of agriculture and technology, Udaipur.
- Pragya O, Abha S (2018) Assessment of occupational health hazards among farm workers involved in agricultural activities. Journal of Pharmacognosy and Phytochemistry SP1: 1369-1372.
- Donald C (2006) Understanding the links between agriculture and health: Occupational health hazards of agriculture. Focus 13: 8-16.
- Forastieri V (2001) Challenges in providing occupational safety and health services to workers in agriculture. Afr Newslett on Occup Health and Safety 11(2): 33-38.
- Auyonga HN (2016) A review of occupational safety and health risks in agriculture sector in Malaysia. International Conference on Agricultural And Food Engineering pp. 23-25.
- London L, Thompson ML, Myers JE (1998) Health status among farm workers in the western cape-collateral evidence from a study of occupational hazards. South African Medical Journal 88(9): 1096-1101.
- Reetinder KA, Sinhaa AK (2011) Globalization and health: A case study of Punjab. Journal of Studies And Research In Human Geography 5(1): 35‐42.
- Farmworker occupational health and safety farmworker health factsheets, National Center For Farmworker Health.
- Stocks SJ, Turner S, Carder M, Hussey L, Agius RM (2010) Medically reported work-related ill-health in the UK agricultural sector. Occupational Medicine 60(5):340-347.
- Shetty PK (2004) Socio‐ecological implications of pesticide use in India. Economic and Political Weekly 39(49): 5261‐5267.
- Roul C (2001) Bitter to better harvest. Northern Book Centre, New Delhi, India.
- Peter K (2012) Physical activity, health benefits, and mortality risk. ISRN Cardiology 2012(14): 718789.
- Myers J, Prakash M, Froelicher V, Partington S, Edwin A, et al. (2002) Exercise capacity and mortality among men referred for exercise testing. The New England Journal of Medicine 346(11): 793-801.
- Hamid AA, Ahamad WMZW (2014) Country report: Malaysia, 1st Asia Pacific Network for Testing Agricultural Machinery (ANTAM) Meeting. China.
- Namee R, Carder M, Chen Y, Agius R (2008) Measurement of trends in incidence of work-related skin and respiratory diseases, UK 1996-2005. Occup Environ Med 65(12): 808-814.
- Walker BK, Palmer KT (2002) Musculoskeletal disorders in farmers and farm workers. Occup Med 52(8): 441-450.
- Fraser K, Smith KB, Judd JS (2005) Farming and mental health problems and mental illness. Int J Soc Psychiatry 51(4): 340-349.
- Vijay KM(2014) An epidemiological study of mechanical health hazards amongst agricultural workers in rural India. International Journal of Occupational Safety and Health 4(2): 19-23.
- Andersson HT, Treich N (2014) Pesticides and health: A review of evidence on health effects , valuation of risks , and benefit-cost analysis. Adv Health Econ Health Serv Res 24: 203-295.
© 2021 Ajay Pal Natt. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






