- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
The Physiotherapeutic Management of Post Stroke Shoulder Pain: A Systematic Review
Anoeska Gajapersad1* and Ameerani Jarbandhan2* and Robbert Bipat3*
1Department of Physiotherapy, Academic Hospital Paramaribo, Suriname
2Department of Anatomy, Faculty of Medical Sciences, Anton de Kom University of Suriname
3Department of Physiology, Faculty of Medical Sciences, Anton de Kom University of Suriname
*Corresponding author: Robbert Bipat,Department of Physiology, Faculty of Medical Sciences, Anton de Kom University of Suriname email: robbert.bipat@uvs.edu
Submission: October 27, 2020; Published: December 01, 2020
ISSN 2637-7934 Volume3 Issue2
Abstract
Purpose: No single effective physiotherapeutic management has been suggested for Post Stroke Shoulder Pain (PSSP), the most frequent occurring type of pain after stroke. The aim of this study is to summarize and evaluate the effect of electrotherapy, training, exercise, thermotherapy and taping on PSSP originating from capsulitis, (sub)luxation and contracture.
Materials and methods: Two independent investigators systematically searched relevant databases for Randomized Controlled Trials (RCTs). The methodological quality was evaluated by the PEDro scale. Inclusion criteria were (1) patients from any age, sex or type of stroke; (2) onset of hemiparetic pain after stroke; (3) RCT’s evaluating the effect of physiotherapeutic modalities on PSSP with a pain measuring scale.
Results: Nineteen studies out of the identified 266 met de inclusion criteria. They represented 792 participants. Ten studies with a PEDro quality from poor to high reported reduction of PSSP associated with shoulder girdle weakness, capsulitis and subluxation, whereas nine studies with fair to high quality reported no reduction after conventional therapy, electrotherapy, sling and taping or a combination of these.
Conclusion: Some studies reveal evidence for adequate management of PSSP with physiotherapeutic modalities. However, additional research with adequate study designs is necessary to confirm the effect of these modalities.
Keywords: Stroke; Pain; Shoulder; Physiotherapy; Hemiplegic
Introduction
Stroke is an important cause of disability and, therefore, a major public health problem [1]. The disorder leads to a number of consequences of which pain is a frequently observed symptom (32% - 42%) [2,3]. Post stroke pain is common but often neglected, apparently due to prioritization of motor function recovery in physiotherapeutic intervention plans [2]. Post Stroke Shoulder Pain (PSSP) is a common complication after stroke and has a major impact on the quality of life and daily life after stroke [4,5]. The prevalence varies from 21% to 64% [4,6].
Physiotherapeutic management of patients with PSSP comprises of several modalities that treat post stroke pain. These may include exercise, electrotherapy and cryotherapy [3]. However, the effectiveness of these modalities in post stroke patients has not been adequately evaluated. Investigators reviewed the influence of modalities on PSSP, like the effect of acupuncture [7] or electrical stimulation on PSSP [8,9]. Reviews regarding the effect of a multidisciplinary approach on hemiplegic shoulder pain management [10], the physiotherapeutic effect on post stroke patients including those with PSSP [11] and management of hemiplegic shoulder pain [12], all provided relevant information. Yet, none of the studies included the complete spectrum of available physiotherapeutic modalities as defined by the World Confederation for Physical Therapy guidelines [10]. Therefore, this study aimed to summarize and evaluate the effects of various physiotherapeutic modalities for PSSP caused by capsulitis, (sub)luxation and contracture in all stroke patients as reported in the past decade. Moreover, we will report on the usage of any form of evaluation of cognitive and somatosensory dysfunction as it may impede proper assessment of pain in stroke survivors [10,13].
Materials and Method
Databases and search strategies
A systematic literature search was conducted in PubMed (MEDLINE) (Sept 2008-Sept 2018), Excerpta Medica database (EMBASE) (Jan 2008-Sept 2018), Web of Science (Aug 1997- Sept 2018) and Physiotherapy Evidence Database (PEDro) (Jan 1994- Jan 2017) and included the following string: (stroke OR CVA) AND (ache OR pain) AND (shoulder OR glenohumeral) AND (electrotherapy OR thermotherapy OR exercise OR training OR treatment OR taping) AND (subluxation OR contracture OR capsulitis) AND (physical therapy OR physiotherapy) AND (hemiparetic OR hemiplegic). After the selection of potential studies from these four databases, the investigators also screened the reference lists of the relevant studies for eligibility.
Study selection
Studies conducted between 2008 and 2018, published in English and designed as a Randomized Controlled Trial (RCT) that reported the effect of a physical therapy modality as treatment for shoulder pain among patients with stroke using a pain measuring scale were eligible for inclusion. Furthermore, studies with patients of any age, sex, type and phase of stroke as well as studies concerning the onset of hemiparetic shoulder pain after stroke were included. Studies regarding shoulder deficiencies originating from neurological disorders other than stroke were excluded. Since our study obtained data from literature already published, no approval was required from the institutional review board and patient consent was not necessary.
Data extraction
Two independent researchers systematically reviewed the selected studies. They screened the records of the databases on title and abstracts according to the eligibility criteria. Once the selected studies met the eligible criteria, the researchers subsequently read the full-text of those publications. Finally, they screened the reference lists of these publications for studies that met the inclusion criteria. With the aid of the PEDro scale eligible studies were assessed for their methodological quality [14] based on the Delphi list.
The total score for this assessment tool ranged from 0 to 10 Criterion 1 deals with external validity opposed to the internal or statistical validity of the trial. It has been included in the PEDro scale to complete all items as represented in the Delphi list. For this reason, the PEDro score does not include criterion 1 for calculation. Studies met the classification of high methodological quality with a score between 6-10; fair quality with a score between 4 and 5 and poor quality with a score less than four. Although, the Cochrane Collaboration prefers the term “bias” above “quality” [15], the latter was still chosen in order to compare the obtained results with those found in previous studies. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement resulted in an outline of possible inclusion in this review [16]. The investigators submitted the protocol at the International Prospective Register of Systematic Reviews (PROSPERO) on the 26th of February 2019 (CRD42019126744).
Result
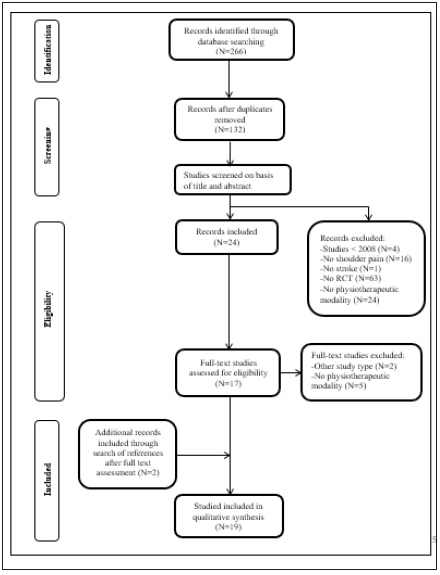
Two hundred and sixty-six studies were initially screened (EMBASE (N=55); PubMed (N=59); PEDro (N=52); and Web of Science (N=100)) (Figure 1). After adjusting for duplicates, a total of 132 studies remained. On the basis of title and abstract, another 108 studies were excluded for the following reasons: (1) studies older than 2008; (2) outcome measurements other than pain; (3) patients without the diagnosis of stroke; (4) study design other than an RCT or studies without a physiotherapeutic modality (Figure 1).
Out of the remaining 24 studies, 17 studies met the inclusion criteria after examination of the full text. Furthermore, references of these 17 studies led to the inclusion of 2 additional studies. Therefore, the present systematic review included a total of 19 studies (Figure 1).
Figure 1: Selection of the studies included in the systematic review.
Study Characteristics
Table 1 summarizes the methodological quality of the studies according to the PEDro scale. The PEDro score for twelve studies [17-27] ranged between 6- 8. One study [28] did not specify the eligibility criteria and the randomization of the allocated subjects None of the studies reported blinding of the therapist to the therapy itself. Five studies [19-21,25,27] reported blinding of all subjects. And only six studies [17,19,22-24,29] reported “intention to treat” for at least one key outcome measure.
Table 1: Methodological quality of the included studies.
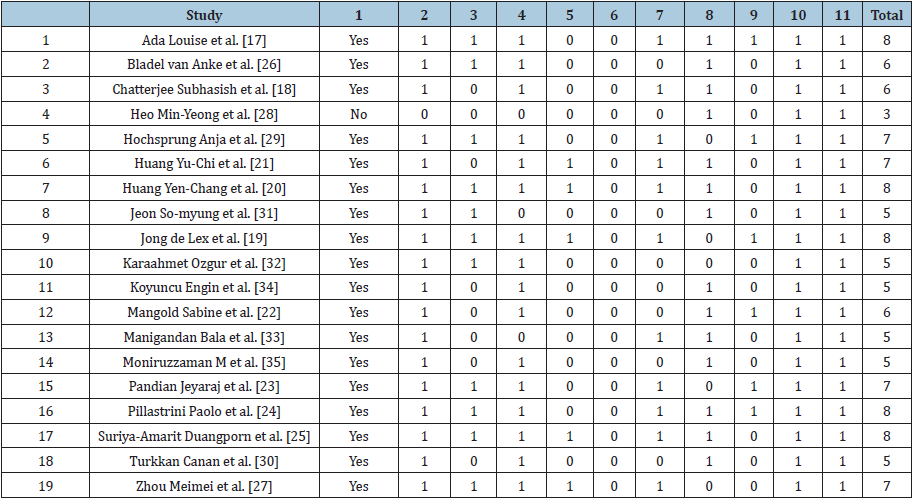
Table 2 summarizes the number of participants, intervention, outcomes and results of each study. One study [30] included only chronic stroke patients, whereas ten studies [17-19,21-23,28,31- 33] included both acute and subacute patients after stroke. The remaining eight studies [20,24-27,29,34,35] did not specify the time after stroke of their study population. Eight studies [18,26,28,30,31-34] reported shoulder subluxation, ten studies [17,19-25,27,29] reported shoulder girdle muscle weakness and one study [35] reported capsulitis as cause of PSSP
Table 2: Overview of included studies.
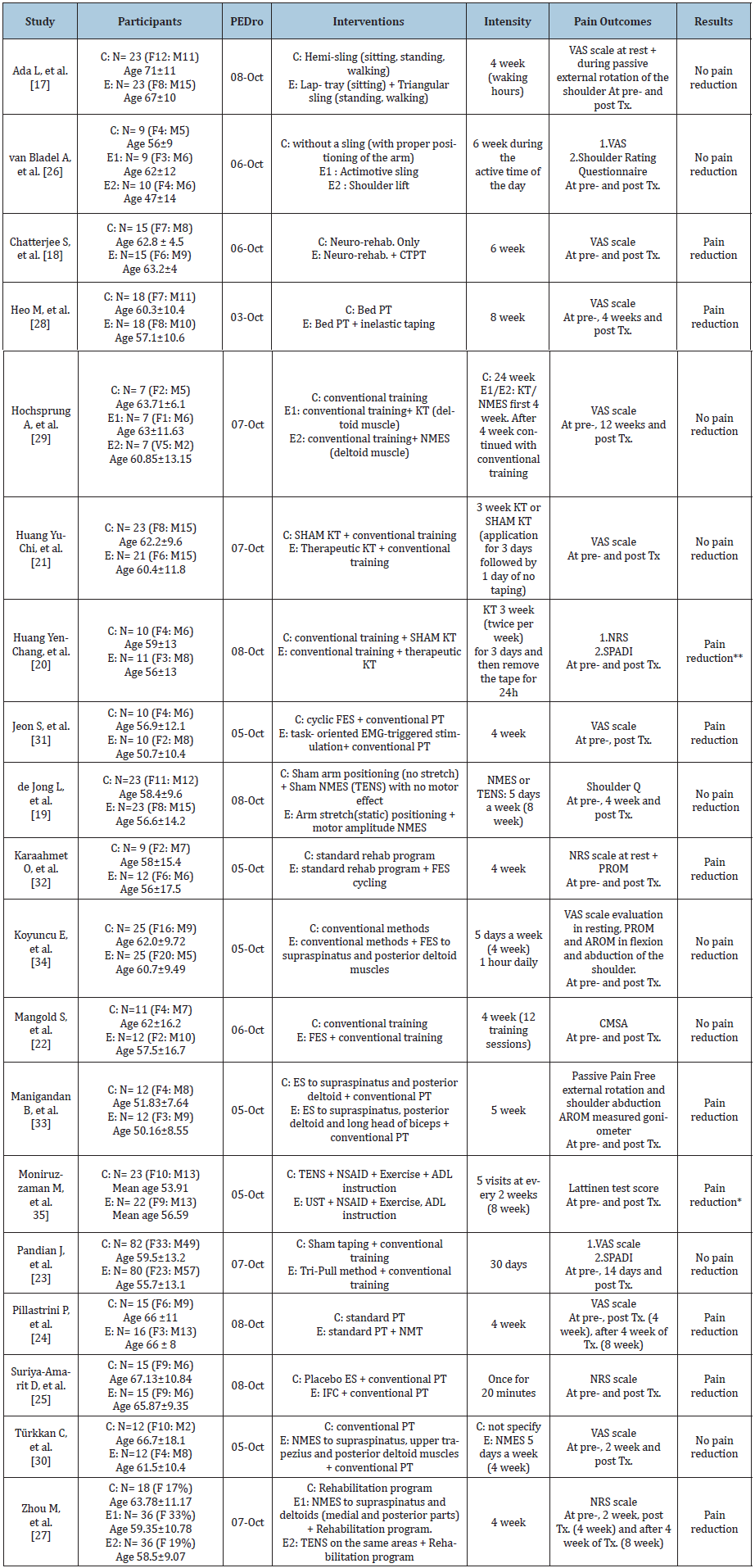
ADL=Activities of Daily Living; AROM=Active Range of Motion; C=Control; CMSA=Chedoke McMaster Stroke Assessment; CTPT=California Tri-Pull Taping; E=Experimental; EMG=Electromyography; ES=Electrical Stimulation; F=Female; FES=- Functional Electrical Stimulation; IFC=Interferential Current Stimulation; KT=Kinesio Taping; M=Male; NMES=Neuro- Muscular Electrical Stimulation; NMT=NeuroMuscular Taping; NRS=Numeric Rating Scale; NSAID=Non-Steroidal Anti Inflammatory Drug; PROM=Passive Range of Motion; PT=Physiotherapy; SPADI=Shoulder Pain and Disability Index; TENS= Transcutaneous Electrical Nerve Stimulation; Tx=Therapy; UST=Ultrasonic Therapy; VAS=Visual Analogue Scale. *TENS and UST both are effective, but TENS may be safer and superior to Age is mean (years) with SD. ** There is greater reduction in SPADI, pain and improvement in shoulder flexion, external and internal rotation after 3 weeks of therapeutic KT intervention.
The scales applied to assess the degree of pain were not consistent in the studies and included:
1. The Visual Analog Scale (VAS) [35] score [17,18,21,24,28- 31,34];
2. The Numeric Rating Scale (NRS) [35] score [25,27,32];
3. The Lattinen [35] score [35];
4. The Shoulder Q [35] Questionnaire [19];
5. The pain-free range of Passive Lateral Rotation (PLRL) [33];
6. The Chedoke McMaster Stroke Assessment [35] (CMSA) [22];
7. The Shoulder Pain and Disability Index [35] (SPADI) [35] and
8. The Shoulder Rating [35] Questionnaire [36].
The Shoulder Rating Questionnaire and the VAS were paired in two studies [23,26]. One study used the SPADI in combination with the VAS [35] and one study used the SPADI together with the NRS score [20]. The VAS score was used in eleven studies. In nine studies [17,19-23,26,29,30,34,35] no significance of pain reduction was reported between the control and intervention groups.
In total 792 participants were studied. Sample sizes in each study ranged from 20 to a maximum of 162. Thirteen studies [17,20-22,24,26,28-33,35] reported a small sample size and only three studies [19,23,27] reported a power-based calculated sample size. The mean age in the studies varied from 47(±14) to 71(±11) years. All the studies included men and women of which 39% were women.
Four studies [28,34,36,37], measured cognitive status with the Mini Mental State Examination (MMSE) whereas 8 [22,23,25-27,29- 31] ignored to mention a specific scale. Five studies evaluated the ability to communicate and cooperate [32]. The remaining two [32] did not evaluate cognition. Ten studies [19,22,25,27,30- 35] focused on various forms of electrotherapy and eight studies [17,18,20,21,23,24,26,28,29] on diverse forms of taping and sling. Furthermore, one study [29] had a combination of electrotherapy and taping. All 19 studies combined the modality with a form of rehabilitation program or conventional therapy mainly consisting of one type of exercise and training. None of the studies reported the use of thermotherapy or a specific type of exercise intensity or frequency.
Significant difference of pain reduction
Electrotherapy: Six studies [25,27,31-33] applied various forms of electrotherapy with a significant reduction of pain. Varieties of electrotherapy were:
1. Electro Stimulation (ES) [33];
2. Functional Electrical Stimulation (FES) [32];
3. Electromyography (EMG) triggered ES versus FES [31];
4. NeuroMuscular Electrical Stimulation (NMES) versus Transcutaneous Nerve Stimulation (TENS) [27];
5. TENS versus Ultrasonic therapy [27] and
6. Interferential Current Stimulation (IFC) versus ES [25].
Of these only one single study [27] presented a power-based calculated desired sample size of 90 whereas others reported sample sizes that varied between 20 and 45 participants. All of these studies scored between 5 and 8 on the PEDro scale.
Taping: Four studies [18,24,28] of taping found significant difference of pain reduction compared to other interventions. They utilized three various taping methods:
1. California Tri-Pull Taping (CTPT) [18],
2. NeuroMuscular Taping (NMT) [24],
3. Kinesio Taping (KT) [18] and
4. Inelastic Taping [28].
These studies scored between 3 and 8 on the PEDro scale and had a random sample size with unknown power.
No significant difference of pain reduction
Electrotherapy: Four [19,22,30,34,35] studies focused on modalities with electrotherapy, and showed no reduction of PSSP. These studies utilized:
1. Functional Electrical Stimulation (FES) [22,34] and
2. Electrical Stimulation (ES) [19,30].
The PEDro score of the studies was between 5 and 8. Only 1 study [19] presented a calculated sample size, whereas the other studies contained a random sample size with unknown power. [29] applied a combination of the modalities taping and NMES, and did not find a significant difference of pain reduction. This study had a sample size of 21 of unknown power and a PEDro score of 7.
Taping: Two studies [17,26] applied a sling and two [20,21,23] applied various forms of taping (Tripull method [23] and Kinesiology Taping [20,21]) , but they did not find a reduction in PSSP. These studies scored between 6 and 8 on the PEDro scale, yet a calculated sample size of 162 participants was present in only one single study [23].
Discussion
This systematic review summarized and evaluated the effects of electrotherapy, training, exercise, thermotherapy and taping for hemiparetic Post Stroke Shoulder Pain (PSSP) originating from etiology such as capsulitis, (sub)luxation and contracture in studies published between 2008 and 2018. Most of the studies had sample sizes that were too small and were not triple blinded. The majority included only acute and subacute patients with PSSP originating from subluxation. Consequently, it was not possible to identify an effective physiotherapeutic modality to manage PSSP.
Similar modalities were observed for studies with both, significant difference of pain reduction [24,26,28,30,32,34,36- 39] and no significant difference of pain reduction [22,23,25,27,29,31,33,35,40] regarding PSSP for patients with stroke, but all studies had a significant risk of bias due to inadequate study designs, inconsistency of pain measurement, lack of inclusion of full sensory assessment and no description of the content of conventional therapy.
Eleven studies reported blinding of the assessors and patients, although none of the studies reported blinding of the therapists. Understandably the nature of physiotherapeutic interventions makes blinding difficult [37] but not impossible [38,39]. Triple blinding prevents performance bias associated to patient’s, therapist’s and assessor’s expectations [37] by assessing the limitations of each study due to bias control in order to avoid incorrect conclusions of the application of several modalities. It is therefore advisable to use open-label trials in order to have tripleblinded trials [40]. Open-label trials involve the comparison of two very similar trials in order to determine the most effective one [41]. Pain is not consistently described in the reviewed studies. Validity and uniformity is advisable since pain measurement is highly subjective [37]. Additionally, none of the studies reported full sensory assessment of participants. As stroke patients are subject to somatosensory disorders, pain assessment could therefore be biased [13]. Studies reported a prevalence varying from at least 33 to 79% [42,43] regarding somatosensory impairments after stroke.
In line with other reviews [11,44], no reduction for shoulder subluxation and shoulder pain for modalities such as electrotherapy, taping, sling and combination therapy (electrotherapy with taping) are reported. Furthermore, distinct phases and locations of stroke, varying intensities of the modalities and poor description of the content of conventional therapy [11,44] are examples of contributing factors that might mask the findings of all studies. This complex interrelated nature of components of physical therapy during treatment of PSSP makes it, therefore, imminent that the content of conventional therapy in addition to the intervention effect should be defined and reported in detail [15].
A limitation of this systematic review could be the use of the PEDro scale. It does not take the sample size calculation into account in comparison to, for instance, the Downs and Black scale [45]. Therefore, a high score on the PEDro scale is subject to interpretation bias. Yet, the PEDro scale was chosen in this systematic review over the Downs and Black scale in order to compare study results to other physiotherapeutic systematic reviews [11,44], and also due to its common use in the physiotherapeutic field [46]. Secondly, this review only included studies that were published in English, which may have resulted in omission of valid publications in other languages. Thirdly, the difference in severity of stroke among these studies challenges this study to conclude a clear effect of physiotherapeutic management on pain. At last, it should be mentioned that the etiology of PSSP is diverse and includes glenohumeral subluxation, spasticity of shoulder muscles, impingement, soft tissue trauma, rotator cuff tears, glenohumeral capsulitis, bicipital tendinitis and shoulder hand syndrome, from which we chose the most common etiologies, but future studies are encouraged to include other etiological factors as well in a systematic search [47].
Conclusion
Despite the high prevalence of patients suffering from PSSP, the evidence for effective physiotherapeutic treatment is unclear and no particular intervention appears to be preferred. Adequate study designs such as prospective controlled trials are required in order to have a better assessment for PSSP treatment. At this point, the applicability of physiotherapeutic modalities for PSSP originating from subluxation, contracture or capsulitis remains inconclusive
Declaration of Interest Statement
The authors report no conflicts of interest.
References
- Strong K, Mathers C, Bonita R (2007) Preventing stroke: Saving lives around the world. Lancet Neurol 6(2): 182-187.
- Hamzat TK, Osundiya OC (2010) Musculoskeletal pain and its impact on motor performance among stroke survivors. Hong Kong Physiotherapy Journal 28(1): 11-15.
- Harrison RA, Field TS (2015) Post stroke pain: Identification, assessment, and therapy. Cerebrovasc Dis 39(3-4): 190-201.
- Olawale OA, Ajepe TO, Oke KI (2017) Chronic Pain After Stroke: A Hospital-Based Study of Its Profile and Correlation with Health-Related Quality of Lif. Middle East J Rehabil Health 4(1): e41874.
- Langhorne P, Stott DJ, Robertson L, MacDonald J, Jones L, et al. (2000) Medical complications after stroke: A multicenter study. Stroke 31(6): 1223-1229.
- Choi-Kwon S, Choi SH, Suh M, Choi S, Cho KH, et al. (2017) Musculoskeletal and central pain at 1 year post-stroke: Associated factors and impact on quality of life. Acta Neurol Scand 135(4): 419-425.
- Lee JA, Park SW, Hwang PW, Lim SM, Kook S, et al. (2012) Acupuncture for shoulder pain after stroke: A systematic review. J Altern Complement Med 18(9): 818-823.
- Price CI, Pandyan AD (2001) Electrical stimulation for preventing and treating post-stroke shoulder pain: A systematic Cochrane review. Clin Rehabil 15(1): 5-19.
- Vafadar AK, Cote JN, Archambault PS (2015) Effectiveness of functional electrical stimulation in improving clinical outcomes in the upper arm following stroke: a systematic review and meta-analysis. Biomed Res Int 2015: 729768.
- Walsh K (2001) Management of shoulder pain in patients with stroke. Postgrad Med J 77(912): 645-649.
- Veerbeek JM, van Wegen E, van Peppen R, Jan van der Wees P, Hendriks E, et al. (2014) What is the evidence for physical therapy poststroke? A systematic review and meta-analysis. PLoS One 9(2): e87987.
- Maxwell AMW. NVQC. (2013) Management of hemiplegic shoulder pain. Current Physical Medicine and Rehabilitation Reports 1(1): 1-8.
- Suethanapornkul S, Kuptniratsaikul PS, Kuptniratsaikul V, et al. (2008) Post stroke shoulder subluxation and shoulder pain: a cohort multicenter study. J Med Assoc Thai 91(12): 1885-1892.
- Maher CG, Sherrington C, Herbert RD (2003) Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther 83(8): 713-721.
- Charrois TL (2015) Systematic reviews: What do you need to know to get started? JCPH 68(2): 144-148.
- Moher D, Liberati A, Tetzlaff J (2010) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg 8(5):336-341.
- Ada L, Foongchomcheay A, Langhammer B, Stanton R, John et al. (2017) Lap-tray and triangular sling are no more effective than a hemi-sling in preventing shoulder subluxation in those at risk early after stroke: a randomized trial. Eur J Phys Rehabil Med 53(1): 41-48.
- Chatterjee S, Hayner KA, Arumugam N, Goyal M, Divya M, et al. (2016) The California Tri-pull Taping Method in the Treatment of Shoulder Subluxation After Stroke: A Randomized Clinical Trial. N Am J Med Sci 8(4): 175-182.
- de Jong LD, Dijkstra PU, Gerritsen J (2013) Combined arm stretch positioning and neuromuscular electrical stimulation during rehabilitation does not improve range of motion, shoulder pain or function in patients after stroke: a randomised trial. J Physiother 59(4): 245-254.
- Huang YC, Chang KH, Liou TH (2017) Effects of Kinesio taping for stroke patients with hemiplegic shoulder pain: A double-blind, randomized, placebo-controlled study. J Rehabil Med 49(3): 208-215.
- Huang YC, Leong CP, Wang L, Liou TH, Cheng CW, et al. (2016) Effect of kinesiology taping on hemiplegic shoulder pain and functional outcomes in subacute stroke patients: a randomized controlled study. Eur J Phys Rehabil Med 52(6): 774-781.
- Mangold S, Schuster C, Keller T, Zimmermann-Schlatter A, Ettlin T, et al. (2009) Motor training of upper extremity with functional electrical stimulation in early stroke rehabilitation. Neurorehabil Neural Repair 23(2): 184-90.
- Pandian JD, Kaur P, Arora R, Dheeraj K, Toor T, et al. (2013) Shoulder taping reduces injury and pain in stroke patients: randomized controlled trial. Neurology 80(6): 528-532.
- Pillastrini P, Rocchi G, Deserri D (2016) Effectiveness of neuromuscular taping on painful hemiplegic shoulder: a randomised clinical trial. Disabil Rehabil 38(16): 1603-1609.
- Suriya-amarit D, Gaogasigam C, Siriphorn A (2014) Effect of interferential current stimulation in management of hemiplegic shoulder pain. Arch Phys Med Rehabil 95(8): 1441-1446.
- Van Bladel A, Lambrecht G, Oostra Km (2017) A Randomized Controlled Trial On The Immediate And Long-Term Effects Of Arm Slings On Shoulder Subluxation In Stroke Patients. Eur J Phys Rehabil Med 53(3): 400-409.
- Zhou M, Li F, Lu W (2018) Efficiency of Neuromuscular Electrical Stimulation and Transcutaneous Nerve Stimulation on Hemiplegic Shoulder Pain: A Randomized Controlled Trial. Arch Phys Med Rehabil 99(9): 1730-1739.
- Heo MY, Kim CY, Nam CW (2015) Influence of the application of inelastic taping on shoulder subluxation and pain changes in acute stroke patients. J Phys Ther Sci 27(11): 3393-3395.
- Hochsprung A, Dominguez-Matito A, Lopez-Hervas A (2017) Short- and medium-term effect of kinesio taping or electrical stimulation in hemiplegic shoulder pain prevention: A randomized controlled pilot trial. NeuroRehabilitation 41(4): 801-810.
- Türkkan C, Öztürk GT, Uğurlu FG (2017) Ultrasonographic assessment of neuromuscular electrical stimulation efficacy on glenohumeral subluxation in patients with hemiplegia: A randomized-controlled study. Turkish Society of Physical Medicine and Rehabilitation 63(4): 287-292.
- Jeon S, Kim Y, Jung K (2017) The effects of electromyography-triggered electrical stimulation on shoulder subluxation, muscle activation, pain, and function in persons with stroke: A pilot study. NeuroRehabilitation 40(1): 69-75.
- Karaahmet OZ, Gurcay E, Unal ZK (2018) Effects of functional electrical stimulation-cycling on shoulder pain and subluxation in patients with acute-subacute stroke: A pilot study. Int J Rehabil Res 42(1): 36-40.
- Manigandan JB, Ganesh GS, Pattnaik M (2014) Effect of electrical stimulation to long head of biceps in reducing gleno humeral subluxation after stroke. NeuroRehabilitation 34(2): 245-252.
- Koyuncu E, Nakipoglu-Yuzer GF, Dogan A (2010) The effectiveness of functional electrical stimulation for the treatment of shoulder subluxation and shoulder pain in hemiplegic patients: A randomized controlled trial. Disabil Rehabil 32(7):560-6.
- Moniruzzaman M, Salek KM, Shakoor MA (2010) Effects of therapeutic modalities on patients with post stroke shoulder pain. Mymensingh Med J 19(1): 48-53.
- Vermeulen HM, Boonman DC, Schuller HM (2005) Translation, adaptation and validation of the Shoulder Rating Questionnaire (SRQ) into the Dutch language. Clin Rehabil 19(3): 300-11.
- Armijo-Olivo S, Fuentes J, da Costa BR (2017) Blinding in Physical Therapy Trials and Its Association with Treatment Effects: A Meta-epidemiological Study. Am J Phys Med Rehabil 96(1): 34-44.
- Martin PR, Nichols PJ, Russell PL, Hughes IG (1986) Physiotherapy exercises for low back pain: process and clinical outcome. Int Rehabil Med 8(1): 34-38.
- Deyo RA WNE, Schoenfeld LS, Ramamurthy S (1990) Can trials of physical treatments be blinded? The example of transcutaneous electrical nerve stinulation for chronic pain. Am J Phys Med Rehabil 69(1): 6-10.
- Jozef Opara CK, Andrzej Malecki, Jan Pilch (2013) Methods of blinding clinical trials in physiotherapy. Fizjoterapia 21(1): 62-64.
- Ramakrishnan TCR, Kumaravelu S, Narayan SK (2018) Efficacy and Safety of Intravenous Tenecteplase Bolus in Acute Ischemic Stroke: Results of Two Open-Label, Multicenter Trials. Am J Cardiovasc Drugs 18(5): 387-395.
- Bowden JL, Lin GG, McNulty PA (2014) The prevalence and magnitude of impaired cutaneous sensation across the hand in the chronic period post-stroke. PLoS One 9(8): e104153.
- De Bruyn N, Meyer S, Kessner SS (2018) Functional network connectivity is altered in patients with upper limb somatosensory impairments in the acute phase post stroke: A cross-sectional study. PLoS One 13(10): e0205693.
- Lee JH, Baker LL, Johnson RE (2017) Effectiveness of neuromuscular electrical stimulation for management of shoulder subluxation post-stroke: a systematic review with meta-analysis. Clin Rehabil 31(11): 1431-1444.
- Olivo SA, Macedo LG, Gadotti IC (2008) Scales to assess the quality of randomized controlled trials: a systematic review. Phys Ther 88(2): 156-75.
- Bhogal SK, Teasell RW, Foley NC (2005) The PEDro scale provides a more comprehensive measure of methodological quality than the Jadad scale in stroke rehabilitation literature. J Clin Epidemiol 58(7): 668-673.
- Association AS (2018) Managing pain American Stroke Association.
© 2020 Robbert Bipat. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






