- Submissions

Full Text
Examines in Physical Medicine and Rehabilitation: Open Access
Atypical Antipsychotic as Add-on Therapy in Obsessive Compulsive Disorder
Shoja Shafti S*
Department of Psychiatry, Iran
*Corresponding author: Shoja Shafti S, University of Social Welfare and Rehabilitation sciences (USWR), Razi Psychiatric Hospital, Tehran, Iran
Submission: May 07, 2018;Published: February 05, 2019

ISSN 2637-7934 Volume2 Issue2
Abstract
In an 8-week, open-label study, 54% (n=6) of treatment-resistant obsessive-compulsive patients (n=11) responded to adding olanzapine to current antidepressant treatment, with a mean reduction of 24.56% in YBOCS, as the primary outcome measure.
Keywords: Obsessive-compulsive disorder; Serotonin reuptake inhibitors; Olanzapine; Treatment resistant
Introduction
Specific Serotonin Reuptake Inhibitors (SSRIs) are the most effective drugs available for Obsessive-Compulsive Disorder (OCD) [1]. Fluvoxamine, Clomipramine, Fluoxetine, Citalopram, Paroxetine, and Sertraline have been shown to be operative against obsessive and compulsive symptoms, independent of their antidepressant action [2-4]. Nonetheless, while 50%-60% of patients with OCD fail to respond to a single trial of an SRI, 20-40% does not respond amply even after several drug trials [1]. Furthermore, though the SSRIs are usually considered to be safe and well-tolerated, still a percentage of subjects do experience unbearable adverse effects and discontinue treatment too early. Besides, no single drug, acting on different neurotransmitter systems, has yet shown a complete effectiveness against obsessive-compulsive symptoms.
Therapeutic approaches in these resistant patients typically consist of augmentation treatments with buspirone, tryptophan, lithium and clonazepam or the addition of antipsychotic medications. But then again, the absolute results with these maneuvers were not promising so far and have remained rather investigational than decisive. Adding low-dose antipsychotics to standard antidepressant treatment has shown to be operative in some patients, but extra-pyramidal adverse effects have limited the use of conventional antipsychotics. Therefore, management with atypical antipsychotics, which show fewer extra-pyramidal symptoms, could be a suitable alternative for treatment-resistant OCD patients. Helpful effects of adding risperidone to SSRIs has been detected in some cases of treatment-refractory OCD [5,6]. In previous reports (4 open and 1 double-blind studies) affirmative outcomes with the addition of olanzapine to the regular antidepressant treatment of the cases [7-11] have been demonstrated. In the current study a new assessment with olanzapine has been accomplished, in a nonwestern patient population, with treatment-resistant OCD.
Method
Eleven female outpatients, after complete description of the process for them and earning assigned informed agreement, came into the evaluation. The mean +/-SD age of the subjects was 39.2+/-9.08 years. All patients have been diagnosed as OCD, according to the DSM-TR criteria. ‘Inclusion criteria’ in the current study consisted: 1-OCD symptoms of at least 3 years’ period, and 2- a score on the YBOCS [12] of at least 18. The subject’s mean +/- SD baseline score on the YBOCS was 33.45+/-4.47 and the mean length of illness was 16.3+/-7.35 years. All the patients had both obsessions and compulsions. Besides, all cases had failed at least two treatments with an SRI at maximum dosage (Fluvoxamine 300mg/day, Clomipramine 250mg/day, Sertraline 200mg/day, Fluoxetine 80mg/day, Citalopram 80mg/day) and sufficient period (12 weeks). Failure had been defined as a less than 25% improvement on the YBOCS.
In an eight-week assessment, all patients continued to take their recommended SRI at the maximum dose throughout evaluation. 4 patients received Clomipramine (250mg/day), three patients received fluvoxamine (300mg/day), two patients received fluoxetine (80mg/day), one patient received sertraline (200mg/day) and one patient received citalopram (80mg/day). Olanzapine (in generic-form tablets) adding was started at a dose of 2.5mg per day and had been increased by 2.5mg increments in weekly consultations, to a maximum of 10mg by week 4, and then this dosage had been held unbroken up to the end of the evaluation. No other psychosocial intervention or psychotropic drug was allowable throughout the appraisal. Patients had been visited by the identical qualified appraiser at starting point (week 0 or baseline) and at the end of 4th and 8th week, when adverse events and clinical response had been evaluated. The appraiser was not blind to the management and its objectives. The primary efficacy parameter was YBOCS score [12]. Complete response to treatment was prospectively demarcated of at least 50% reduction in YBOCS and partial response of at least 25% reduction in YBOCS in comparison with baseline. Side effects had been measured at each visit by means of patients’ reports and clinical examination by the aforesaid psychiatrist.
Result
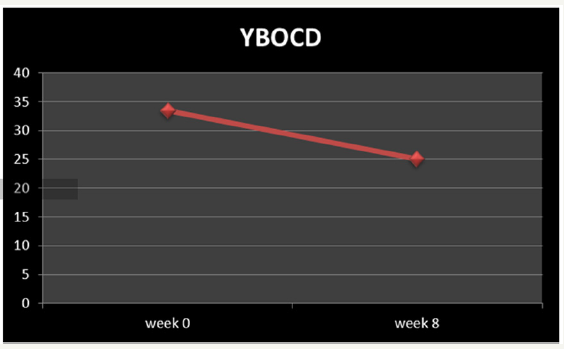
Two of the cases were among full responders with a mean decrease of 51% in YBOCS’ score. Four patients were among partial responders with at least a 25% reduction. Five patients experienced no alteration in their obsessive-compulsive symptoms (Table 1 & Figure 1). In those who profited from the management, enhancement initiated within the first 2 weeks of olanzapine addition. On the whole, patients mean YBOCS score diminished meaningfully (by 24.56%) from baseline (starting point) to endpoint (t=4.23, df=10, p< 0.002) (Table 1 & Figure 2). The most common side effects of olanzapine in the present assessment were somnolence (n=3), weight gain (n=2), dyspepsia (n=2), dizziness (n=2), constipation (n=1) and tremor (n=1). Since the adverse effects were slight and well-tolerated, no one dropped out owed to drug intolerance.
Table 1:Characteristics of the participants, and the outcome of the assessment.
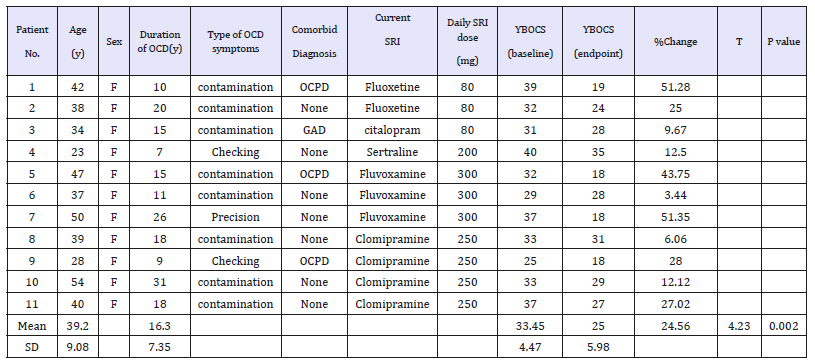
Abbreviations: GAD: Generalized Anxiety Disorder; YBOCS: Yale-Brown Obsessive-Compulsive Scale; OCD: Obsessive-Compulsive Disorder; OCPD: Obsessive-Compulsive Personality Disorder
Figure 1:Percentage of response of participants to add-on therapy.
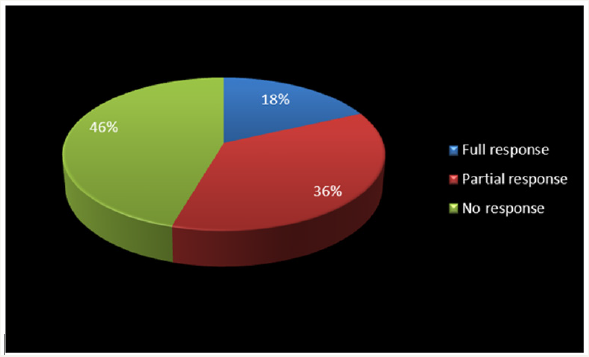
Figure 2:Mean total Decrease of YBOCD between baseline (week 0) and week 8.
Discussion
This trial affords extra evidence that adding olanzapine to current SRI treatment may be effective for therapy-refractory OCD cases. There are, nevertheless, restrictions to the information presented because of the small sample size and open-label project. In all, the outcomes of our assessment are in accordance with the findings of preceding similar trials with olanzapine and risperidone [5-11]. Enhancing SRIs with atypical antipsychotics displays profits, but the foremost problem here is that there is some discrepancy in the meaning of management refractoriness. Most evaluations encompassed cases who had failed to respond to merely one SRI trial. They should somewhat be eligible as treatment-resistant. The problem of poor response is an area under debate and merits additional investigation.
Also, a clear criterion for no-response necessities to be agreed upon since regularly the standards for response rates vary to a great extent. For example, Weiss et al. [7] used a cut-off of 50% reduction in YBOCS score as responders, while Francobanderia [10] picked a cut-off of 25%. McDougal et al. [6], alternatively, used a more limiting criterion with a cut-off of 35% for YBOCS diminution and a final score of 16 on the YBOCS in combination with a final Clinical Global Impressions scale rating of ‘much improved’ or ‘very much improved’. Such variances invalidate the comparison of Effect Sizes between different evaluations. Besides, atypical antipsychotics may augment the action of SRIs by means of serotonin receptor blockade. The broader range of effective treatment with the addition of atypical antipsychotics may be because of a D2 blockade, or a combined serotonergic-dopaminergic blockade, particularly D2 and 5-HT2A antagonism [5]. Anyway, adding atypical antipsychotics to SRIs seems a promising pharmacotherapy intervention for treatmentresistant OCD patients. Undoubtedly, further studies with regard to the mechanism of action of these augmentative tactics for OCD are necessary.
Conclusion
According to the findings of the present assessment, addition of olanzapine to serotonin-reuptake inhibitor, as an augmentative medication, can be a valuable approach in treatment-resistant obsessive-compulsive disorder.
References
- Fienberg NA, Bullock T, Montgomery DB, Montgomery SA (1992) Serotonin reuptake inhibitors are the treatment of choice in obsessivecompulsive disorder. Clin Psychopharmacology 7(Suppl 1): 43-47.
- Mcdougle CJ, Gordman WK, Price LH (1993) The pharmacotherapy of obsessive-compulsive disorder. Pharmopsychiatry 269(Suppl): 24.
- Hollander E, Kaplan A, Allen A, Cartwright C (2000) Pharmacotherapy for obsessive-compulsive disorder. Psychiatric Clin North AM 23(3): 643-656.
- Goodman WK, Price LH, Rasmussen SA, Delgado PL, Heninger GR, et al. (1989) Efficacy of fluvoxamine in obsessive-compulsive disorder: a comparison with placebo. Arch Gen Psychiatry 46(1): 36-44.
- McDougle CJ, Fleischmann RL, Epperson CN, Wasylink S, Leckman JF, et al. (1995) Risperidone addition in fluvoxamine-refractory obsessivecompulsive disorder: three cases. J Clin Psychiatry 56(11): 526-528.
- McDougle CJ, Epperson CN, Pelton GH, Wasylink S, Price LH (2000) A double-blind, placebo-controlled study of resperidone addition in serotonin reuptake inhibitor-refractory obsessive-compulsive disorder. Arch Gen Psychiatry 57(8): 794-801.
- Weiss El, Potenza MN, McDougle CJ, Epperson CN (1999) Olanzapine addition in obsessive-compulsive disorder refractory to selective serotonin reuptake inhibitors; an open-label case series. J Clin Psychiatry 60(8): 524-527.
- Koran LM, Ringold AL, Elliot MA (2000) Olanzapine augmentation for treatment-resistant obsessive-compulsive disorder. J Clin Psychiatry 61(7): 514-517.
- Bogetto F, Bellino S, Vaschetto P, Ziero S (2000) Olanzapine augmentation of fluvoxamine-refrectory obsessive-compulsive disorder (OCD): a 12- week open trial. Psychiatry Res 96(2): 91-98.
- Francobandiera G (2001) Olanzapine augmentation of serotonin uptake inhibitors in obsessive-compulsive disorder: an open study. Can J Psychiatry 46(4): 356-358.
- Bystrisky A, Ackerman DL, Rosen RM, Vapnik T, Gorbis E, et al. (2001) Augmentation of SSRI response in refractory OCD using adjunctive olanzapine: a placebo-controlled trial. J Clin Psychiatry 65(4): 565-568.
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, et al. (1998) The Yale-brown obsessive-compulsive scale, 1: development, use, and reliability. Arch Gen Psychiatry 46(11): 1006-1011
© 2019 Shoja Shafti S. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






