- Submissions

Full Text
Environmental Analysis & Ecology Studies
Autism Spectrum Disorder and Attention Deficit/Hyperactivity Disorder in Children with Inflammatory Bowel Disease
Hasret Ayyıldız Civan1* and Gonca Bektaş2
1Department of Gastroenterology, Hepatology and Nutrition, Turkey
2Department of Pediatric Neurology, Training and Research Hospital, Turkey
*Corresponding author: Hasret Ayyildiz Civan, Department of Gastroenterology, Hepatology and Nutrition, Bakırköy, Turkey
Submission: January 25, 2021; Published: November 23, 2021

ISSN 2578-0336 Volume9 Issue2
Abstract
Objective: Inflammatory Bowel Diseases (IBD) are accompanied by some psychiatric disturbances
some of which are suggested to have a common pathophysiological pathway related to the intestinal
malfunction, The goal of the study was to evaluate the presence of symptoms associated with Autism
Spectrum Disorder (ASD) and Attention Deficit/Hyperactivity Disorder (ADHD) in children with IBD and
to investigate the relation of symptoms to their clinical features.
Methods: A total of 42 children with IBD, either ulcerative colitis or Crohn disease and 45 healthy
controls were included. Demographic features, the duration of the IBD and currently used medications
were recorded. The Social Communication Questionnaire (SCQ) and Turgay DSM-IV Disruptive Behavior
Disorders Rating Scale (T-DSM-IV-S) were employed for ASD and ADHD related symptoms.
Result: The mean total SCQ score, the SCQ reciprocal social interaction score, and the SCQ communication
score were significantly higher in children with IBD indicating an increased likelihood for ASD whereas
total T-DSM-IV-S and subscale scores for hyperactivity- impulsivity and inattention were not statistically
different between groups. However, 4 patients with IBD (10%) presented an increased likelihood for
ADHD with more positive items whereas none of the healthy controls presented an increased likelihood
for ADHD.
Conclusion: Children with IBD may have a higher risk of having ASD and ADHD without regard
to the age, age at disease onset and the duration of IBD. Young patients with IBD should be assessed in
terms of neurodevelopmental disorders.
Keywords: Inflammatory bowel diseases; Autism spectrum disorder; Attention deficit/hyperactivity disorder; ADHD
Introduction
Inflammatory Bowel Diseases (IBD) are a group of immune-mediated disorders involving
Crohn disease, ulcerative colitis and indeterminate colitis. Although not particularly an
etiology of mortality, IBD are associated with significant morbidity and impact on the quality
of life. Thromboembolism, malignancies, hepatobiliary disorders, decrease or increase in the
diversity of bacteria in the gut, arthropathies and high levels of psychological stress are among
those morbidities and related complications. Considering the extra-intestinal manifestations
of IBD, those involving the psychiatric pathologies are relatively rare.
Attention-Deficit/Hyperactivity Disorder (ADHD), on the other hand, is a clinical
entity marked by a continuous pattern of inattention and/or hyperactivity-impulsivity
that restrains functioning or development, whereas Autism Spectrum Disorder (ASD) is a
developmental issue that disrupt communication and behavior. Both ADHD and ASD may be associated by gastrointestinal symptoms or complications.
Evidence from the current literature suggests a combination of
changes in gut microflora, intestinal permeability, inappropriate
immune response, activation of specific metabolic pathways, and
behavioral changes in genetically predisposed individuals, which
notes multiple intersection points of IBD and psychiatric issues [1].
The aims of this study were to evaluate the presence of
symptoms associated with ASD and ADHD in children with IBD, and
to investigate whether there is an association of these symptoms to
the clinical features of the children with IBD.
Methods
This was a single-center prospective case-control study including children with IBD followed-up by the pediatric gastroenterology outpatient clinic at the Bakirkoy Dr. Sadi Konuk Research and Training Hospital from February 1st, 2019 to August 1st, 2019.
Participants
The inclusion criteria were as follows; children with IBD, either
ulcerative colitis or Crohn disease, and aged 6-18 years. The IBD
was diagnosed according to ESPGHAN revised Porto criteria [1].
Children with a preexisting neurological or psychiatric disorder
were excluded from the study. Healthy subjects matched by age,
sex, and socioeconomic status constituted the control group.
The study was reviewed and approved by the Institutional
Ethics Committee at the Bakirkoy Dr. Sadi Konuk Research and
Training Hospital. All participants were asked for assent and their
legal representatives provided written informed consent.
Clinical data and neuropsychological assessment
Demographic features, the duration of the IBD, and the currently
used medications were abstracted from medical records. All
participants were evaluated by standardized assessment batteries
completed by parents or caregivers. The Social Communication
Questionnaire (SCQ) and Turgay DSM-IV Disruptive Behavior
Disorders Rating Scale (T- DSM-IV-S) were the used instruments to
assess ASD and ADHD related symptoms.
The features of ASD were screened utilizing SCQ based on
3 subscales; reciprocal social interaction, communication, and
restricted, repetitive, stereotyped patterns of behavior. SCQ, a 40-
item questionnaire, was reported as a reliable and valid tool for
children aged 4 to 18 years [2-4]. The score of each item ranges
0 to 1 and the total scores range between from 0 to 39. The total
score above the threshold of 15 represents a likelihood of ASD.
T-DSM-IV-S is an instrument that evaluates the ADHD symptoms. It
has four subscales including hyperactivity/impulsivity, inattention,
opposition-defiance, and conduct disorder. T-DSM-IV-S is a
reliable and valid tool to measure ADHD related symptoms [5,6].
Hyperactivity-impulsivity (9 items), inattention (9 items) and total
ADHD (18 items) scores were examined in our analyses. Each item
was scored based on the severity of symptom from 0 to 3 points,
in which higher scores representing more psychopathology. Also,
each item was defined as positive if scored as 2 or 3, and negative
if scored as 0 or 1. ADHD type was classified based on the number
of positive items of hyperactivity-impulsivity or inattention, which
requires more than 5 positive items.
Statistical analysis
All statistical analyses were applied using SPSS Statistics for Windows version 23.0 (IBM Corp., Armonk, NY, USA). The distribution of variables was determined by Kolmogorov-Smirnov test. Demographic features and the scores of instruments were assessed using independent samples t-tests in case of normality and homogeneity of variances, or Mann-Whitney U-tests otherwise. The value of p < 0.05 was accepted as statistically significant.
Result
Demographic and clinical characteristics
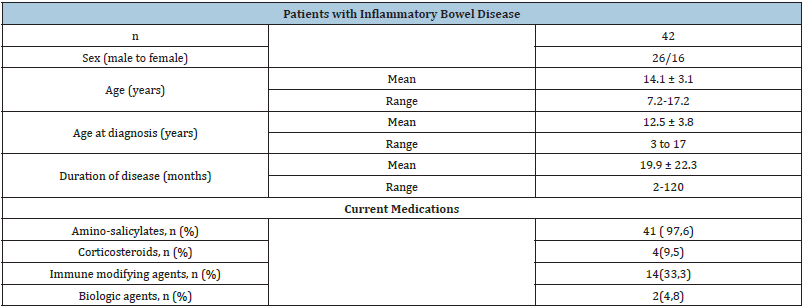
A total of 87 children, 42 children with IBD and 45 healthy
controls, were evaluated. The patient group included 26boys and
16girls with a ratio of 1:1.6, indicating slightly male predominance.
The mean age of patients was 14.1±3.1 (range 7.2-17.2 years) with
an age at disease onset of 12.5±3.8 years (range 3-17 years). The
mean duration of disease was 19.9±22.3 months (range 2-120
months).
The overall 42 patients with IBD consisted of 31 (18 males)
patients with ulcerative colitis and 11 (8 males) patients with
Crohn disease. The currently used medications of children with
IBD were amino-salicylates in 41 patients (97,6 %); corticosteroids
in 4 (9,5%),immune modifying agents in 14(33,3%), and biologic
agents (adalimumab, infliximab) in 2(4,8%). The demographic and
clinical characteristics of participants are provided in Table 1.
Table 1: Demographic and clinical features of children with inflammatory bowel disease.
*Used doses: Trichoderma reesei - 100mL/ha, Bacillus megaterium - 100mL/ha, Acinetobacter calcoaceticus - 100mL/ ha, ammonium nitrate - 20kg N/t residues.
Neuropsychological assessment
All participants were evaluated using both the SCQ and T-DSMIV- S. The mean total SCQ score, the SCQ reciprocal social interaction score, and the SCQ communication score were significantly higher in children with IBD compared to healthy controls (p=0.002, p=0.001, p<0.001, respectively) (Figure 1). There was no significant difference observed between two groups in terms of the SCQ restricted interests score (p=0.57). Eight patients (19%) among patients with IBD versus 1 child (2%) in the control group exhibited a score above the cut-off value, indicating an increased likelihood for ASD.
Figure 1: Box plots for reciprocal social interaction, communication score, restricted interests score, and total SCQ score in children with inflammatory bowel disease and healthy controls.

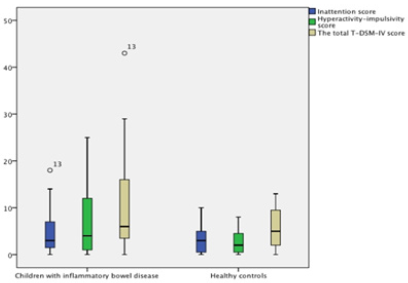
The total T-DSM-IV-S score and subscale scores for
hyperactivity-impulsivity and inattention were not statistically
different between patients with IBD and healthy controls
(p=0.097, p=0.17, p=0.91, respectively) (Figure 2). The number
of positive items for hyperactivity-impulsivity and inattention
were significantly different between patients with IBD and healthy
controls (p=0.018, p=0.04, respectively). A total of 4 patients with
IBD (10%) presented an increased likelihood for ADHD (1 patient
for the hyperactivity- impulsivity type and the remaining for the
mixed type), whereas none of the healthy controls presented an
increased likelihood for ADHD.
We observed no correlation between the SDQ and T-DSM-IV-S
scores and clinical variables including the age, the age at disease
onset, disease duration (p>0.05).
Figure 2: Box plots for inattention, hyperactivity-impulsivity scores and total T-DSM-IV score in children with inflammatory bowel disease and healthy controls.
Discussion
In our study, children with IBD presented an increased
likelihood of ASD and ADHD related symptoms compared to
healthy controls. In terms of ASD, the reciprocal social interaction
and communication more likely impaired in children with IBD
than healthy children, whereas restricted interests were similar
between both groups. Also, children with IBD were more prone to
exhibit symptoms of hyperactivity-impulsivity and inattention than
healthy children.
The prevalence of ADHD ranges from 1.4% to 3.4% in the
general population, depending on the diagnostic approach [7,8].
Overall, among children with IBD, the risk of having ADHD was 10%,
which was more than the general population and healthy controls.
The relationship between ADHD and IBD has been previously
defined in a study with a large sample size, which indicates a 1.2-
fold increase in the risk of ADHD in children with IBD [9]. ADHD has
been related to multifactorial pathogenic mechanisms including
genetics and environmental factors [10]. It has been suggested
that the increase in dopamine precursors related to altered gut
microbiome functions may lead to the core symptoms of ADHD
[11]. This observation may clarify the increased likelihood of ADHD
in children with IBD.
In our study, ASD related symptoms were more common in
children with IBD than healthy children, in line with previous
studies showing a 1.4-fold increased risk [12]. The underlying
pathogenic mechanism for ASD is defined as multifactorial. Besides
genetic factors, it has been suggested that inflammation and
immunity, triggered by the impaired intestinal barrier, may play a
role in the pathogenesis of the disease [13]. On the other side, it has
been notified the epithelial barrier genes showed altered functions
in the active state of IBD [14]. Therefore, the proposed brain-gutmicrobiome
axis may be responsible for the association between
IBD and ASD.
The pediatric IBD population was reported to have a
higher frequency of poor adherence to oral drugs, namely
immunomodulators and mesalamine [15]. Additionally, in case
of ASD, where children may have challenging attitudes and
noncompliance to therapies, adalimumab or certolizumab may
have been preferred as they are administered with subcutaneous
injections and thus more effective in terms of compliance and
feasibility, and not necessarily associated with inherent severity. In
our study, however, two of the cases were taking biologic agents
which had been initiated for juvenile idiopathic arthritis. Thus, oral
medications were well tolerated with good compliance in our study
population.
Our study has some limitations. Firstly, the small sample size
and the lack of confirmatory evaluation to diagnose ASD and ADHD
are significant. Secondly, the correlation of the IBD activity index to
the scores of screening tools for ASD and ADHD may help to improve
the understanding of the association of these disorders. It has been
reported that uninflamed mucosa represents normal intestinal
barrier gene levels [14]. Therefore, to compare the presence of ASD
and ADHD related symptoms between the active state of disease
and following disease control may be valuable.
In conclusion, our results showed that children with IBD may
have an increased risk of having ASD and ADHD irrespective of the
age, age at disease onset and the duration of IBD. All children with
IBD should be monitored for the neuro-developmental disorders.
References
- Coury DL, Ashwood P, Fasano A, George F, Maureen G, et al. (2012) Gastrointestinal conditions in children with autism spectrum disorder: Developing a research agenda. Pediatrics 130(Suppl 2): 160-168.
- Berument K, Rutter M, Lord C, Pickles A, Bailey A, et al. (1999) Autism Screening Questionnaire: diagnostic Validity. Br J Psychiatry 175: 444-451.
- Avcil S, Baykara B, Baydur H, Kerim MM, Neslihan İE, et al. (2015) The validity and reliability of the Social Communication Questionnaire- Turkish form in autistics aged 4-18 years. Turk Psikiyatri Derg 26(1): 56-64.
- Öner P, Öner Ö, Çöp E, Kerim MM (2012) Reliability and validity of the Turkish version of the social communication scale. Klinik Psikofarmakol Bulteni 22(1): 43-50.
- Turgay A (1994) Disruptive behavior disorders child and adolescent screening and rating scales for children, adolescents, parents and teachers. Integrative Therapy Institute Publication, West Bloomfield, Michigan, USA.
- Ercan ES, Amado S, Somer O (2001) Development of a test battery for the assessment of attention deficit hyperactivity disorder. Turk J Child Adolesc Ment Health 8: 132-144.
- Polanczyk GV, Salum GA, Sugaya LS, et al. (2015) Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry 56: 345-365.
- Meltzer H, Gatward R, Goodman R, T Ford (2003) Mental health of children and adolescents in great Britain. Int Rev Psychiatry 15(1-2): 185-187.
- Butwicka A, Olén O, Larsson H, Jonas H, Catarina A, et al. (2019) Association of childhood-onset inflammatory bowel disease with risk of psychiatric disorders and suicide attempt. JAMA pediatrics 173(10): 969-978.
- Thapar A, Cooper M (2016) Attention deficit hyperactivity disorder. The Lancet 387(10024): 1240-1250.
- Aarts E, Ederveen TH, Naaijen J, Marcel PZ, Jos B, et al. (2017) Gut microbiome in ADHD and its relation to neural reward anticipation. PLoS One 12(9): e0183509.
- Butwicka A, Olén O, Larsson H, Jonas H, Catarina A, et al. (2019) Association of childhood-onset inflammatory bowel disease with risk of psychiatric disorders and suicide attempt. JAMA Pediat 173(10): 969-978.
- Fiorentino M, Sapone A, Senger S,Stephanie SC, Sarah MK, et al. (2016) Blood-brain barrier and intestinal epithelial barrier alterations in autism spectrum disorders. Molecular autism 7(1): 49.
- Vancamelbeke M, Vanuytsel T, Farré R, Sare V, Marc F, et al. (2017) Genetic and transcriptomic bases of intestinal epithelial barrier dysfunction in inflammatory bowel disease. Inflammatory Bowel Dis 23(10): 1718-1729.
© 2021 © Hasret Ayyıldız Civan. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






