- Submissions

Full Text
Determinations in Nanomedicine & Nanotechnology
Nanodrugs to End Viral Infection in Pancreatic β-Cell and Pyknosis
Rajiv Kumar*
National Institute of Medical Science, India
*Corresponding author: Rajiv Kumar, National Institute of Medical Science, India
Submission: July16, 2020;Published: July 22, 2020

ISSN: 2832-4439 Volume2 Issue1
Introduction
Diabetes mellitus, a metabolic disorder wherein the natural ability of the insulin to hold surfaces well tumbledown and because of it, the surface receptors turn erroneous in the creation of insulin. Thus, the pancreatic β-cell initiates mass reduction lead to types 1 and 2 diabetes [1,2]. This is a nonstop unanimity of lowering the secretion of insulin from top to bottom trigger numerous negative inferences, reparations, and dysfunction of organs (eyes, kidneys, blood vessels, nerves, and heart) [3]. In diabetes, the etiology of β-cell death and ongoing multifaceted mechanisms of mitochondria uphold precarious implications. Wantonness in the routine of the progressive β-cells, hyperglycemia and chronic inflammatory itineraries lead more imperfections in the secretion of insulin caused unpredictable dysfunction (improper functioning of granulocytes, monocyte/macrophages, natural killer cells, dendritic cells, T-cells, B-cells, and destroy cytokine signaling by producing of IL1β mediator) in nearby cells and organelles too. Later on, it initiates inflammation and amplified oxidative stress.
Such annoying happenings assassinate glutathione efficiency which safeguards DNA, proteins, and lipid membranes on or after radical outbreaks. Such transgressions doings augment the level of 3-nitrotyrosine, a key factor to initiate diabetes and pyknosis. Enteroviruses, (Cytomegalovirus, Epstein-Barr virus, Mumps virus, Rotavirus, Parvovirus B19, and Human Endogenous Retroviruses) infections highlighted as the foremost cause for fiascoes in the routine functioning of pancreatic β-cells. The pathways of progressive autoimmune-mediated catalysis answerable for amplified biological routes (pathology of pancreatic β-cell mass lose, apoptosis, immunological implications, and enteroviral tropism). These viruses infect and alter the islets of nondiabetic donors, as well as gene expression profiles of the virus strain. Such transformations instigate upregulation of pro-inflammatory cytokines interleukin 1α (IL-1α), IL-1β, viral inclusions, and coeval, enrich apoptosis, and proliferate pyknosis [4,5].
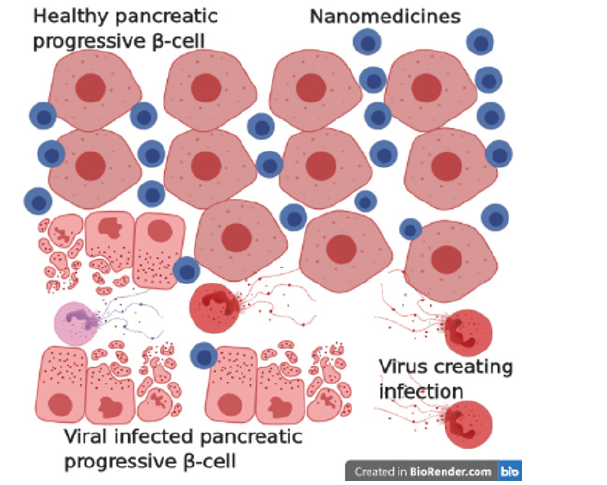
Cellular permissiveness to viral infection is modulated by kick off innate antiviral ripostes from the poles apart cells. Usually, pancreatic islet α cells trigger antiviral response proficiently to do battle with these diabetogenic viruses to a certain degree do β-cells to get rid of viral infections intuitively without undergoing apoptosis. Nanoparticles of albumin (non-toxic, non-immunogenic, biocompatible, and biodegradable) emerged as a versatile source to incorporate with macromolecular protein as therapeutic and theranostic resources to cure unhealthy and infected pancreatic β-cell and to stop pyknosis. These nanoparticles are impasse with bioactive molecules (chemicals, proteins/peptides, and oligonucleotides) and macromolecules having better-quality of pharmacokinetics to enhance longer circulation time, disease-specific buildup and easy to use a carrier for antiviral drugs across molecular barriers of cells deftly (Figure 1).
Figure 1: Schematic representation of the mechanism of nanomedicine’s impact on various stages of pancreatic β-cell, prevention routes, therapeutics, riposte for destroying viruses, and other virus creating the infection.
Conclusion
These innovations (glucose nanosensors, carbon nanotubes, quantum dots, nanopumps, oral insulins, microspheres, and artificial pancreas) in nanotechnology renewing cure preferences for the bloodbath of infected pancreatic β-cell. Further discoveries on the routes and types of machinery of vital diabetogenic viruses responsible for insulitis may be helpful in the innovation of novel nanovaccines to end metabolic virus’s blameworthiness liable for crafting infection in pancreatic β-cell and catalyzing pyknosis.
References
- Kahn SE (2003) The relative contribution of insulin resistance and beta‐cell dysfunction to the pathophysiology of type 2 diabetes. Diabetologia 46: 3-19.
- American Diabetes Association (2015) 2. Classification and diagnosis of diabetes. Diabetes Care 38: S8-S16.
- Alicic, RZ, Tuttle, KR (2014) Novel therapies for diabetic kidney disease. Adv Chronic Kidney Dis 21(2): 121-133.
- Antje P, Michele S, Klaus-Peter K (2015) Mechanisms of beta cell dysfunction associated with viral infection. Current Diab Rep 15(10): 73.
- Lopes M, Shrestha N, Correia A, Shahbazi MA, Sarmento B, et al. (2016) Dual chitosan/albumin-coated alginate/dextran sulfate nanoparticles for enhanced oral delivery of insulin. J Control Release 232: 29-41.
© 2020 Baidoo Philip. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






