- Submissions

Full Text
Developments in Clinical & Medical Pathology
Meta-Cognitive Therapy for Depression with Anxiety Features: A Case Study
Vandita SharmaandManju Mehta*
All India Institute of Medical Sciences, New Delhi, India
*Corresponding author: Manju Mehta, All India Institute of Medical Sciences, New Delhi, India
Submission: February 02, 2018;Published: July 17, 2018
ISSN:2690-9731 Volume1 Issue5
Abstract
Metacognitive Therapy (MCT) for depression and anxiety Wells [1] is based on the idea that persistent emotional distress is a consequence of a particular way of responding to negative thoughts and emotions. MCT for depression and anxiety aims at targeting attentional control, rumination, worry, and metacognitive beliefs of individuals. The purpose of this study was to examine the effect of meta-cognitive therapy (MCT) in the treatment of a patient diagnosed with major depressive disorder with anxiety features using an AB-design with repeated assessments at baseline, post-intervention, and follow-up. Following 10 sessions of MCT, it was observed that there were clinically significant improvements on outcome measures. A significant decrease in anxiety and depression symptoms and loss of diagnostic status was observed. It was concluded that MCT seems to be promising approach in managing the highly comorbid depression and anxiety symptoms. Further testing using more powered methodologies are needed.
Keywords: Meta cognitive therapy; Depression; Anxiety; Rumination; Worry; Cognitive attentional syndrome
Introduction
Over the past two decades, the prevalence of co-morbid mental and physical diseases has reached epidemic proportions in many counties. In individuals above the age of 60 years, cooccurrence of two or more disorders has become a norm rather than an exception. Depressive and anxiety symptoms often cooccur in patients with a primary diagnosis of either a depressive or anxiety disorder Brown 2001;Wiethoff 2010 with some studies reporting the prevalence rates to be as high as 60 %. Kaufman J, Chaney D 2000. This co-morbid symptomatology has often leaded to complications in treatment and worse outcomes Joffe 1993; Zajecka& Ross 1995; Fava 2004; Wiethoff2010. According to the NICE guidelines (2015) pharmacotherapy alone is not the recommended first line treatment in recent onset mild depression. Combination treatments including active monitoring of symptoms, individual guided self-help, increased physical activity and psychotherapies are preferredNational Institute for Clinical Excellence 2015. Combination treatment with psychotherapy and pharmacotherapy has also been recommended as the first line treatment recommended for chronic depression Jobse 2016. Commonly used psychotherapies in the management of comorbid depression and anxiety include cognitive behavior therapy (CBT), self-guided internet-delivered cognitive behavior therapy (iCBT), acceptance and commitment Therapy (ACT), mindfulness based cognitive therapy (MBCT), metacognitive therapy (MCT), supportive psychotherapy (SP), problem-solving therapy (PST), and interpersonal psychotherapy (IPT).Patients with chronic forms of depression should be offered tailored psychotherapeutic treatments. Findings from a recent meta-analysis suggest that Weitzetal.[2]when comparing effect sizes, psychotherapy for depression is almost as effective at reducing comorbid anxiety symptoms as it is at reducing depressive symptoms with moderate to large effect sizes for anxiety symptoms (g=0.52;NNT=3.50) and depression (g=0.63;NNT=2.82) at outcome. Follow-up assessments also reveal a small lasting effect up to 1 year after baseline assessment (g=0.27) Weitz et al.[2].
Metacognitive therapy for emotional disorders Wells [1] aims to enhance executive control over thinking and attention by changing patterns of preservative self-focused thinking styles and thereby reducing emotional distress and symptoms. The metacognitive model Wells [1] focuses on repetitive styles thinking; particularly; worry and rumination which occur commonly across psychological disorders Wells [1]. Worry and rumination are maintained by positive and negative Metacognitive beliefs Wells[1].A central concept in MCT is the cognitive attentional syndrome(CAS) consisting of three elements: (a) Preservativethinking in the form of worry and rumination,(b) focusing attention on sources of threatperceptions, and (c) maladaptive coping behaviors that backfire (avoidance, thought suppression).Metacognitive therapy has been found to effective for different disorders like generalized anxiety disorder, obsessive-compulsive disorder Fisher & Wells 2008, social anxiety disorder (SAD), panic disorder, major depressive disorder Normann2014; Wells, Fisher, Myers, Wheatley, Patel & Brewin 2012, and traumatic stress Wells &Sembi 2004; Wells, Wellford, Fraser et al. 2008.
The present study aimed to examine the effect of metacognitive therapy (MCT) in the treatment of an individual diagnosed with major depressive disorder with anxiety features. It was hypothesized that metacognitive therapy will help in reducing rumination & worry leading to an overall reduction in symptoms of depression & anxiety in the present case.
Methods
Design
The present study used a single case A-B design Barlow et al. [3], with a follow-up assessment at one month and 2 months after treatment completion. Before starting the treatment, the patient completed a series of self-report questionnaires in English language administered over a period of 2 sessions lasting about an hour each.Treatment included 10 sessions of metacognitive therapy for depression and anxiety delivered on a weekly basis with each treatment session lasting for up to 1 hour. The treatment followed the Metacognitive Therapy for Depression and Anxiety protocol Wells [1] and was delivered in exactly the same format as described in the manual. Permission to conduct the therapy and use the specific outcome measures was obtained via email from Dr. Adrian Wells. The primary therapist (first author of this paper) was a clinical psychologist and research scholar who had undergone a 2 year training program in psychotherapy. Each session was supervised and discussed with a clinical psychologist and psychotherapist (second author of this paper) with over 41 years of experience and training in psychotherapy. At the end of treatment, the patient was re-assessed the same self-report measures. A follow up assessment was also held after 1 month and 2 months of completion of the therapy. No additional treatment was delivered in the follow-up period. A written informed consent was obtained from the participant before conducting the study.
Participant presenting problems and diagnosis
The participant was a 37 year old married Muslim femalewith a total history of psychiatric illness for 3 years. She had previously been diagnosed with dysthymia, major depressive disorder, Anxiety No’s at various private and state run clinics. At present she reported to the outpatient psychiatry services at the All India Institute of Medical Sciences, New Delhi, India with complaints of feelings of discomfort, anxiety, sadness of mood, increased thoughtfulness, worry over future, decreased self-confidence, and increased sleep since. The patient believed that she was weak and inferior to everyone around her, and felt isolated. She would not be able to work well and felt easily fatigued. She would start experiencing tension & worry when attempting to perform any new task. She reported that she would spend about half of her time in a day in brooding over her mental and physical health. She had sought psychiatric treatment at various private clinics; however, there was no change in her symptoms. She had not enrolled herself under any structured psychological treatment for her condition. The present episode had been for 6 months. She met the diagnostic criteria for F41.2 Mixed anxiety and depressive disorder (ICD-10). She was also prescribed benzodiazepines and SSRIs to help in management of her symptoms. The patient was a graduate homemaker and was well versed in spoken and written English language.
Outcome measures
A detailed interview was held with the patient by an experienced psychiatrist to establish the diagnosis. Beck Depression Inventory II (BDI-II) Beck et al.[4] and Beck anxiety Inventory (BAI) Beck et al.[4] were used to assess the levels of depression and anxiety in the patient. Anxious thoughts inventory (AnTi) Wells [1] and Rumination response scale (RRS) Nolen-Hoeksema 1991were used to assess the content of worry and rumination that the patient was frequently engaged in. Metacognitive questionnaire-30 (MCQ-30) Wells [1] was used to assess the nature of meta-cognitive beliefs. Positive beliefs about Rumination scale (PBRS) Papageorgiou & Wells, 2001and Negative beliefs about Rumination scale (NBRS) Papageorgiou, Wells & Meina, 2004 were used to assess the positive and negative metacognitive beliefs held by the patient. All the scales are self-report measures available for use in English language. Permissions to use these assessment scales were obtained from the publishers via email.
The patient was assessed on 4 occasions across the treatment and follow up. Baseline assessments were carried out in 2 sessions before beginning the MCT treatment. Post-treatment assessment was carried out after 10 sessions of MCT to assess the immediate benefits using the same measures. Follow up assessment was carried out at two points in time-at one month and two months of completion of the therapy sessions.
Procedure
Treatment
The patient received 10 individual 1 hour therapy sessions of metacognitive therapy using the MCT manual for depression and anxiety. The overall outline of the sessions is as follows:
A. Psycho-education & generation of individual case formulation
B. Introduction of Attention Training Technique (ATT) exercises
C. Introduction of Detached mindfulness (DM) exercises
D. Introduction of Rumination & Worry Postponement exercises
E. Modification of negative metacognitive beliefs
F. Modification of positive metacognitive beliefs
G. Modification of threat monitoring
H. Addressing maladaptive coping styles
I. Developing new plans for processing
J. Relapse prevention
Data analysis
The study data was analyzed by monitoring percentage changes in the patient’s scores obtained on BDI-II and BAI administered across baseline, the post-treatment and at one month and two month follow-up. Changes in scores obtained on the MCQ-30, PBRS, NBRS, AnTi and RRS were also observed across baseline, the posttreatment and at one month and two month follow-up. Scores were graphically represented along the various points of assessment.
Clinically significant change
A clinically significant change was defined as a 30-40% reduction in symptoms on BDI-II and BAI at post-treatment assessment National Co morbidity Survey, 1994.
Results
The patient’s score on the BDI-II and BAI at baseline, posttreatment and follow-up is illustrated in (Figure 1). At baseline, the patient had obtained a score of 38 on BDI-II indicating severe depressive symptoms. She obtained a score of 30 in BAI indicating severe anxiety. Following treatment using the MCT module, the patient’s scores dropped to 14 on BDI-II suggestive of mild depressive features and 7 on BAI indicating mild anxiety. These changes were maintained at one month and two months follow up. After one month of completion of MCT therapy, patient obtained a score of 14 on BDI-II indicating mild depressive features and a score of 10 on BAI suggesting minimal anxiety. At two monthfollow- up assessment, the patient obtained a score of 13 on BDI-II and a score of 10 on BAI. Considering the criterion for ‘clinically significant change’ used in the present study NCS 1994 the patient obtained about 38% reduction in symptoms on the BDI-II and about 36% reduction in symptoms on BAI scales from baseline to post-treatment. Gains from therapy were maintained at one month and two months follow-up assessments (about 38-39% reduction in symptoms compared to baseline on BDI-II, and about 32% reduction in symptoms compared to baseline on BAI).
Figure 1: Scores obtained (y-axis) by Ms T. on BDI-II and BAI across baseline, post-intervention, and one & two months follow up (x-axis).
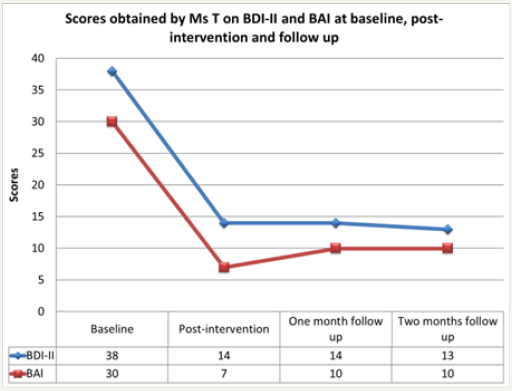
Visual inspection of the graph in Figure 1 also indicates a substantial reduction in symptoms which was maintained at follow up. The scores obtained by the patient at post-treatment and follow up were in the minimal-mild ranges on both, BDI-II, and BAI.The patient’s scores obtained on MCQ-30, PBRS and NBRS were also obtained at baseline assessment, post-therapy assessment, and one and two months follow up assessment. At baseline, the patient obtained a score of 48 on MCQ-30, and a score of 34 on NBRS, and 26 on PBRS. A significant reduction in these scores was observed at post-intervention assessment. After completing therapy, the patient obtained a score of 39 on MCQ-30, 22 on NBRS, and 14 on PBRS. The gains obtained from therapy were maintained at one-month and two months follow up. The patient obtained a score of 35 on MCQ- 30 at the first follow up and a score of 42 on the second follow up. These scores were substantially lower compared to the baseline. An analysis of the scores obtained at follow up assessments on PBRS and NBRS used to assess the positive and negative meta cognitive beliefs of the patient showed similar results. The patient obtained a score of 16 on NBRS and 13 on PBRS at one-month follow-up. She obtained a score of 15 and 12 on NBRS and PBRS respectively, at 2 months follow up.
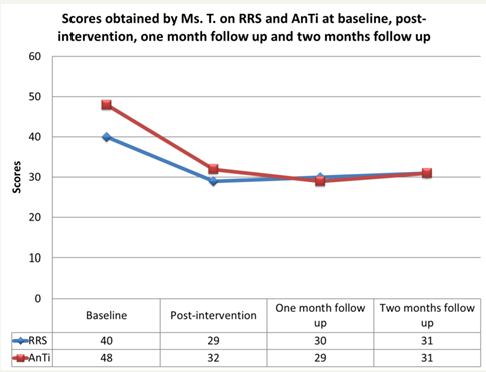
Visual inspection of the graph in Figure 2 also indicates a substantial reduction in symptoms which was maintained at follow up. The patient’s scores obtained on RRS and AnTi were analyzed at baseline assessment, post-therapy assessment, and one and two months follow up assessment. At baseline, the patient obtained a score of 40 on RRS, and a score of 48 on AnTi. After completing the intervention, the patient obtained a score of 29 on RRS, and 32 on AnTi. This shows that there was a significant reduction in the amount of rumination and worry that the patient was engaging in at baseline. This reduction was maintained at one-month and two months follow up. The patient obtained a score of 30 and 31 at the first and second follow-up, respectively on RRS suggesting that her ruminative behavior continued to be lesser as compared to the baseline levels. Similar results were observed in the scores of AnTi. At follow-up assessments, the patient obtained a score of 29 (one month) and 31 (two months) indicating that she was worrying a lot less at follow up when compared with baseline scores. As shown in Figure 3, the participant’s scores on measures assessing worry and rumination dropped substantially across the assessment period.
Figure 2: Scores obtained (y-axis) by Ms T. on MCQ-30, PBRS and NBRS across baseline, post-intervention, and one & two months follow up (x-axis).
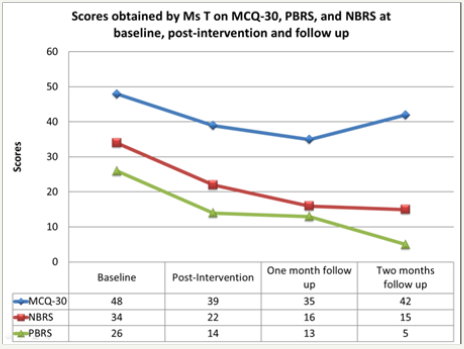
Figure 3: Scores obtained (y-axis) by Ms T. on RRS and AnTi across baseline, post-intervention, and one & two months follow up (x-axis).
Discussion
This case study illustrates that patients with depression and anxiety can be treated using the MCT model of therapy Wells[1]. Meta-cognitive therapy can be used as a helpful transdiagnostic treatment to simultaneously address many emotional problems and deal with common co-morbid conditions. The case ofMsThighlights that multiple emotional problems can arise from excessively engaging in the process of worry and rumination. Worry involves future-centric thinking while rumination involves repeated thinking focusing on past events. Applying disorder-specific approaches based on CBT in this case would have lead to a change in the content of thinking. However, the tendency of the patient to engage in worry and rumination would have remained the same leading to a higher possibility of recurrence of symptoms. MsT. had strongly held positive and negative beliefs about engaging in the process of repetitive thinking. During the sessions, she reported that engaging in repetitive thinking could help her find reasons for her symptoms and arriving at a solution. She also believed that engaging in the process of rumination and worrying may help in reducing her confusion and help sort her problems.
She also reported that thinking in this style had become almost like a habit for her and would maintain the low mood. She also believed that there was some problem with her, that she was not like “normal people” around her. She would keep worrying about her recovery, if medications and treatment will help her in any way, if the health professionals had diagnosed her correctly. She also complained that after hours of thinking in the same style she would try to distract herself by trying to control her thoughts and checking her internal state. However, she would fail every time in trying to control her thoughts and would feel helpless and start worrying further about this uncontrollability. Through MCT, MsT. learned to abandon her old styles of thinking and regulating her emotions. This further lead to a reduction in her perceived distress. Treatment strategies were directed at helping her alter her style of thinking (CAS) instead of challenging her negative thoughts. Modification of negative metacognitive beliefs about worry and rumination helped the patient to confront many of the situations that she was avoiding earlier. Research findings from studies comparing the effectiveness of MCT, as compared to CBT on a sample of treatment-resistant patients Nordahl2009have shown that patients who received MCT displayed significantly greater reductions in anxiety and worry levels than those who received CBT.Wells (1) designates perceived lack of control over thinking as a negative metacognitive belief and challenging this metacognitive belief is a very important mechanism for change and improvement[5-8]. The metacognitive model of treating emotional disorders is based on the Self-Regulatory Executive Function Model (S-REF), which highlights the similarities in maladaptive cognitive processing across different psychological disorders Wells & Matthews 1996; Wells 2009.This model does not focus on a particular diagnosis. It focuses on the common psychological processes that patients engage in that lead to several emotional problems. Thus, it can allow simultaneous treatment of a high level of co morbidities. Given the high rates of co morbidity in clinical practice, there is a high need for designing treatments that do not focus on a particular diagnosis, but are applicable to class of disorders Moses and Barlow, 2006. Such treatments can be extremely cost-effective and applicable to a wide variety of mental health conditions.
Limitations
There are a few in the present study. First, an alternative interpretation of the findings could be the effect of pharmacotherapy and therapeutic alliance. Secondly, although permissions to use the therapy manual Wells [1] were obtained from the original publisher and the sessions were supervised, the primary therapist (first author of this paper) did not obtain any formal training in MCT. Thirdly, better statistical techniques could have been applied to establish the causal relationship between treatment and outcome. In the present study, a percentage change of symptoms on self-report measures was observed over a course of time to examine the outcome of therapy. This methodology is rudimentary and the generalizability of results can be questioned. A better methodology involving pre-post assessments after each session and a mid-therapy assessment could have yielded more comprehensive results. Fourthly, no formal assessment tools measuring treatment and homework compliance were used in this study. Treatment compliance and homework practices are a vital ingredient in therapy. Lastly, since the present study follows a case study design, the reliability and generalizability of results is low.
References
- Wells A (2009) Metacognitive therapy for anxiety and depression. New York: Guilford Press
- Weitz E, Kleiboer A, Van Straten A, & Cuijpers P (2018) The effects of psychotherapy for depression on anxiety symptoms: A meta-analysis. Psychological Medicine, pp. 1-13.
- Barlow DH, Nock MK, Hersen M (2009) Single case experimental designs. MA: Allyn and Bacon Boston, USA.
- Beck AT, Epstein N, Brown G, Steer RA (1988) An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology. 56(6): 893–897.
- World Health Organization (1992) The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines.
- http://www.nice.org.uk/guidance/ng11
- Beck AT, Steer R, Brown G (1995) Beck depression inventory-II manual. San Antonio, USA.
- Beck AT, Steer RA, Brown OK (1996) Beck Depression Inventory Manual 2nd edn. San Antonio, USA.
© 2018 Vandita SharmaandManju Mehta. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






